Abstract
Background
Dexmedetomidine has been used by multiple routes in laparoscopic surgeries to attenuate the hemodynamic response. The present study was done to compare the efficacy of dexmedetomidine nebulization with intravenous dexmedetomidine and fentanyl in laparoscopic surgeries under general anesthesia.
Methods
A prospective, double blind study was conducted, and 90 American Society of Anesthesiologists (ASA) I and II patients of either gender between 18–65 years undergoing laparoscopic surgeries under general anesthesia were randomized into three groups. (1) Group N (n = 30) received dexmedetomidine nebulization 1 mcg/kg in 3 mL of 0.9% saline 15 minutes before induction and 10 mL of intravenous 0.9% saline over 10 minutes at the time of induction of anesthesia. (2) Group I (n = 30) received 0.9% saline nebulization 3 mL and intravenous dexmedetomidine 1 mcg/kg in 10 mL of 0.9% saline. (3) Group F (n = 30) received 0.9% saline nebulization 3 mL and intravenous fentanyl 2 mcg/kg in 10mL of 0.9% saline. Heart rate, blood pressure, propofol requirement, and opioid consumption were monitored throughout surgery and for 1 hour in post-operative period. Statistical analysis was done by using analysis of variance test, chi-square test.
Results
Suppression of hemodynamic response following intubation and pneumoperitoneum by dexmedetomidine nebulization was compared to intravenous dexmedetomidine and fentanyl. Opioid requirement was significantly lower in dexmedetomidine group than fentanyl group (
Conclusions
In laparoscopic surgeries, nebulized dexmedetomidine suppresses hemodynamic response when compared to intravenous dexmedetomidine along with dose sparing effect of opioid and propofol.
Keywords
dexmedetomidine, hemodynamics, laparoscopy, nebulization, opioid sparing
Introduction
Laparoscopic surgeries have increased in recent days because of multiple benefits like magnified operating field, less cosmetic scar and less post-operative pain along with reduced duration of hospital stay, morbidity, and mortality.1,2 Pneumoperitoneum associated with laparoscopy and anesthetic maneuvers like laryngoscopy and intubation has been associated with severe hemodynamic disturbances like tachycardia, hypertension, increased systemic and pulmonary vascular resistance predisposing cardiac ischemia.3-6 Multiple drugs like opioids, beta-blockers, calcium channel blockers, and local anesthetics have been used to suppress the hemodynamic response with variable results.7-13
Dexmedetomidine is an α-2 adrenergic agonist that has been proven to attenuate the hemodynamic response to intubation and pneumoperitoneum along with dose sparing effect on opioids and propofol.14,15 It has been used in multiple routes such as intravenous, intramuscular, oral, nasal, or intrathecal routes.16-22 There are limited studies on nebulized dexmedetomidine15,23-25 for suppression of hemodynamic response to intubation and pneumoperitoneum in comparison with intravenous dexmedetomidine and fentanyl. This study aims to not only compare the effect of dexmedetomidine nebulization (1 mcg/kg) on the suppression of hemodynamic response to intubation and pneumoperitoneum with intravenous dexmedetomidine and fentanyl but also assess opioid and propofol requirement during surgery.
Methods
A prospective, randomized, double blind comparative study was conducted after Institutional Ethical Committee approval, Clinical Trial Registry-India (CTRI) registration (CTRI/2019/11021920, registered on 7/11/2019).
The aim of the study was to not only compare the effect of dexmedetomidine nebulization on the suppression of hemodynamic response to intubation and pneumoperitoneum with intravenous dexmedetomidine and fentanyl but also assess opioid and propofol requirement.
Ninety patients of either gender aged between 18–65 years with American Society of Anesthesiologists (ASA) physical status I and II scheduled for laparoscopic surgeries under general anesthesia were included in the study. Exclusion criteria included patients refusing to participate in the study, obese individuals, difficult airway, uncontrolled hypertension, diabetes, cardio-respiratory disorders, neuro-psychiatric disorders, hepatic or renal dysfunction, pregnant or lactating mothers, alcoholic, patients on opioids, sedatives, beta-blockers, and allergic to study drug. Equipment, drugs for resuscitation and general anesthesia, were kept ready. Pre-anesthetic evaluation was done, and written informed consent was obtained before the surgery. Patients were randomly divided into three groups of 30 each using computer generated randomization software, and group allocation was concealed by sealed opaque envelopes which was opened in the preoperative room. Randomization and preparation of study drug was done by one anesthesiologist not involved in this study, and outcome measures were observed by the other independent anesthesiologist. Patient and assessor of outcome measures were blinded to group allocation.
(1) Group N: nebulized with dexmedetomidine 1 mcg/kg in 3mL of 0.9% saline 15 minutes before shifting the patients to operation room and 10 mL of 0.9% saline intravenous over 10 minutes at the time of induction.
