Subcutaneous emphysema (ScE) refers to air appearing in subcutaneous tissue. It can be caused by chest trauma, infection, pulmonary complications, or other factors. Although shoulder arthroscopy is generally considered a relatively safe operation that helps surgeons examine or treat the joint, various complications can occur during this operation which force surgeons to use tools such as an air-driven drill. However, ScE and pneumothorax (PnT) have seldom been reported as arising from shoulder arthroscopy surgery. In this paper, we present a case with ScE and PnT appearing due to shoulder arthroscopy surgery and discuss the possible mechanism as well as the management of this rare complication.
A 53-year-old woman suffered from left shoulder pain for months. She had received left shoulder arthroscopic surgery 7 years previously. A preoperative left shoulder magnetic resonance imaging revealed humeral head destruction and glenoid bone destruction with implant loosening. Suspecting the pain was due to loosening of the screw, she was scheduled for arthroscopic screw removal surgery. She had no other medical history except a gastric ulcer, and reported that she did not smoke. A preoperative chest X-ray showed nothing unusual. The patient is average size and build (height/weight: 163 cm/64 kg). In the operation room, general anesthesia was delivered with target controlled infusion. Oral endotracheal tube (ET) was intubated smoothly with traditional Macintosh blade without difficulty, and an ultrasound-guided interscalene block was performed with 10 mL of 0.5% bupivacaine plus 10 mL of 2.0% lidocaine smoothly. The operative position was set as right decubitus, and a sterile wrapping was used to cover her body, including her head and ET. When the operation started, her blood pressure was kept around 100–110 mmHg/60–70 mmHg, and the peak airway pressure was stable at 18–20 mmHg. However, 2 hours later after the surgery began, the surgeon found that the electrically-driven drill had insufficient power to remove the screw, so switched to an air-driven model. Fifteen minutes later, high airway pressure (over 40 mmHg) was detected. The ventilator and ET condition were immediately checked, and ventilation was shifted to manual. The ventilator worked well, and the suction tube was inserted into the ET smoothly, with nothing being sucked from the ET. However, manual ventilation still showed strong resistance and the gauge continued to indicate high airway pressure. The ET and the surrounding tissue were then traced, and subcutaneous crepitus was found over her face and neck. The surgeon then stopped the procedure and removed the sterile wrapping from the patient’s head. A huge area of ScE was found, extending from the patient’s forehead through the chest and abdominal wall to the bilateral leg, in which the condition was found to be dominant. The sound of breathing in the left side was found to have decreased, and a portable chest X-ray (Figure 1) revealed a left-side diaphragm depression. A chest surgeon was immediately consulted and a chest tube was then inserted under his recommendation. Air sprayed out from the chest wall when chest tube was inserted. Fortunately, arterial gas analysis showed only mild CO2 retention without metabolic acidosis, and vital signs were all relatively stable without hypotension. She was then transferred to the intensive care unit and extubated smoothly 2 days later. PnT and the area of ScE improved gradually over the following days (Figure 2), and she was discharged 5 days after the surgery without sequelae.
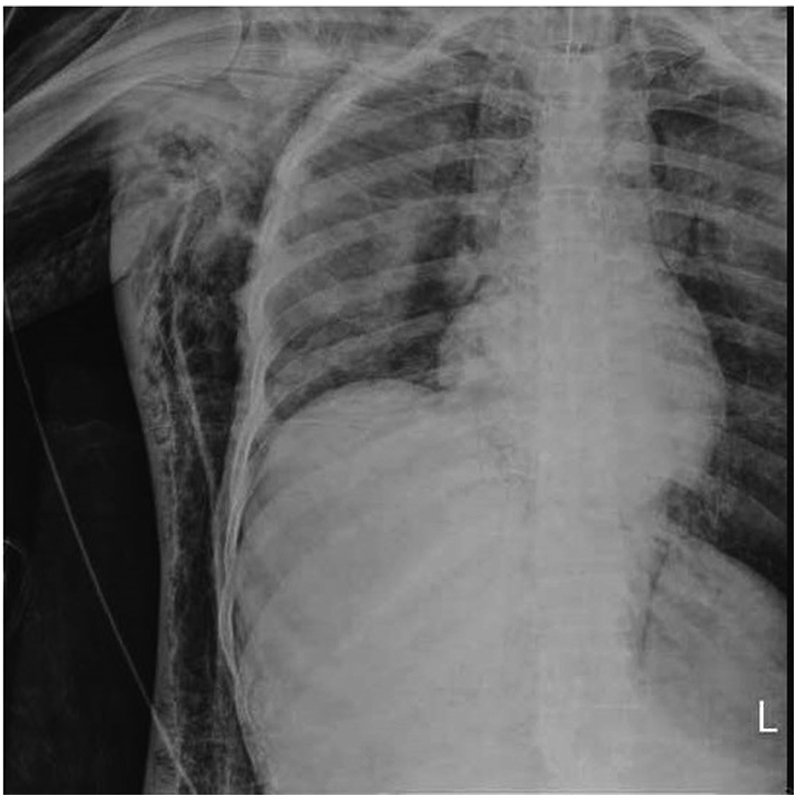
Download full-size image
The left side of the diaphragm is depressed, and subcutaneous emphysema is readily visible. We can see the outline of the bilateral pectoralis major muscles, which indicates air dissecting into the deeper muscles along the fascial planes.

