Abstract
To the Editor,
Existing evidence supports that intra-operative use of processed electroencephalography (EEG) monitor may guide anesthesia delivery to prevent adverse neurocognitive effects, minimize the risk of intraoperative awareness, and administer anesthetics precisely.1 Acute changes of the density spectral array (DSA) and low indices of bispectral index (BIS) can detect cerebral hypoperfusion or ischemia during general anesthesia (GA).1,2 Here, we present a case experiencing hypovolemic shock and hypoxia with DSA revealing low total EEG power, delta arousal, and alpha dropout, but increased BIS values during hepatectomy under GA.
A 76-year-old woman (height 157 cm/weight 64 kg) with left lobe hepatocellular carcinoma was admitted for elective hepatectomy. After the establishment of the standard monitoring system, BIS™ Monitoring System (BIS-Vista™ monitors, Aspect Medical Systems, Newton, MA, USA) and BIS™ Quatro (4 Electrodes) Sensor (Aspect Medical Systems) were used to monitor the depth of anesthesia. A radial arterial line and central venous catheter were inserted after GA induction.
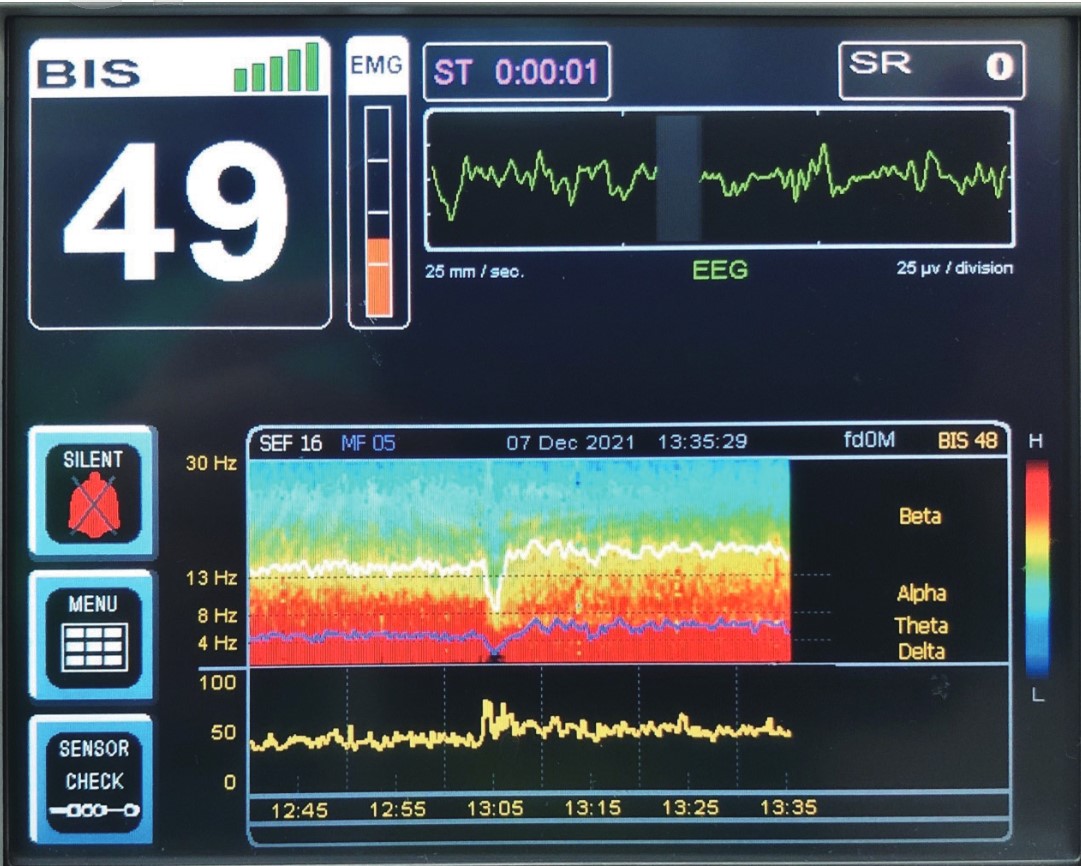
As acute blood loss of 500 mL occurred, increasing heart rate of 110 bpm, decreasing arterial blood pressure of 52/30 mmHg, and reducing peripheral oxygen saturation of 65% were noted during surgery. We adjusted FiO2 (from 50% to 100%), administered ephedrine (total 20 mg), and 0.9% normal saline 250 mL for volume replacement. Then, the critical condition resolved within 2 minutes. In the period, DSA revealed delta arousal and alpha dropout. In addition, the BIS value, spectral edge frequency (SEF), and median frequency (MF) showed 70, 7, and 2, respectively (Figure 1). The surgical time was 14 hours and the total blood loss of 1,000 mL. The patient was sent to the intensive care unit after surgery and extubated the next morning without any sequelae.