(2) Group I: nebulized with 3 mL of 0.9% saline 15 minutes before shifting the patientsto operation room and dexmedetomidine 1 mcg/kg in 10mL of 0.9% saline intravenous over 10 minutes at the time of induction.
(3) Group F: nebulized with 3 mL of 0.9% saline 15 minutes before shifting the patients to operation room and fentanyl 2 mcg/kg in 10 mL of 0.9% saline intravenous over 10 minutes at the time of induction.
The patients were given glycopyrrolate 5 mcg/kg and midazolam 0.02 mg/kg, pre-oxygenated with 100% oxygen for 3 minutes and then induced with propofol 30 mg/10s till loss of verbal response. Intubation by experienced anesthetist using appropriate sized endotracheal tube was facilitated with 0.1 mg/kg vecuronium and maintained with oxygen, air, isoflurane, and intermittent doses of vecuronium 0.02 mg/kg. Neuromuscular block was reversed with neostigmine 0.05 mg/kg and glycopyrolate 10 mcg/kg, and the patients were extubated after meeting the extubation criteria. Post-operative patients were monitored for 1 hour in the recovery room.
Heart rate (HR) and non-invasive systolic blood pressure (SBP) changes were noted before nebulization, after nebulization, immediately after induction, after intubation for 5minutes, post-pneumoperitoneum every 15 minutes, post extubation, and in post-operative room for 1 hour.
Additional doses of fentanyl (25–50 mcg) and propofol (20–30 mg) were given if HR and SBP increased more than 20%during surgery, and total consumption of fentanyl and propofol was noted.
Statistical Methods
Pilot study was conducted. Sample size was estimated by using mean HR at 5 minutes following intubation. To detect at least 20% of difference in HR among study groups at 95% confidence interval, 90% power, sample size of 26 was obtained. Assuming 10% dropout, we recruited 30 patients in each group.
The statistical software namely SPSS 22.0 (IBM Corp, Armonk, NY, USA) and R environment ver.3.2.2 were used for the analysis of the data. Microsoft word and excel have been used to generate graphs, tables, etc. Analysis of variance has been used to find the significance of study parameters between three or more groups of patients. Post hoc Tukey test has been used to find the group wise significance. Chi-square/Fisher’s exact test has been used to find the significance of study parameters on categorical scale between two or more groups. Non-parametric setting for qualitative data analysis and Fisher’s exact test was used when cell samples were very small.
Results
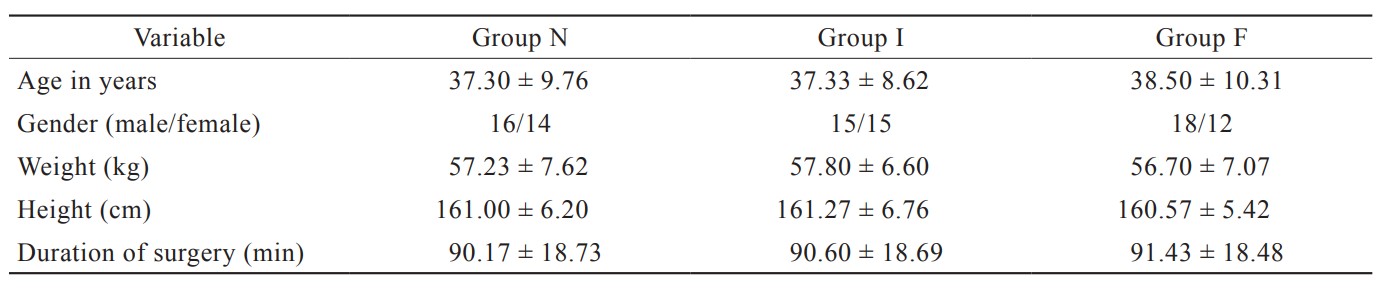
Ninety patients were recruited and received intended treatment without any dropouts or exclusions. The demographic data and the duration of surgery were comparable in all three groups (Table 1).
