Abstract
Background
The quality of postanesthesia recovery is among the important issues of general anesthesia that affect the patient’s ability to perform daily activities. This study hence aimed to investigate the effects of general anesthesia with isoflurane and propofol on the quality of recovery (QoR) in patients undergoing an abdominal hysterectomy.
Methods
This clinical trial was conducted on 80 women aged 30–65 years who visited Ayatollah Rouhani Hospital of Babol for an elective abdominal hysterectomy in 2020. Based on a randomized block design (4 blocks of 20), the participants were equally assigned to two groups of propofol (P) and isoflurane (I). The QoR-15 scale was employed to measure the QoR in terms of physical and mental dimensions, as primary outcomes, and duration of anesthesia, duration of surgery, response time, quality of extubation, changes in blood pressure and heart rate, length of stay in the recovery unit, Aldrete score, pain score, and prevalence of postoperative nausea and vomiting (PONV), as secondary outcomes.
Results
The results showed that there was no significant difference between the two groups in terms of postoperative physical and mental changes (
Conclusions
Propofol outperformed isoflurane in terms of response time, quality of extubation, prevalence of PONV, and increase in blood pressure. In addition, the physical and mental QoR on the second night after surgery was higher in patients anesthetized with propofol compared to those anesthetized with isoflurane.
Keywords
general anesthesia, hysterectomy, isoflurane, propofol, recovery of function
Introduction
Hysterectomy, which is the most common gynecological surgery after cesarean section, is done in three ways including radical, abdominal, and vaginal.1 A hysterectomy is performed under general anesthesia or local anesthesia (spinal and epidural).2
General anesthesia is associated with complications such as aspiration of gastric contents, respiratory failure, nausea and vomiting, and postoperative shivering,1 whereas complications of spinal anesthesia include headache, hypotension, unwanted drug injection, neurological injury, hematoma, and infection.2
An abdominal hysterectomy is usually done under general anesthesia because of the greater patient satisfaction with it and since it provides more time for the surgical team to perform the surgery.3 Postoperative nausea and vomiting (PONV) is a common complication in patients undergoing surgical procedures, especially abdominal surgeries or hysterectomies, as its prevalence is about 50%–79% in obstetric and gynecological surgeries.4,5 It is hence very important to choose an anesthesia method that produces more rapid emergence from anesthesia in order to upgrade postoperative recovery.6,7
Propofol and isoflurane (an inhalational anesthetic) are two commonly used substances in modern general anesthesia8,9 that cause anti-nausea effects10,11 and reduce the level of consciousness or alertness.12 Propofol takes about 2 minutes and sometimes 5 to 10 minutes to produce anesthetic effects.13
Some of the complications of propofol are decreased heart rate, bradycardia, hypotension, burning sensation at the injection site, and apnea.14 Among other serious complications of this anesthetic are infection, addiction, and propofol infusion syndrome.15 Propofol causes anticonvulsant and anti-nausea effects and results in very quick recovery.16,17
As a substance used to induce and maintain anesthesia,18 isoflurane reduces pain sensitivity and relaxes muscles.19 Isoflurane is also known as an inhalational anesthetic that binds to gamma-aminobutyric acid (GABA) receptors to enhance inhibition of synapse transmission in postsynaptic neurons.20 Isoflurane takes a very short time to exert its anesthetic effects.21
Although the observation that propofol reduces pain after surgery was serendipitous, there are clear mechanistic reasons to explain this phenomenon. Propofol exerts a positive modulation of the inhibitory function of the neurotransmitter GABA through GABAA (GABA type A) receptors, and this is believed to mediate most of its anesthetic effect.18
Isoflurane has been found to attenuate the changes in arterial blood pressure, heart rate, and efferent autonomic nerve activity.