Download full-size image
There is still obvious and extensive subcutaneous emphysema, but much better than in Figure 1. The bilateral diaphragm is back in the normal position.
ScE and pneumomediastinum have been reported as arising from dental procedures after using an air-driven drill.1 This may have resulted from the inappropriate use of dental equipment powered by highly compressed air during tooth extraction. It was thought that the dental equipment disrupted the intraoral barrier, allowing air used by the equipment to leak from the disrupted area to ScE, even reaching the pneumomediastinum,2 but 3 cases have been reported with ScE and PnT during shoulder arthroscopic surgery 25 years ago.3 Those cases were thought to be associated with extravasation of air that may have been drawn in from the lateral portal when the arthroscopic infusion pump and power shaver with suction were turned on.3 Some articles have mentioned ScE and PnT after shoulder arthroscopy.3-5 However, those cases indicated little about the surgical tools used, and are not the same as in the present case, in which there were no problem when using the electric drill with arthroscopic infusion system (pump infusion pressure from 60 to 100 mmHg). It is thought that when the surgeon used the air-driven drill, a large amount of air at high pressure in the shoulder cavity was pushed into the surrounding tissue, causing extensive ScE. The air may then be further extended into other spaces, including the neck and mediastinum, and can even be pushed into the pleura where it can cause unilateral or bilateral PnT. Another possible reason which has been reported for PnT and ScE is the mucosal disruption during ET intubation.6 However, in the present case, there was no evidence of tracheal injury and no paratracheal air on the plain film, so a mucosal break was not likely. Compared with previous case reports, in which the arthroscopic surgery was done in with the patient in an upright position,3 our patient was in a right lateral decubitus position. Whether the surgical position is related to the complications is still unknown. However, the decubitus position may cause more ScE due to the effects of gravity. Positive pressure ventilation is another well-known risk factor of such complications,7 but we maintained peak air pressure at around 18–20 cmH2O, which is far less than the 50 cmH2O which is considered leading to an increased risk of alveolar rupture during mechanical ventilation.8 Concomitant acute respiratory distress syndrome, chronic obstructive lung disease and pneumonia are also well-known risks for such complications,8 but these are not concerns in our case because of the patient’s good pre-operative lung condition, with no ventilation abnormality found before the complication occurred. In most cases involving ScE or PnT problems during the administration of anesthesia, the ventilator setting or patient’s condition is considered to be the cause of the complications. However, these are not factors in our case, which seems to make it unique. Berjano reported that, in 179 arthroscopic shoulder procedures, there was an overall complication rate of 9.49%.9 The complications included infection, excessive bleeding, blood clots, and brachial plexus injury, but no ScE or PnT. Therefore, the incidence of ScE or PnT was very low (under 0.5%) for shoulder arthroscopic surgery. In fact, there has been no actual incidence reported.
Air-driven drills designed for dental procedures use compressed air at 3.5–4.0 kgf/cm2 with the head rotating at 450,000 rpm.10 However, we have been unable to find any articles which discuss the upper limit pressure at which air-driven drills are considered to be safe and prevent such complications. In our case, we did not know the real pressure nor the air amount within the shoulder cavity. However, the extensive ScE complication detected approximately 15-minutes after use, and the high infusion pump pressure strongly suggest that high pressure air-driven drills cannot be used safely in close or semi-close arthroscopic surgery.