Download full-size image
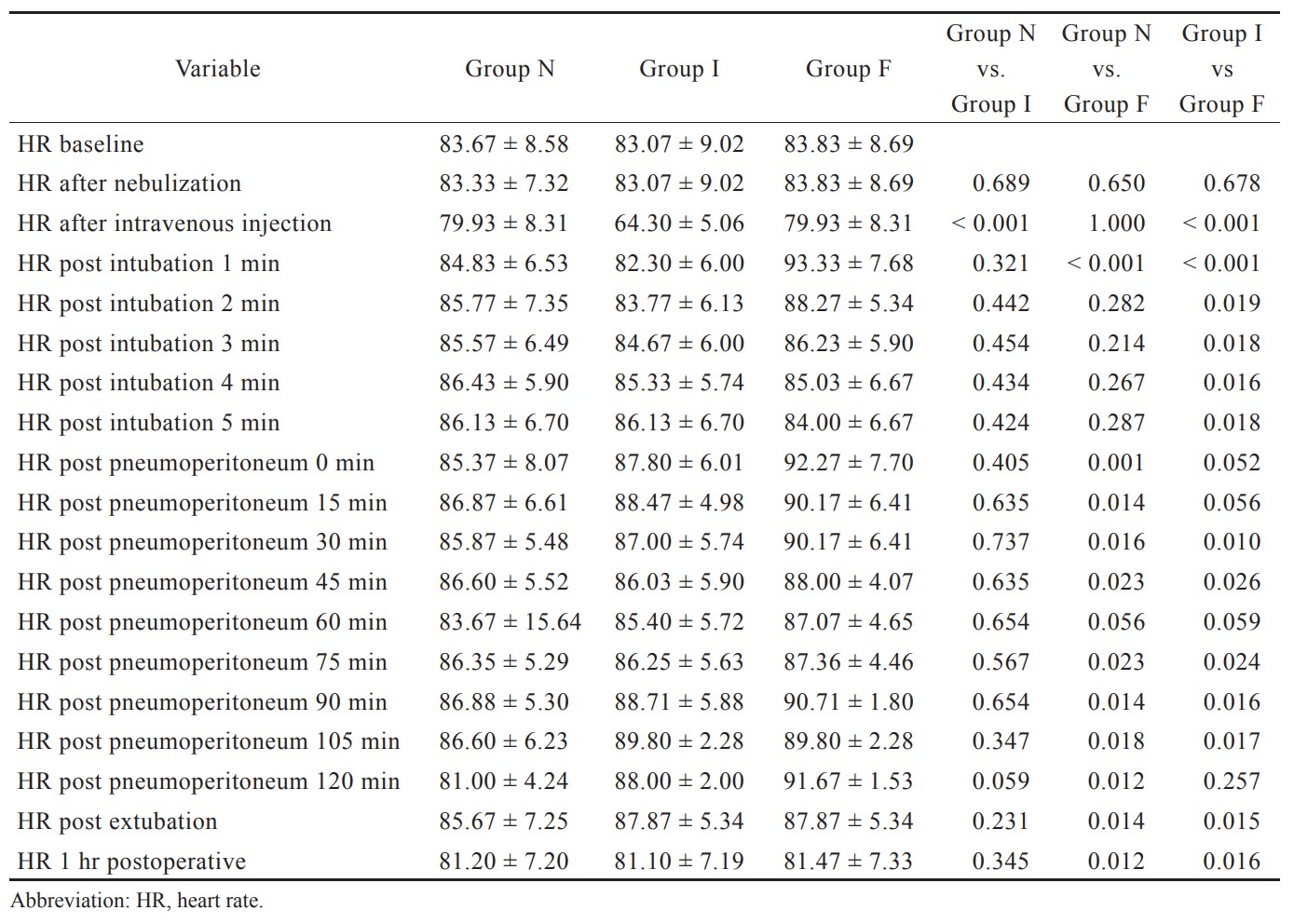
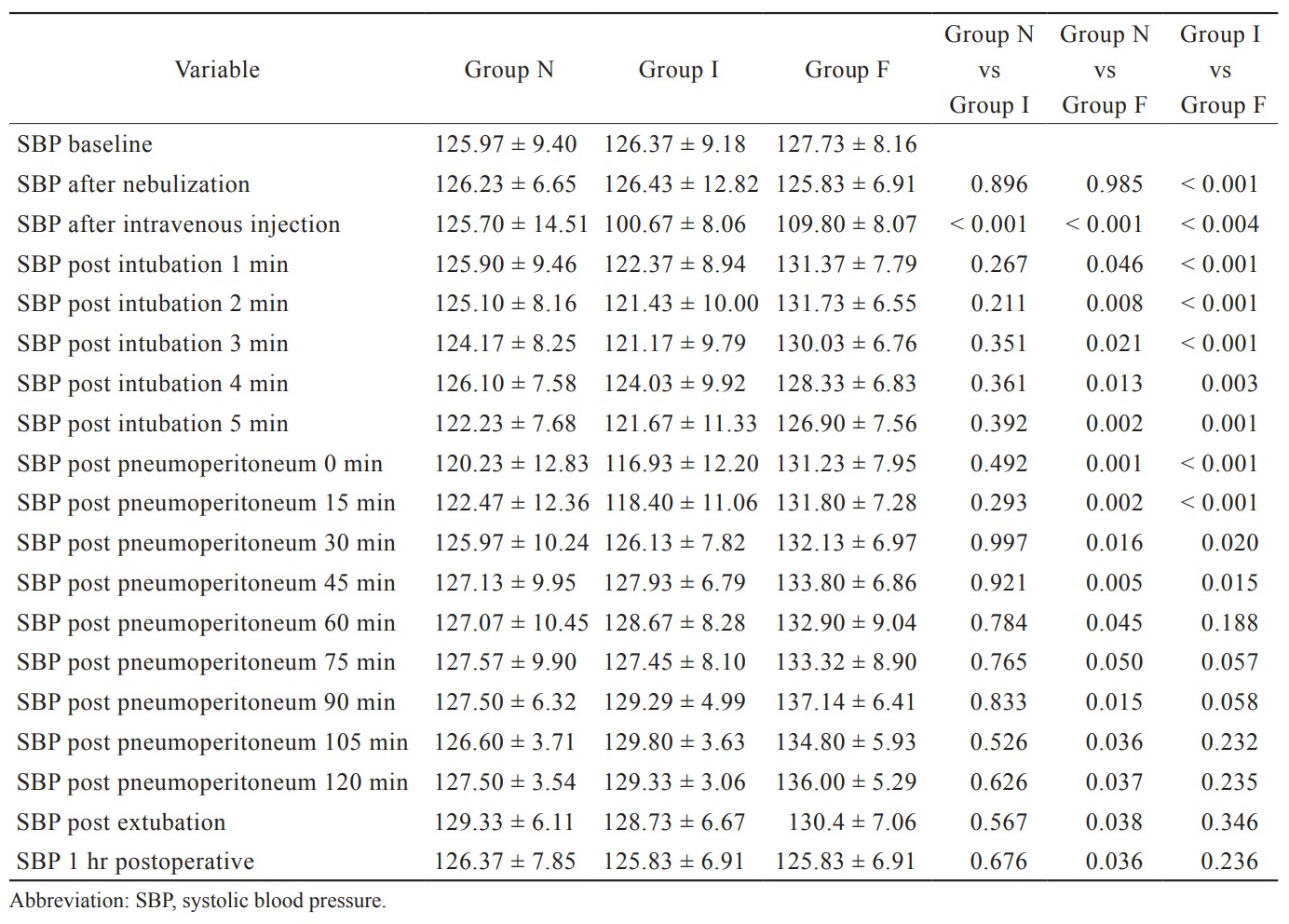
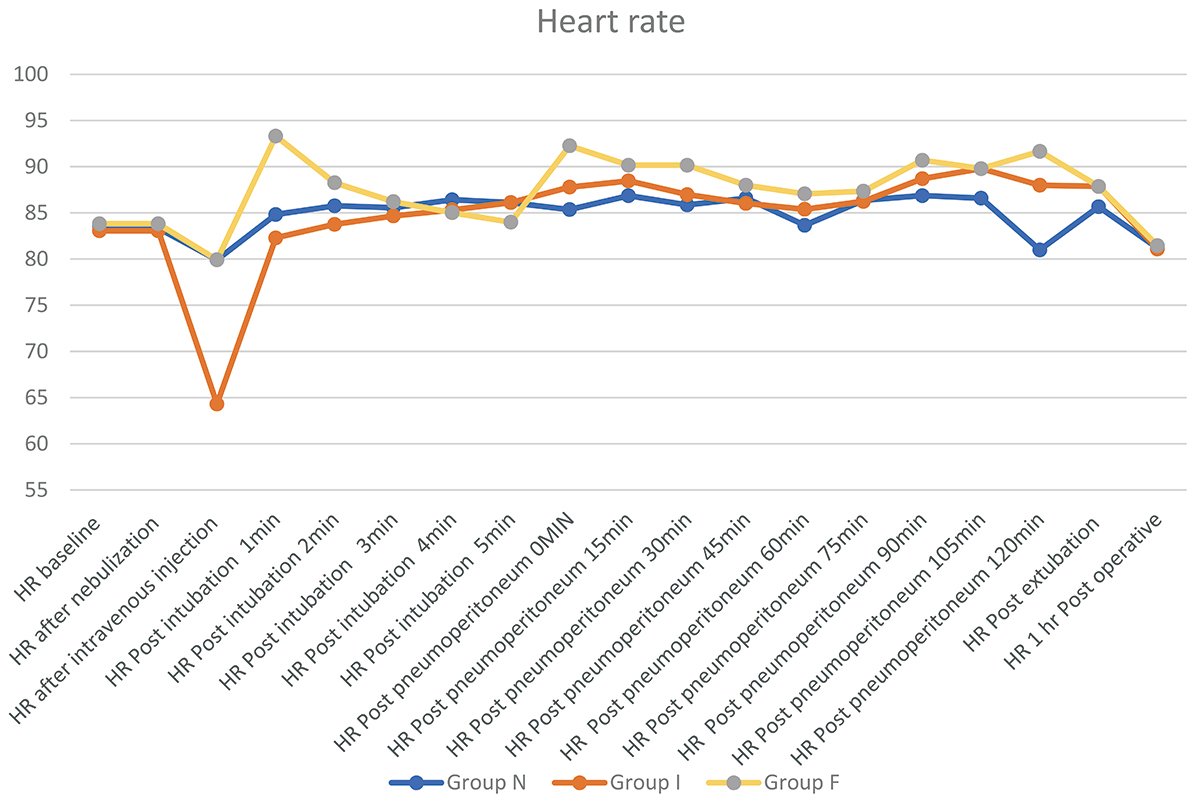
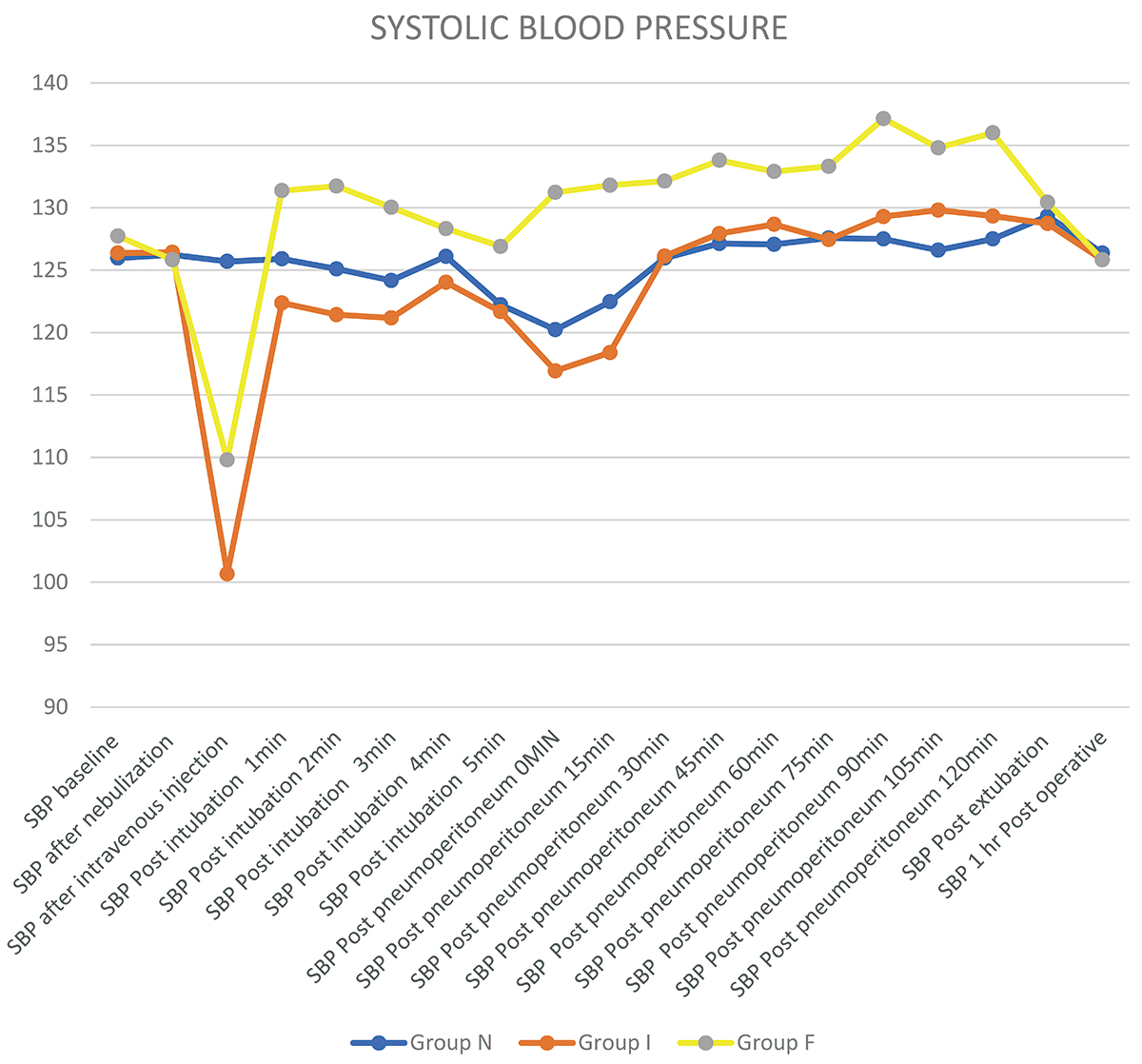
HR and blood pressure dropped significantly after administration of intravenous dexmedetomidine when compared to nebulized dexmedetomidine and intravenous fentanyl. Suppression of HR and blood pressure after intubation and pneumoperitoneum with nebulized dexmedetomidine was comparable to intravenous dexmedetomidine and fentanyl (Tables 2 and 3, Figures 1 and 2).