Our patient suffered from hypovolemic shock with hypoxia, and DSA revealed the low power of EEG as low SEF and MF, reflecting the low perfusion status of the brain. Lee et al.1 reported that significant cerebral ischemia or hypoperfusion during anesthesia could be detected using EEG changes, particularly a sudden alteration in the EEG during stable anesthesia. For instance, shifts in power from higher to lower frequency ranges, decreases in waveform amplitude, isoelectric waveforms, or periods of burst suppression may indicate incidental cerebral ischemia.1
Download full-size image
During hypovolemic shock and hypoxia, the density spectral array of bispectral index (BIS) monitor showed alpha wave dropout with delta arousal, and the BIS index, spectral edge frequency (SEF), and median frequency (MF) showed 70, 7, and 2, respectively.
Alpha dropout and delta arousal during hypovolemia-associated hypoxia were also detected in our patient. Fanciullacci et al.3 reported that cortico-subcortical ischemic stroke patients presented a higher delta power and lower alpha power than subcortical ischemic stroke patients. In addition, when the cerebral blood flow was less than 25–35 mL/100 g/min, the disappearance of alpha and beta waves was detected in the following seconds. At a more advanced stage, a marked slowing down of the electrogenesis, which was linked to the appearance of delta waves.2 Therefore, the DSA of our case revealed higher delta power and lower alpha power might indicate cortico-subcortical ischemic stroke or hypoperfusion during transient hypovolemia. García et al.4 reported that alpha dropout and delta arousal were associated with noxious stimuli as high concentrations of anesthetic drugs with insufficient opioids. In our case, the alpha dropout and delta arousal occurred with decreased EEG power during transient hypovolemia. In this emergency situation, the surgical stimulation might be intense to result in alpha dropout and delta arousal. However, during noxious stimulation, the total power of EEG does not decrease.4 Therefore, surgical stress-induced alpha dropout and delta arousal are not a preferred interpretation in our patient. Lee et al.1 reported the BIS index dropped during cerebral ischemia or hypoperfusion; however, the BIS index increased in our case during hypovolemia. The increased BIS index might result from ephedrine administration.5
A growing number of anecdotal reports and small case series support that BIS monitor can detect cerebral ischemia or hypoperfusion. It must be stressed that the interpretation of BIS monitor in such settings must be guarded and should include a consideration of other clinical and diagnostic information. Moreover, large prospective studies are necessary before this technology can be reliably used to monitor cerebral perfusion and other aspects of brain function during surgery.
Acknowledgment
We thank the patient for signing the informed consent for publication.
Conflict of Interest
None to all authors.
References
| 1 |
Lee KH, Egan TD, Johnson KB.
Raw and processed electroencephalography in modern anesthesia practice: a brief primer on select clinical applications.
Korean J Anesthesiol. 2021;74(6):465-477.
|
| 2 |
Sastre JA, López T, Reta L.
Changes in density spectral array of bilateral BIS during carotid external compression in cardiac surgery.
J Clin Monit Comput. 2018;32(6):1147-1148.
|
| 3 |
Fanciullacci C, Bertolucci F, Lamola G, et al.
Delta power is higher and more symmetrical in ischemic stroke patients with cortical involvement.
Front Hum Neurosci. 2017;11:385.
|
| 4 |
García PS, Kreuzer M, Hight D, Sleigh JW.
Effects of noxious stimulation on the electroencephalogram during general anaesthesia: a narrative review and approach to analgesic titration.
Br J Anaesth. 2021;126(2):445-457.
|
| 5 |
Takizawa D, Takizawa E, Miyoshi S, et al.
The effect of ephedrine and phenylephrine on BIS values during propofol anaesthesia.
Eur J Anaesthesiol. 2006;23(8):654-657.
|