Outline
Dear Editor,
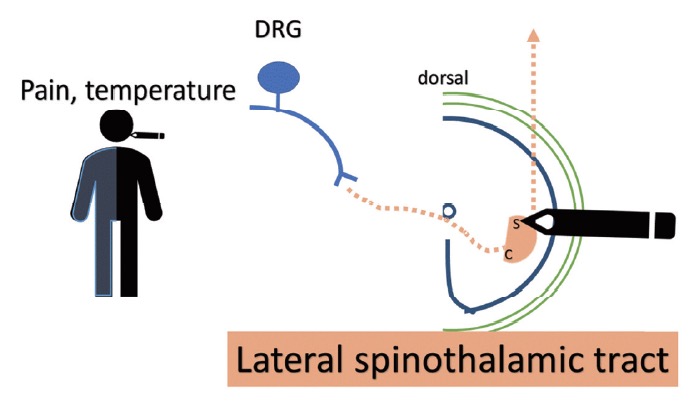
Emerging trends indicate that terminal-stage diseased patients can consider advanced early interventional measures to manage pain and reduce the side effects of opioids.1 Interventional strategies for managing pelvic tumor-associated pain include subarachnoid neurolytic block, which produces effective analgesia but is associated with voiding symptoms.2 As percutaneous cervical cordotomy achieves effective contralateral analgesia below the clavicle by destroying the lateral spinothalamic tract, it is associated with the risk of transient weakness and dysesthesia (Fig. 1).3
Download full-size image
DRG: dorsal root ganglion; S: sacral origin of lateral spinothalamic tract; C: cervical origin of lateral spinothalamic tract.
Download full-size image
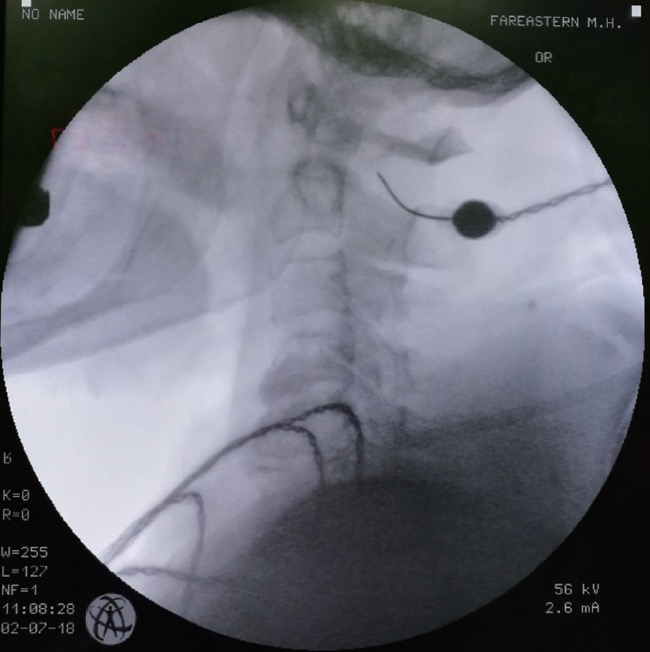
and required more numbers of fentanyl patches (fentanyl 50 µg/hr × 16 patches) in combination with adjuvant oral medicine, which nevertheless, failed to relieve the pain. Suspecting poor prognosis, a lumbar subarachnoid neurolysis by alcohol and percutaneous fluoroscopy-guided cordotomy was suggested during our consultation in May 2018. However, the expertise and knowledge needed for these procedures was lacking among most oncologists. Primarily, a combined meeting was held with the oncology staff, nurses, and the pharmacist introducing the pain interventions, and the relevant information pertaining to the case were disseminated, from basic to clinical evidence. Additional options besides opioid analgesic regimens were explained to the patient’s family. However, her children did not consent to the procedure and therefore, the surgery was postponed twice. The patient initially refused consent, preferring to avoid the voiding and motor function side-effects, but eventually, consented due to debilitating pain. After extensive discussion and shared decision-making, a percutaneous cervical cordotomy was consensually adjudged to be the more precise and tolerable procedure as it was executable in the supine position as opposed to subarachnoid neurolytic blocks. Eventually, a percutaneous cervical cordotomy was performed on July 3, 2018, after the patient’s family provided consent. The entry point on the skin was above the C1–2 intervertebral foramen on the left side with continuous patient feedback of sensory experiences. A radiofrequency (RF) generator with a 22-gauge straight, sharp cannula with a 10-mm electrode tip was used, aided by neurophysiological confirmation via impedance measurement and stimulation, and confirmed functional response of the target. RF thermocoagulation was achieved with sequential lesions at rising temperatures from 50°C to 70°C for 60 s (Fig. 3).4,5
Download full-size image
In the case presented herein, sufficient time and explanation were given to the patient and her family, with eventual achievement of discharge without analgesics, and the patient’s condition remained stable without any deterioration or tumor progression on subsequent follow-up, 8 months after the procedure. We believe that in addition to identifying specific symptoms and appropriate patient selection, an open approach of communication for shared decision-making can improve authenticity and ensure that patients receive utmost holistic care.
References
| 1 |
Ischia S, Luzzani A, Ischia A, Magon F, Toscano D.
Subarachnoid neurolytic block (L5–S1) and unilateral percutaneous cervical cordotomy in the treatment of pain secondary to pelvic malignant disease.
Pain 1984;20:139–149.
|
| 2 |
d’Amours RH, Ferrante FM.
Subarachnoid and epidural neurolysis.
Tech Reg Anesth Pain Manag 1997;1:32–37.
|
| 3 |
Kanpolat Y, Ugur HC, Ayten M, Elhan AH.
Computed tomography-guided percutaneous cordotomy for intractable pain in malignancy.
Neurosurgery 2009;64(3 Suppl):ons187–ons194.
|
| 4 |
Feizerfan A, Antrobus JH.
Role of percutaneous cervical cordotomy in cancer pain management.
BJA Educ 2014;14:23–26.
|
| 5 |
Lake WB, Konrad PE.
Cordotomy procedures for cancer pain: a discussion of surgical procedures and a review of the literature.
World J Surg Proced 2015;5:111–118.
|