Download full-size image
Download full-size image
Download full-size image
Download full-size image
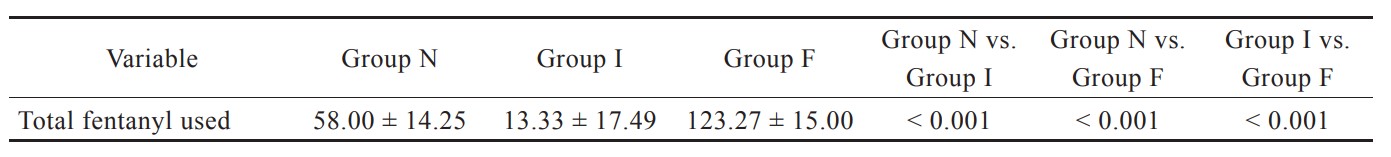
Fentanyl requirement was recorded throughout the surgery and was significantly lower with both intravenous and nebulized dexmedetomidine group than fentanyl group. Intravenous dexmedetomidine group required less fentanyl when compared to nebulized dexmedetomidine (Table 4).
Download full-size image
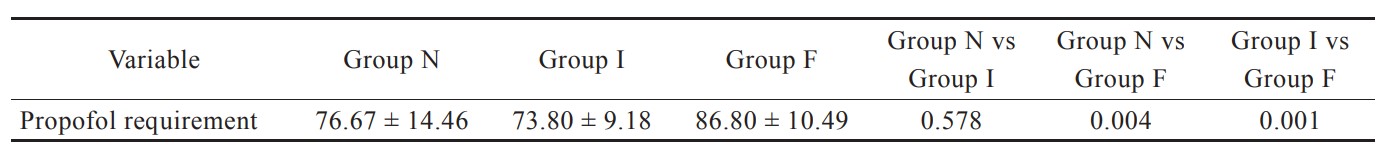
Propofol consumption was significantly lower in both nebulized and intravenous dexmedetomidine group when compared to intravenous fentanyl group (Table 5).
Download full-size image
No adverse events related to dexmedetomidine nebulization administration such as intra-operative or post-operative hypotension, or bradycardia were noted.
Discussion
In our study, we observed that dexmedetomidine provides significantly better suppression of hemodynamic response to intubation and pneumoperitoneum in laparoscopic surgeries. Suppression of response with nebulized dexmedetomidine was compared to intravenous dexmedetomidine. Significant drop in blood pressure was seen after the administration of intravenous dexmedetomidine. There was significant opioid sparing effect in both nebulized and intravenous dexmedetomidine groups which was highly significant in the intravenous group. Significant dose sparing effect on induction dose of propofol was seen with both nebulized and intravenous dexmedetomidine when compared to intravenous fentanyl.
Laparoscopic surgeries under general anesthesia are associated with unique hemodynamic changes in the form of increased systemic vascular resistance, hypertension, and tachycardia which requires increasing the depth of anesthesia and sometimes the use of vasodilators. Fentanyl is a synthetic opioid commonly used as pre-medication for analgesia to potentiate the hypnotic effect of propofol and to suppress hemodynamic responses; however, there is incomplete suppression of hemodynamic responses. Dexmedetomidine, a centrally acting α-2 adrenergic agonist, decreases sympathetic nervous activity, and suppresses hemodynamic response to intubation and pneumoperitoneum.26 Onset of intravenous dexmedetomidine is within 5 minutes and the duration of action is up to 2 hours with single dose as per the literature. Dexmedetomidine nebulization onset of action is within 15 minutes; however, the duration of action was assumed to be longer than intravenous route because of sustained release of the drug from the respiratory mucosa into systemic circulation.
Kataria et al.15 studied the efficacy of dexmedetomidine and fentanyl on pressor response and pneumoperitoneum in laparoscopic cholecystectomy and found that the control of HR and mean arterial pressure was better with intravenous dexmedetomidine. Misra et al.25 studied the effect of preoperative dexmedetomidine nebulization on the hemodynamic response to laryngoscopy and intubation and observed that nebulized dexmedetomidine at 1 µg/kg attenuated the increase in heart rate but not SBP following laryngoscopy and reduced the intraoperative anesthetic and analgesic consumption. Ours was a unique study which compared both intravenous and nebulized dexmedetomidine with intravenous fentanyl on hemodynamic suppression to intubation and pneumoperitoneum, and we found that nebulized dexmedetomidine had significant suppression of hemodynamic response similar to intravenous dexmedetomidine when compared to intravenous fentanyl without any hypotension or bradycardia. Previous studies have demonstrated high incidence of hypotension and bradycardia with intravenous dexmedetomidine.27,28 Our study has shown incidence of hypotension and bradycardia immediately after the administration of dexmedetomidine is significantly lower with nebulized dexmedetomidine than intravenous dexmedetomidine.