Postoperative outcomes are very complicated and depend on the residual effects of anesthetics, effects of surgical trauma, and the patient’s preoperative health status.22
Different anesthetics used for surgical procedures may have different effects on hemodynamics, respiratory system, postoperative pain intensity, and PONV23 that can delay discharge from hospital.24 The use of opioids in anesthesia can lead to better control of postoperative pain, reduce the need for anesthetics, and shorten the recovery time after stopping medication.25
Most studies comparing these two anesthetics (propofol and isoflurane) have mainly emphasized their pharmacological effects on the patient’s hemodynamic stability and respiratory system, postoperative pain control, and on other items separately.26-28
Propofol is well suited for continuous infusion techniques, as its context-sensitive half-life increases by only 20 to 30 minutes with infusion durations from 2 to 8 hours. High clearance and redistribution after a long infusion allow a rapid return to consciousness.27
Recent studies have extensively investigated the patient’s quality of recovery (QoR) and postoperative health status by using many QoR measurement tools.29 The QoR-15 measured the patient’s health status in the two domains of physical well-being (10 items) and mental well-being (5 items), totally 15 items. Each items were scored based on an 11-point numerical rating scale (for positive items, 0 = “none of the time” to 10 = “all of the time”; for negative items the scoring was reversed; maximum score 150).30
The main objective of this study is to compare the effects of propofol and isoflurane on the quality of postoperative recovery using the QoR-15, which is the short form of the QoR-40 questionnaire.30
The QoR-15 measured the patient’s health status in the two domains of physical well-being (10 items) and mental well-being (5 items). The items were scored based on an 11-point Likert scale (from 0: never to 10: always for positive items and from 0: always to 10: never for negative items). The maximum score obtainable on this measure was 150.11
The secondary objectives of this study were to measure the effects of propofol and isoflurane on postoperative blood pressure, pain, nausea and vomiting, extubation conditions, and anesthesia duration and also to evaluate the effects of these changes on the overall postoperative recovery.
Methods
The study sample in this clinical trial consisted of patients aged 30–65 years categorized under American Society of Anesthesiologists (ASA) classes I and II in terms of physical health status who were candidates for elective abdominal hysterectomy in Ayatollah Rouhani Medical Center of Babol University of Medical Sciences. The patients aged under 30 or over 65 years, categorized under an ASA class other than I and II, with a body mass index higher than 30 kg/m3,
with a difficult airway, and afflicted with mental disorders or drug addiction were excluded from the study. Based on the study conducted by Lee et al.9, the sample size was determined to be 80.
By using a randomized block design (4 blocks of 20), the participants were equally assigned to two groups of 40 each: the propofol (P) and the isoflurane (I) groups. All participants were briefed on the research procedure before obtaining their informed consent and standard monitoring using a pulse oximeter, a non-invasive sphygmomanometer, and electrocardiography was carried out for them. After 1 mg of midazolam and 1 mg/kg of lidocaine were administered, anesthesia induction and endotracheal intubation (No. 7) were done by injecting 1 µg/kg of fentanyl, 2 mg/kg propofol, and 0.5 mg/kg atracurium. Mechanical ventilation was provided for all participants under CO2 exhalation control with a current volume of 6–8 mL/kg and a respiratory rate of 12 breaths per minute.
To maintain anesthetic effects, participants in the propofol group received 100 µg/kg/min of propofol and 1 µg/kg/hour of fentanyl, and those in the isoflurane group were administered 1% isoflurane and 1 µg/kg/hour of fentanyl. Participants in both groups received an equal ratio of oxygen and N2O. In cases of more than a 20% increase in the baseline arterial blood pressure, the participants received 25–50 µg of fentanyl. Fifteen minutes before the end of the surgery, participants in both groups were administered 4 mg of ondansetron and 0.005 mg/kg of morphine. In addition, the effect of muscle relaxants was neutralized by injecting 0.02 mg/kg of atropine and 0.04 mg/kg of neostigmine. After the participants were fully conscious and had enough spontaneous breathing, they were extubated and transferred to the postanesthesia care unit (PACU). When the Aldrete score of participants reached 9 or greater, they were discharged from the PACU.
The QoR was measured by completing the QoR-15 the day before surgery (as the baseline) and on the first and second days after surgery (postoperation day 1 [POD1], postoperatuion day 2 [POD2]). Hemodynamic signs of participants (systolic blood pressure, diastolic blood pressure, and heart rate) were measured every 5 minutes before and during the induction of anesthesia, during surgery, before extubation, and after extubation. Other secondary outcomes such as quality of extubation, the duration of time between cessation of anesthetics and patients’ response to verbal commands (response time), PONV, and length of stay in the PACU were investigated. The QoR-15 measured the QoR after surgery and anesthesia by asking 15 questions in the two domains of physical well-being (10 items) and mental well-being (5 items). The items were scored based on an 11-point Likert scale (from 0: never to 10: always for positive items and from 0: always to 10: never for negative items). The maximum obtainable score was 150. Based on a 5-point scale, the quality of extubation was measured by incidence of cough immediately after extubation. This scale was as follows: 1 = no coughs, 2 = gentle extubation, one or two coughs, 3 = moderate coughing (3 or 4 times), 4 = severe and difficult coughing (5 to 10 times), and 5 = poor and very annoying extubation (laryngospasm and coughing more than 10 times). Postoperative pain was also measured by using an 11-point scale. The participants with a pain score of 5 or higher were administered 50 µg of fentanyl, and those with vomiting received 10 mg of metoclopramide.