We consider the present case to have been fortunate because of the eventually successful complication management without any sequela. We would like to thank the surgeon’s reminding for problems (air-driven drill induced), even though neither of us (surgeon and anesthesiologist) had ever considered that an air-driven drill could cause such damage initially. His caution helped us to make the right diagnosis and treatment. However, we must consider what could have happened if we had failed to diagnose the problem quickly enough, or if the chest tube had not improved patient’s condition. Kahn et al. write of a patient with bilateral PnT with pneumonia and refractory to chest tube insertion.10 They scheduled video-assisted thoracoscopic surgery to remove the patient’s bullae, and applied veno-venous extracorporeal membrane oxygenation (ECMO) due to expected poor oxygenation under one lung ventilation. However, tension PnT were reported to reduce flow in ECMO system.11 Early detection plus alertness via close monitoring are always important. Although PnT and ScE are rare complications in shoulder arthroscopic surgery, this can be life-threatening. Certainly, precise evaluation plus good communication between team members are always the key to success.
We present a rare ScE and PnT complication during shoulder arthroscopic surgery caused by the air-driven drill used. The successful management of such potentially life-threatening complications depends on early detection, quick evaluation, good communication, and the right response. We sincerely hope this case is useful to others in the event of ScE or PnT occurring from shoulder arthroscopic surgery.
Conflicts of Interest
None.
Author Contributions
Wen-Yun Niu helped conceive the structure of the case report and write the manuscript. Yi-An Liao helped conceive the structure of the case report and write the manuscript. Shu-Cheng Liu helped conceive the structure of the case report and write the manuscript. Yen-Chin Liu helped conceive the structure of the case report. Feng-Sheng Lin helped conceive the structure of the case report, and revised the whole body of manuscript.
Financial Disclosures
None.
References
| 1 |
McKenzie WS, Rosenberg M.
Iatrogenic subcutaneous emphysema of dental and surgical origin: a literature review.
J Oral Maxillofac Surg. 2009;67(6):1265–1268.
|
| 2 |
Sekine J, Irie A, Dotsu H, Inokuchi T.
Bilateral pneumothorax with extensive subcutaneous emphysema manifested during third molar surgery. A case report.
Int J Oral Maxillofac Surg. 2000;29(5):355–357.
|
| 3 |
Lee HC, Dewan N, Crosby L.
Subcutaneous emphysema, pneumomediastinum, and potentially life-threatening tension pneumothorax: pulmonary complications from arthroscopic shoulder decompression.
Chest. 1992;101(5):1265–1267.
|
| 4 |
Shariyate MJ, Kachooei AR, Ebrahimzadeh MH.
Massive emphysema and pneumothorax following shoulder arthroscopy under general anaesthesia: a case report.
Arch Bone Jt Surg. 2017;5(6):459–463.
|
| 5 |
Leander-Olsson O, Borglund-Hemph A, Jakobsson JG.
Pneumothorax following shoulder arthroscopy under combined regional and general anaesthesia—a case report.
Int J Surg Case Rep. 2016;24:73–76.
|
| 6 |
Tan CS, Tashkin DP, Sassoon H.
Pneumothorax and subcutaneous emphysema complicating endotracheal intubation.
South Med J. 1984;77(2):253–255.
|
| 7 |
Gammon RB, Shin MS, Buchalter SE.
Pulmonary barotrauma in mechanical ventilation: patterns and risk factors.
Chest. 1992;102(2):568–572.
|
| 8 |
Petersen GW, Baier H.
Incidence of pulmonary barotrauma in a medical ICU.
Crit Care Med. 1983;11(2):67–69.
|
| 9 |
Berjano P.
Complications in arthroscopic shoulder surgery.
Arthroscopy. 1998;14(8):785–788.
|
| 10 |
Kahn J, Müller H, Marte W, et al.
Establishing extracorporeal membrane oxygenation in a university clinic: case series.
J Cardiothorac Vasc Anesth. 2007;21(3):384–387.
|
| 11 |
Odonkor PN, Stansbury L, Garcia JP, Rock P, Deshpande SP, Grigore AM.
Perioperative management of adult surgical patients on extracorporeal membrane oxygenation support.
J Cardiothorac Vasc Anesth. 2013;27(2):329–344.
|