Intravenous dexmedetomidine has shown to reduce intra-operative opioid and anesthetic consumption in previous studies.19,27-29 In the present study, nebulized dexmedetomidine reduced the induction dose of propofol and fentanyl requirement when compared to intravenous dexmedetomidine.
Limitation of our study is that only single dose administration of intravenous and nebulized dexmedetomidine was studied. Effects of different doses on hemodynamics cannot be commented. Also, effect of nebulized dexmedetomidine on postoperative outcomes like analgesia, postoperative nausea and vomiting, sore throat, and duration of action was not studied.
Conclusions
Dexmedetomidine nebulization 1 mcg/kg administered before induction of anesthesia significantly attenuates hemodynamic response to intubation and pneumoperitoneum when compared to intravenous fentanyl along with dose sparing effect on fentanyl and propofol requirement. Nebulized dexmedetomidine can be used as an alternative to intravenous dexmedetomidine without any adverse effects.
Further studies on different doses and other outcomes like postoperative analgesia, sore throat, postoperative relief of nausea and vomiting are required to ratify widespread use of nebulized dexmedetomidine.
Conflict of Interest
There are no conflicts of interest.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial Support and Sponsorship
Nil.
References
| 1 |
Rao LN.
A clinical study of dexmedetomidine for maintenance during general anaesthesia for laparoscopic surgeries.
Int J Med Sci Clin Invent. 2015;2(1):681-687.
|
| 2 |
Srivastava VK, Agrawal S, Gautam SKS, Ahmed M, Sharma S, Kumar R.
Comparative evaluation of esmolol and dexmedetomidine for attenuation of sympathomimetic response to laryngoscopy and intubation in neurosurgical patients.
J Anaesthesiol Clin Pharmacol. 2015;31(2):186-190.
|
| 3 |
Chraemmer-Jørgensen B, Hertel S, Strøm J, Høilund-Carlsen PF, Bjerre-Jepsen K.
Catecholamine response to laryngoscopy and intubation.
Anaesthesia. 1992;47(9):750-756.
|
| 4 |
Manne GR, Upadhyay MR, Swadia V.
Effects of low dose dexmedetomidine infusion on haemodynamic stress response, sedation and post-operative analgesia requirement in patients undergoing laparoscopic cholecystectomy.
Indian J Anaesth. 2014;58(6):726-731.
|
| 5 |
O’Leary E, Hubbard K, Tormey W, Cunningham AJ.
Laparoscopic cholecystectomy: haemodynamic and neuroendocrine responses after pneumoperitoneum and changes in position.
Br J Anaesth. 1996;76(5):640-644.
|
| 6 |
Bhattacharjee DP, Nayek SK, Dawn S, Bandopadhyay G, Gupta K.
Effects of dexmedetomidine in haemodynamics in patients undergoing laparoscopic cholecystectomy—a comparative study.
J Anaesthesiol Clin Pharmacol. 2010;26(1):45-48.
|
| 7 |
Victory RA, Gajraj NM, Pace NA, Ostman LP, White PF.
Nebulized bupivacaine attenuates the heart rate response following tracheal intubation.
J Clin Anesth. 1995;7(1):9-13.
|
| 8 |
Singh H, Vichitvejpaisal P, Gaines GY, White PF.
Comparative effects of lidocaine, esmolol, and nitroglycerin in modifying the hemodynamic response to laryngoscopy and intubation.
J Clin Anesth. 1995;7(1):5-8.
|
| 9 |
Inada E, Cullen DJ, Nemeskal AR, Teplick R.
Effect of labetalol or lidocaine on the hemodynamic response to intubation: a controlled randomized double-blind study.
J Clin Anesth. 1989;1(3):207-213.
|
| 10 |
Ghignone M, Quintin L, Duke PC, Kehler CH, Calvillo O.
Effects of clonidine on narcotic requirements and hemodynamic response during induction of fentanyl anesthesia and endotracheal intubation.
Anesthesiology. 1986;64(1):36-42.
|
| 11 |
Charuluxananan S, Kyokong O, Somboonviboon W, Balmongkon B, Chaisomboonpan S.
Nicardipine versus lidocaine for attenuating the cardiovascular response to endotracheal intubation.
J Anesth. 2000;14(2):77-81.
|
| 12 |
Kutlesic MS, Kutlesic RM, Mostic-Ilic T.
Attenuation of cardiovascular stress response to endotracheal intubation by the use of remifentanil in patients undergoing Cesarean delivery.
J Anesth. 2016;30(2):274-283.
|
| 13 |
Min JH, Chai HS, Kim YH, et al.