The data were carefully collected and statistically analyzed using the independent
Results
All 80 participants in this study were female. Their mean age and weight were 47.56 ± 6.13 years and 68.78 ± 8.07 kg in the isoflurane group and 49.22 ± 8.95 years and 70.39 ± 10.03 kg in the propofol group. Therefore, there were no significant differences between the two groups with regard to age and weight (
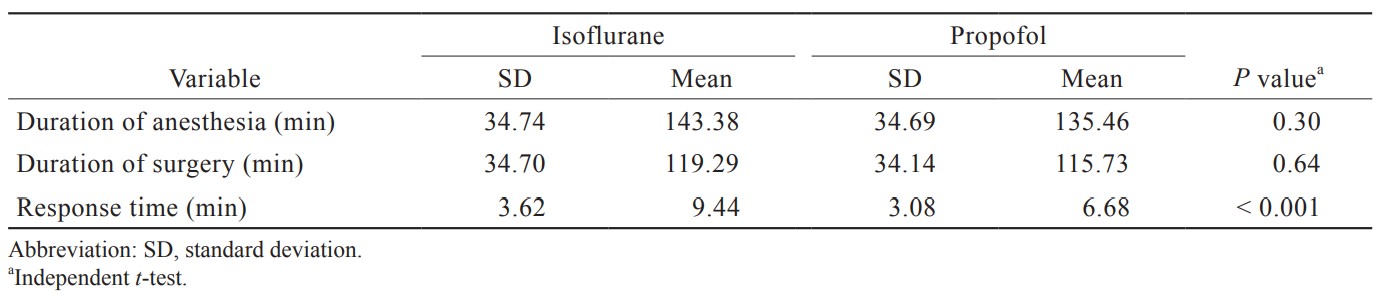
The data presented in Table 1 revealed that the effect of time was statistically significant (
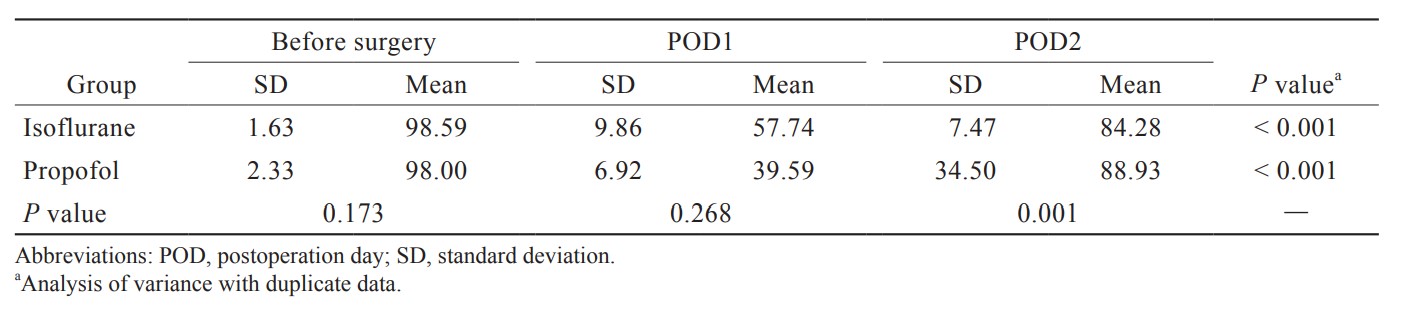
Download full-size image
Table 2 showed that the effect of time was statistically significant as the mean QoR in terms of mental well-being significantly changed over time (
