To the Editor,
Opioids are preferred analgesics during neurosurgery for perioperative pain management. However, opioid-induced respiratory impairment in the postoperative period is noted in patients with obstructive sleep apnoea (OSA)1 which can be detrimental to neurosurgical patients. Further, opioid use in patients with difficult airway can pose challenges in maintaining spontaneous respiration during intubation and extubation. We report opioid free analgesia (OFA) technique for intracranial tumour surgery in an obese patient with OSA and known difficult airway.
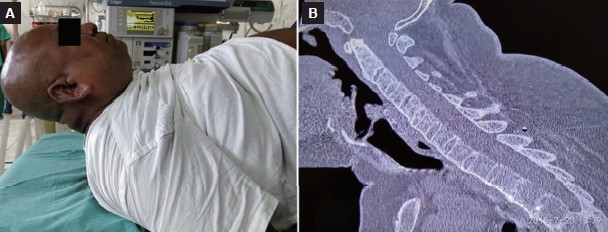
A 53-year-old gentleman with left frontal recurrent glioma was scheduled for urgent craniotomy for rapidly worsening headache and hemiparesis. Previous craniotomy three years earlier was performed awake for failed intubation. On this occasion, both surgeon and patient requested surgery under general anesthesia. On examination, patient was categorized as high-risk for OSA with a score of 6/8 (snoring, hypertension, body mass index 38.3 kg/m2, age 53 years, neck circumference 45.5 cm and male gender) on STOP-BANG questionnaire. He had a fixed-flexed cervical spine from the fusion of all cervical vertebrae (Figure 1) and Mallampati grade 2 airway. We planned oral fiberoptic intubation with dexmedetomidine sedation maintaining spontaneous respiration. Airway anesthesia was achieved with 2 mL each of 2% lignocaine for bilateral superior laryngeal nerve block and trans-tracheal anesthesia, respectively and 10% lignocaine spray provided oro-pharyngeal anesthesia. Dexmedetomidine was administered at 0.75 μg/kg/h for 10 minutes before intubation. Oral fiberoptic intubation the with a 7.5 mm flexo-metallic tube was successful in the first attempt. General anesthesia was maintained with O2/Air/Sevoflurane, intermittent doses of vecuronium, and dexmedetomidine (0.5–1 μg/ kg/h) titrated to Surgical Pleth Index below 50. Scalp block with 20 mL of 0.25% bupivacaine was performed before skull-pin fixation. Patient maintained hemodynamic stability throughout the surgery. At dural closure, phenytoin 600 mg, dexamethasone 8 mg, and paracetamol 1,000 mg were administered. After skin closure, incision site was infiltrated with 10 mL of 0.25% bupivacaine. Following the completion of surgery, patient was extubated without new neurological deficits. There was no postoperative nausea and vomiting (PONV), shivering, respiratory depression/obstruction in postoperative period and pain (numerical rating scale score remained < 4/10 on diclofenac 150 mg/d without any opioid supplementation).
Download full-size image
Opioids are associated with several undesirable adverse effects such as respiratory depression, prolonged sedation, PONV, pruritus, ileus, urinary retention, and hyperalgesia which contribute to morbidity, costs, and delayed discharge. OFA techniques are preferred in patients with morbid obesity, OSA, obstructive lung disease, chronic pain, opioid addiction and bariatric and onco-surgery.2 OFA with dexmedetomidine and scalp block obviated the need for peri-operative opioids and yet provided good analgesia. Dexmedetomidine was better than fentanyl for pain relief for spinal surgeries.3 Similarly, meta-analysis of 11 trials involving 674 neurosurgical patients showed reduced perioperative opioid consumption and pain intensity with intraoperative dexmedetomidine.4 We have recently demonstrated dexmedetomidine analgesia to be non-inferior to fentanyl for craniotomies.5
To conclude, we report the successful use of dexmedetomidine-based OFA for intracranial tumor surgery in an obese patient with OSA and difficult airway. Dexmedetomidine facilitated awake intubation preserving spontaneous respiration both during intubation and extubation in this vulnerable patient.
Author Contributions
Seham: Data collection, first draft; Sangeetha: Review of the manuscript; Sriganesh: Conduct of case, Literature review and final draft.
Conflict of Interest
None.
Funding
This was taken from the patient.
References
| 1 |
Lam KK, Kunder S, Wong J, Doufas AG, Chung F.
Obstructive sleep apnea, pain, and opioids: is the riddle solved?
Curr Opin Anaesthesiol. 2016;29(1):134-140.
|
| 2 |
Sultana A, Torres D, Schumann R.
Special indications for Opioid Free Anaesthesia and Analgesia, patient and procedure related: including obesity, sleep apnoea, chronic obstructive pulmonary disease, complex regional pain syndromes, opioid addiction and cancer surgery.
Best Pract Res Clin Anaesthesiol. 2017;31(4):547-560.
|
| 3 |
Turgut N, Turkmen A, Gökkaya S, Altan A, Hatiboglu MA.
Dexmedetomidine-based versus fentanyl-based total intravenous anesthesia for lumbar laminectomy.
Anestesiol. 2008;74(9):469-474.
|
| 4 |
Liu Y, Liang F, Liu X, Shao X, Jiang N, Gan X.
Dexmedetomidine reduces perioperative opioid consumption and postoperative pain intensity in neurosurgery: a meta-analysis.
J Neurosurg Anesthesiol. 2018;30(2):146-155.
|
| 5 |
Sriganesh K, Syeda S, Shanthanna H, Venkataramaiah S, Palaniswamy SR.
Comparison of intraoperative fentanyl with dexmedetomidine for perioperative analgesia and opioid consumption during craniotomies: a randomised controlled pilot study with non-inferiority design.
Int J Clin Pract. 2019;73(6):e13338.
|