Attenuation of hemodynamic responses to laryngoscopy and tracheal intubation during rapid sequence induction: remifentanil vs.
Minerva Anestesiol. 2010;76(3):188-192.
|
| 14 |
Afonso J, Reis F.
Dexmedetomidine: current role in anesthesia and intensive care.
Rev Bras Anestesiol. 2012;62(1):118-133.
|
| 15 |
Kataria AP, Attri JP, Kashyap R, Mahajan L.
Efficacy of dexmedetomidine and fentanyl on pressor response and pneumoperitoneum in laparoscopic cholecystectomy.
Anesth Essays Res. 2016;10(3):446-450.
|
| 16 |
El-Shmaa NS, El-Baradey GF.
The efficacy of labetalol vs dexmedetomidine for attenuation of hemodynamic stress response to laryngoscopy and endotracheal intubation.
J Clin Anesth. 2016;31:267-273.
|
| 17 |
Kunisawa T, Nagata O, Nagashima M, et al.
Dexmedetomidine suppresses the decrease in blood pressure during anesthetic induction and blunts the cardiovascular response to tracheal intubation.
J Clin Anesth. 2009;21(3):194-199.
|
| 18 |
Kakkar A, Tyagi A, Nabi N, Sethi AK, Verma UC.
Comparision of clonidine and dexmedetomidine for attenuation of laryngoscopy and intubation response—a randomized controlled trial.
J Clin Anesth. 2016;33:283-288.
|
| 19 |
Scheinin B, Lindgren L, Randell T, Scheinin H, Scheinin M.
Dexmedetomidine attenuates sympathoadrenal responses to tracheal intubation and reduces the need for thiopentone and peroperative fentanyl.
Br J Anaesth. 1992;68(2):126-131.
|
| 20 |
Kumari K, Gombar S, Kapoor D, Sandhu HS.
Clinical study to evaluate the role of preoperative dexmedetomidine in attenuation of hemodynamic response to direct laryngoscopy and tracheal intubation.
Acta Anaesthesiol Taiwan. 2015;53(4):123-130.
|
| 21 |
Dogru K, Arik T, Yildiz K, Bicer C, Madenoglu H, Boyaci A.
The effectiveness of intramuscular dexmedetomidine on hemodynamic responses during tracheal intubation and anesthesia induction of hypertensive patients: a randomized, double-blind, placebo-controlled study.
Curr Ther Res Clin Exp. 2007;68(5):292-302.
|
| 22 |
Niyogi S, Biswas A, Chakraborty I, Chakraborty S, Acharjee A.
Attenuation of haemodynamic responses to laryngoscopy and endotracheal intubation with dexmedetomidine: a comparison between intravenous and intranasal route.
Indian J Anaesth. 2019;63(11):915-923.
|
| 23 |
Zanaty OM, El Metainy SA.
A comparative evaluation of nebulized dexmedetomidine, nebulized ketamine, and their combination as premedication for outpatient pediatric dental surgery.
Anesth Analg. 2015;121(1):167-171.
|
| 24 |
Abdel-Ghaffar HS, Kamal SM, El Sherif FA, Mohamed SA.
Comparison of nebulised dexmedetomidine, ketamine, or midazolam for premedication in preschool children undergoing bone marrow biopsy.
Br J Anaesth. 2018;121(2):445-452.
|
| 25 |
Misra S, Behera BK, Mitra JK, Sahoo AK, Jena SS, Srinivasan A.
Effect of preoperative dexmedetomidine nebulization on the hemodynamic response to laryngoscopy and intubation: a randomized control trial.
Korean J Anesthesiol. 2021;74(2):150-157.
|
| 26 |
Basar H, Akpinar S, Doganci N, et al.
The effects of preanesthetic, single-dose dexmedetomidine on induction, hemodynamic, and cardiovascular parameters.
J Clin Anesth. 2008;20(6):431-436.
|
| 27 |
Lawrence CJ, De Lange S.
Effects of a single pre-operative dexmedetomidine dose on isoflurane requirements and peri-operative haemodynamic stability.
Anaesthesia. 1997;52(8):736-744.
|
| 28 |
Mahajan L, Kaur M, Gupta R, Aujla KS, Singh A, Kaur A.
Attenuation of the pressor responses to laryngoscopy and endotracheal intubation with intravenous dexmedetomidine versus magnesium sulphate under bispectral index-controlled anaesthesia: a placebo-controlled prospective randomised trial.
Indian J Anaesth. 2018;62(5):337-343.
|
| 29 |
Yildiz M, Tavlan A, Tuncer S, Reisli R, Yosunkaya A, Otelcioglu S.
Effect of dexmedetomidine on haemodynamic responses to laryngoscopy and intubation: perioperative haemodynamics and anaesthetic requirements.
Drugs R D. 2006;7(1):43-52.
|