Download full-size image
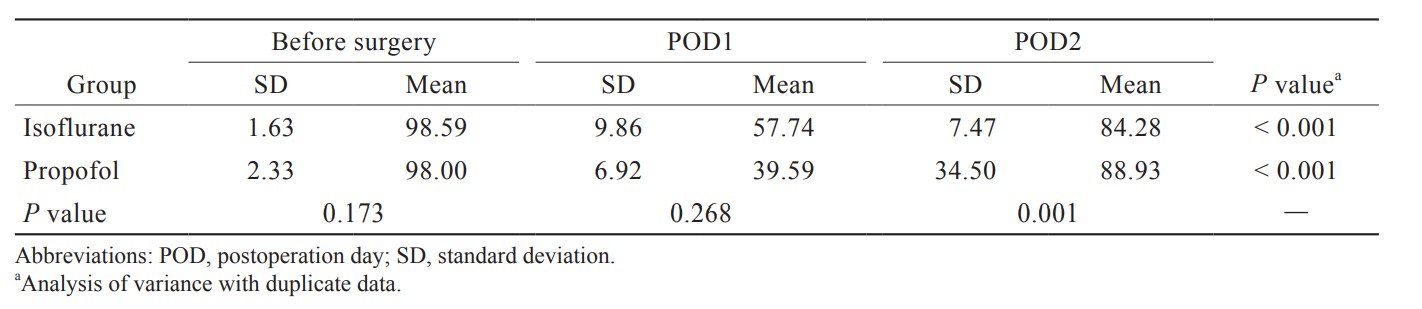
According to Table 3, the effect of time was statistically significant as the mean QoR in terms of physical well-being significantly changed over time (
Download full-size image
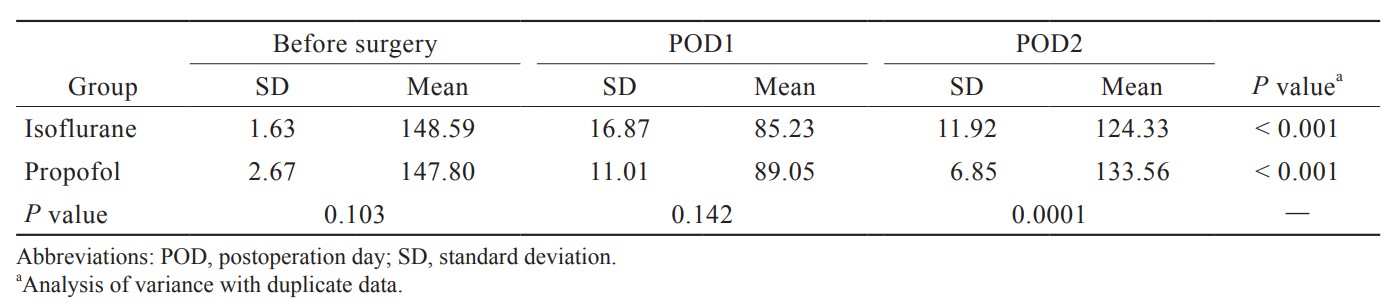
The results indicated that there was no significant difference between the two groups in the duration of anesthesia (
Download full-size image
It should be noted that the half-times for propofol is 1 to 8 minutes and the half-times for isoflurane is less than 5 minutes. The drugs were stopped at the end of the surgery.
The results showed 60% and 40% of participants in the isoflurane group had no coughs and coughed 1 or 2 times, whereas 85% and 15% of participants in the propofol group had no coughs and coughed 1 or 2 times. Therefore, the number of participants’ cough in the isoflurane group is significantly more than those in the propofol group (
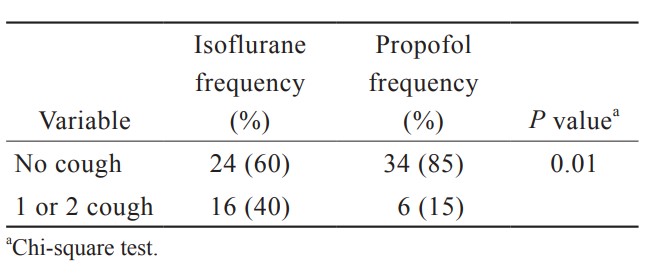
Download full-size image
The data in Table 6 reveal that there was no significant difference between the two groups in terms of length of stay in the PACU (
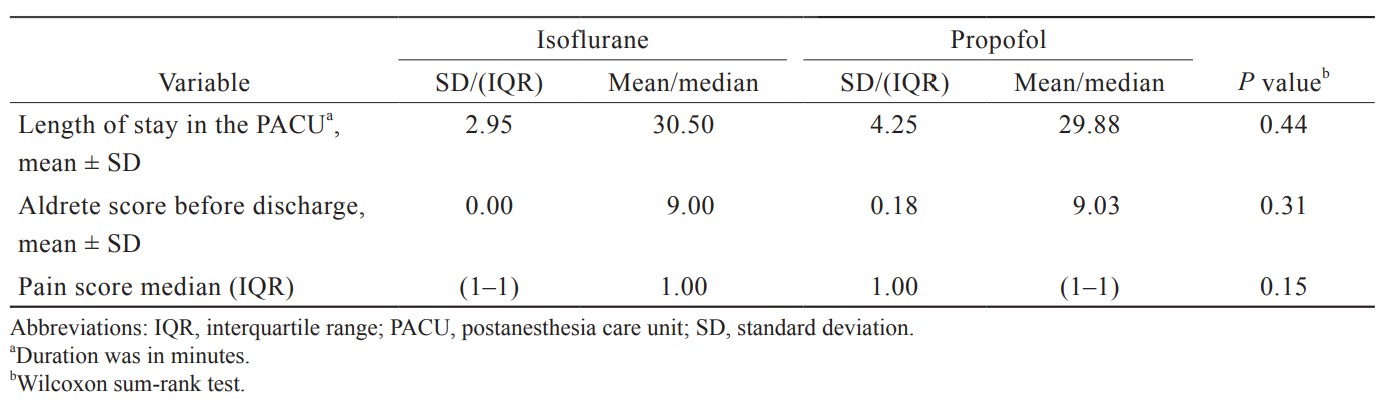
Download full-size image
Table 7 also showed that the prevalence of nausea and vomiting was significantly lower in the propofol group (2.4%) than in the isoflurane group (29.3%) (
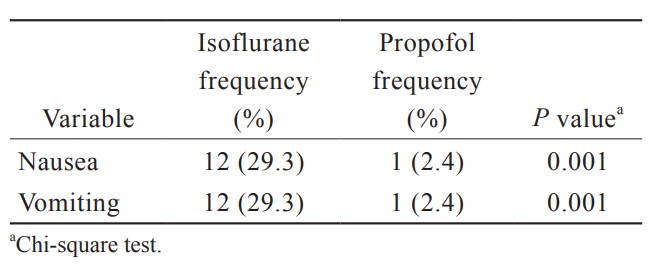
Download full-size image
Discussion
The results showed that the mean quality of postoperative recovery in terms of mental, physical, and overall well-being significantly changed over time in both groups. There was no significant difference between the two groups in this regard on the night before surgery and on the first night after surgery, whereas the QoR was higher in the propofol group on the second night after surgery.
Lee et al.9 in 2015 studied the QoR after anesthesia with propofol-remifentanil and desflurane and reported that the QoR was significantly higher after anesthesia with propofol-remifentanil. Although they used the QoR-40 to measure the QoR in patients undergoing thyroidectomy, their findings were consistent with those of this study.
Another study31 in 2008 investigated the QoR after anesthesia with isoflurane and propofol in 60 patients undergoing laparoscopic cholecystectomy. The results showed that the QoR (easier extubation and shorter eye-opening time) was significantly higher in patients anesthetized with propofol.
A systematic review and meta-analysis of 229 clinical trials that compared the effects of propofol with those of other inhalational anesthetics in maintaining general anesthesia revealed that patient satisfaction and the quality of respiratory recovery and tracheal extubation were higher after anesthesia with propofol.8
This study indicated that there was no significant difference between the isoflurane and propofol groups in the duration of anesthesia and the duration of surgical procedure, but the response time was significantly shorter in the propofol group. In addition, the quality of tracheal extubation was higher in the propofol group.
In this research, there was no significant difference between the two groups in length of stay in the PACU, Aldrete score before discharge, and pain score. By contrast, a systematic review showed that the mean score of pain after intubation and the quality of respiratory recovery and tracheal extubation were higher under anesthesia with propofol compared to other inhalational anesthetics.8 This discrepancy can be attributed to the larger sample size and strengths of systematic review and meta-analysis compared to clinical trials with much smaller sample sizes.
Khalid et al.31 reported that, compared to the other anesthetics, propofol provided improvement (extubation and eye-opening time) significantly faster immediately after surgery. Most patients in the propofol group received the maximum Aldrete score at different times up to 30 minutes. These results are not consistent with the findings of the present study. This study had a different type of surgery and the characteristics of patients from our study.
In this study, the blood pressure of participants in the propofol group was significantly lower than that of the isoflurane group (
Consistent with the results of this study, Schraag et al.8 reported that anesthesia with propofol, compared to other inhalational anesthetics, significantly reduced the risk of PONV.
Khalid et al.31 also proved that anesthesia with propofol considerably reduced the prevalence of PONV in the early and late periods. In addition, the need for antiemetic drugs during the first 24 hours was significantly less in the propofol group.
In another study conducted to compare the postoperative complications of total intravenous anesthesia (TIVA) and inhalational anesthetics, it was shown that TIVA anesthetics were more effective than inhalational anesthetics in preventing PONV.25
There are two limitations or considerations to this study. First, the sample size may not be sufficient to compare each postoperative outcome, including nausea/vomiting and pain score between groups. Lastly, because we enrolled patients undergoing abdominal hysterectomy, our study results should be generalized with caution to those who receive other types of surgery.
Conclusions
The QoR using propofol was higher only on the second day after surgery compared to isoflurane, but there was no significant difference between the two groups in this regard on the following days. However, anesthesia with propofol led to shorter response time, higher quality of extubation, lower prevalence of PONV, and an increase blood pressure of patients.
Conflict of Interest
None declared.
Acknowledgments
The authors thank the Clinical Research Development Unit of Rouhani Hospital.
References
| 1 | |
| 2 |
Borgstedt L, Blobner M, Musiol M, et al.
Neurotoxicity of different amyloid beta subspecies in mice and their interaction with isoflurane anaesthesia.
PLoS One. 2020;15(12):e0242989.
|
| 3 |
Massicotte L, Chalaoui KD, Beaulieu D, Roy JD, Bissonnette F.
Comparison of spinal anesthesia with general anesthesia on morphine requirement after abdominal hysterectomy.
Acta Anaesthesiol Scand. 2009;53(5):641-647.
|
| 4 |
Sekhavat L, Davar R, Behdad S.
Efficacy of prophylactic dexamethasone in prevention of postoperative nausea and vomiting.
J Epidemiol Glob Health. 2015;5(2):175-179.
|
| 5 |
Achuthan S, Singh I, Varthya SB, Srinivasan A, Chakrabarti A, Hota D.
Gabapentin prophylaxis for postoperative nausea and vomiting in abdominal surgeries: a quantitative analysis of evidence from randomized controlled clinical trials.
Br J Anaesth. 2015;114(4):588-597.
|
| 6 |
Lavand’homme P, De Kock M.
The use of intraoperative epidural or spinal analgesia modulates postoperative hyperalgesia and reduces residual pain after major abdominal surgery.
Acta Anaesthesiol Belg. 2006;57(4):373-379.
|
| 7 |
Kroon UB, Rådström M, Hjelthe C, Dahlin C, Kroon L.
Fast-track hysterectomy: a randomised, controlled study.
Eur J Obstet Gynecol Reprod Biol. 2010;151(2):203-207.
|
| 8 | |
| 9 |
Lee WK, Kim MS, Kang SW, Kim S, Lee JR.
Type of anaesthesia and patient quality of recovery: a randomized trial comparing propofol–remifentanil total i.
Br J Anaesth. 2015;114(4):663-668.
|
| 10 |
Vuyk J, Sitsen E, Reekers M.
Intravenous anesthetics.
|
| 11 |
Krasowski MD, Koltchine VV, Rick CE, Ye Q, Finn SE, Harrison NL.
Propofol and other intravenous anesthetics have sites of action on the γ-aminobutyric acid type A receptor distinct from that for isoflurane.
Mol Pharmacol. 1998;53(3):530-538.
|
| 12 |
Kahraman S, Zup SL, McCarthy MM, Fiskum G.
GABAergic mechanism of propofol toxicity in immature neurons.
J Neurosurg Anesthesiol. 2008;20(4):233-240.
|
| 13 |
McKeage K, Perry CM.
Propofol: a review of its use in intensive care sedation of adults.
CNS Drugs. 2003;17(4):235-272.
|
| 14 |
Marik PE.
Propofol: therapeutic indications and side-effects.
Curr Pharm Des. 2004;10(29):3639-3649.
|
| 15 |
Schneider U, Rada D, Rollnik JD, Passie T, Emrich HM.
Propofol dependency after treatment of tension headache.
Addict Biol. 2001;6(3):263-265.
|
| 16 |
Irwin MG, Chung CKE, Ip KY, Wiles MD.
Influence of propofol‐based total intravenous anaesthesia on peri‐operative outcome measures: a narrative review.
Anaesthesia. 2020;75(Suppl 1):e90-e100.
|
| 17 |
Kodama M, Higuchi H, Ishii-Maruhama M, et al.
Multi-drug therapy for epilepsy influenced bispectral index after a bolus propofol administration without affecting propofol’s pharmacokinetics: a prospective cohort study.
Sci Rep. 2020;10(1):1578.
|
| 18 |
Şen ZB, Kiliç N.
General anesthesia in geriatric dogs with propofol-isoflurane, propofol-sevoflurane, alphaxalone-isoflurane, alphaxalone-sevoflurane and their comparison of biochemical, hemodynamic and cardiopulmonary effects.
Acta Sci Vet. 2018;46(1):1519.
|
| 19 |
Seagard JL, Elegbe EO, Hopp FA, et al.
Effects of isoflurane on the baroreceptor reflex.
Anesthesiology. 1983;59(6):511-520.
|
| 20 |
Sonner JM, Zhang Y, Stabernack C, Abaigar W, Xing Y, Laster MJ.
GABA (A) receptor blockade antagonizes the immobilizing action of propofol but not ketamine or isoflurane in a dose-related manner.
Anesth Analg. 2003;96(3):706-712.
|
| 21 |
Guedes A, Knych H, Tucker L, et al.
Pharmacokinetics and clinical effects of xylazine and dexmedetomidine in horses recovering from isoflurane anesthesia.
J Vet Pharmacol Ther. 2020;43(4):369-376.
|
| 22 |
Inai Y, Nomura Y, Takarada T, Hanada N, Wada N.
Risk factors for postoperative pneumonia according to examination findings before surgery under general anesthesia.
Clin Oral Investig. 2020;24(10):3577-3585.
|
| 23 |
Moharram EE, El Attar AM, Kamel MA.
The impact of anesthesia on hemodynamic and volume changes in operative hysteroscopy: a bioimpedance randomized study.
J Clin Anesth. 2017;38:59-67.
|
| 24 |
Herrera FJ, Wong J, Chung F.
A systematic review of postoperative recovery outcomes measurements after ambulatory surgery.
Anesth Analg. 2007;105(1):63-69.
|
| 25 |
Miller TE, Gan TJ.
Total intravenous anesthesia and anesthetic outcomes.
J Cardiothorac Vasc Anesth. 2015;29(Suppl 1):S11-S5.
|
| 26 |
Glass PS, Bloom M, Kearse L, Rosow C, Sebel P, Manberg P.
Bispectral analysis measures sedation and memory effects of propofol, midazolam, isoflurane, and alfentanil in healthy volunteers.
Anesthesiology. 1997;86(4):836-847.
|
| 27 |
Smith I, Ding Y, White PF.
Comparison of induction, maintenance, and recovery characteristics of sevoflurane-N2O and propofol-sevoflurane-N2O with propofol-isoflurane-N2O anesthesia.
Anesth Analg. 1992;74(2):253-259.
|
| 28 |
Abe K, Shimizu T, Takashina M, Shiozaki H, Yoshiya I.
The effects of propofol, isoflurane, and sevoflurane on oxygenation and shunt fraction during one-lung ventilation.
Anesth Analg. 1998;87(5):1164-1169.
|
| 29 |
Stark PA, Myles PS, Burke JA.
Development and psychometric evaluation of a postoperative quality of recovery score: the QoR-15.
Anesthesiology. 2013;118(6):1332-1340.
|
| 30 |
Chazapis M, Walker EMK, Rooms MA, Kamming D, Moonesinghe SR.
Measuring quality of recovery-15 after day case surgery.
Br J Anaesth. 2016;116(2):241-248.
|
| 31 |
Khalid A, Siddiqui SZ, Aftab S, Sabbar S, Haider S.
Recovery profile—a comparison of isoflurane and propofol anesthesia for laparoscopic cholecystectomy.
J Coll Physicians Surg Pak. 2008;18(6):329-333.
|