Abstract
Background
The withdrawal or continuation of angiotensin II receptor blockers (ARBs) before surgery continues to be debated. We hypothesized that this is because ARBs with different half-lives have not been studied individually. This retrospective study aimed to clarify whether the degree of hypotension during anesthesia induction differs among ARBs with different half-lives.
Methods
We included patients who received general anesthesia with regular oral administration of telmisartan (group T) or valsartan (group V), which have half-lives of approximately 24 and 6 hours, respectively. The frequency of hypotension and vasopressor frequency and dose during anesthesia induction were compared between the two groups. At our hospital, ARBs were withdrawn on the day of surgery in all patients.
Results
Groups T and V included 190 and 132 patients, respectively. Patient backgrounds in group V were significantly more strongly associated with the use of calcium channel blockers. No significant differences were observed in the use of other concomitant antihypertensive medications, cardiovascular complications, or renal function. The time during which the mean arterial blood pressure was < 60 mmHg during anesthesia induction was significantly greater in group T than in group V (11 min vs. 7 min,
Conclusion
Patients taking telmisartan showed more hypotensive during the induction of general anesthesia than those taking valsartan, even after withdrawal on the day of surgery.
Keywords
angiotensin II receptor antagonists, hypotension, telmisartan, valsartan
Introduction
Angiotensin II receptor blockers (ARBs) exert their effects by inhibiting the renin-angiotensin (RA) system and are therefore widely used as antihypertensive agents for patients undergoing surgery.1 ARBs are useful antihypertensive agents; however, these drugs should be taken with caution when administered as preoperative medication, owing to their significant effect on blood pressure (BP) during general anesthesia.
BP maintenance is based on the balance of the sympathetic nervous system, RA system, and arginine vasopressin (AVP) system. The roles of the first two systems are significant, whereas the impact of the AVP system is negligible. Because the sympathetic nervous system is depressed during general anesthesia, patients taking preoperative ARBs, which depress the RA system, may experience hypotension and are sometimes refractory to vasopressors.2 Notably, these patients have a higher incidence of intraoperative hypotension, acute kidney injury (AKI), and major adverse cardiac and cerebrovascular events, as well as significantly lower BP, compared to patients taking beta blockers or calcium channel blockers.3,4 Moreover, complications are also associated with intraoperative hypotension, such as an increased risk of acute ischemic stroke with a mean arterial pressure (MAP) of < 60 mmHg for > 20 minutes5 and an increased risk of 30-day mortality with a MAP of < 50 mmHg for > 5 minutes6. As even short periods of hypotension increase the risk of complications, prevention of intraoperative hypotension is an important task for anesthesiologists.
The withdrawal or continuation of RA inhibitors (angiotensin-converting-enzyme inhibitors [ACE-I] or ARBs) on the day of surgery to prevent hypotension during general anesthesia has been a topic of debate for many years.1,7-11 Reportedly, the withdrawal of RA inhibitors on the day of surgery reduces the risk of intraoperative hypotension.1,7,8 However, it has also been reported that taking these medications preoperatively is not associated with intraoperative hypotension.9-11. Nevertheless, this topic remains inconclusive, and many studies have investigated it in recent years.12 The inconclusiveness may be due to the fact that each type of RA inhibitor was not examined separately but rather lumped together, even though their half-lives varied. Moreover, to the best of our knowledge, no study, to date, has examined ARBs in a drug-specific manner. In this study, we investigated hypotension during the induction of general anesthesia in patients taking telmisartan or valsartan, which have different half-lives.
Methods
Ethical Approval and Consent to Participate
This study was approved by the Ethics Committee of the University Hospital on November 18, 2021 (approval no. 2021-285). Since this was a single-center retrospective observational study, the Ethics Committee determined that written informed consent was not required.
Study Population
We recruited patients older than 20 years who underwent general anesthesia at Yamagata University Hospital between January 2019 and June 2021 who were taking telmisartan or valsartan preoperatively. The participants were selected using an electronic medical record retrieval system. The exclusion criteria were as follows: (1) patients who had only non-invasive arterial blood pressure (NIBP) measurements at the time of anesthesia induction because measurements taken every 2.5 or 5.0 minutes were deemed insufficient for BP comparisons; (2) patients who underwent emergency surgery since the timing of the last dose of telmisartan or valsartan was unknown; (3) patients who underwent cardiac surgery because many patients have impaired cardiac function and may actively use catecholamines or anesthetics with minimal hemodynamic effects from anesthesia induction; and (4) patients whose airway was secured using a laryngeal mask airway (LMA), because an LMA is much less irritating than tracheal intubation.
Data Collection
For BP data, the baseline was BP and heart rate at the time of the first vital sign measurement after entering the operating room. The BP from the NIBP measurement was used until the catheter was inserted for intra-arterial BP measurement. When measurements at NIBP were taken every 2–5 minutes, we obtained the previous BP measurement every minute until the next BP measurement was recorded. In the case of position change (prone, side-lying, beach chair), the data acquisition was terminated. Systolic BP of > 300 mmHg or < 20 mmHg, diastolic BP of > 200 mmHg or < 10 mmHg, and diastolic BP exceeding systolic BP were considered errors and were excluded.
The following data on anesthesia were extracted from the electronic anesthesia recording system ORSYS® (Philips Electronics Japan, Tokyo, Japan): the initial BP and heart rate upon entering the operating room, type of anesthesia induction drug (propofol, remimazolam, or midazolam), and dose of remifentanil at the start of administration. In addition, the following data were obtained: types of anesthesia maintenance drugs (propofol, inhalation anesthetics, and remimazolam); amounts of ephedrine and phenylephrine used as vasopressors and whether catecholamine was used; time of anesthetic induction (time between anesthetic administration and start of surgery); and time (minutes) with a MAP of < 60 mmHg during anesthesia induction.
The following data were extracted from HOPE® (Fujitsu, Tokyo, Japan): sex, height, and weight; surgical technique; timing of last oral administration of telmisartan or valsartan; estimated glomerular filtration rate (eGFR) from blood tests; concomitant antihypertensive medications (alpha, beta, and calcium channel blockers and diuretics); preoperative complications such as diabetes mellitus, cardiac/cerebrovascular disease, chronic obstructive pulmonary disease; American Society of Anesthesiology Physical Status (ASA-PS); smoking status; postoperative cardiovascular disease; and stroke.
The antihypertensive potency of telmisartan is reported to be approximately twice as strong as that of valsartan.13,14 Therefore, in this study, telmisartan 20 mg and valsartan 40 mg were evaluated as having equivalent antihypertensive efficacy.
Timing of Preoperative ARB Administration
In all cases, ARBs were withdrawn on the day of surgery.
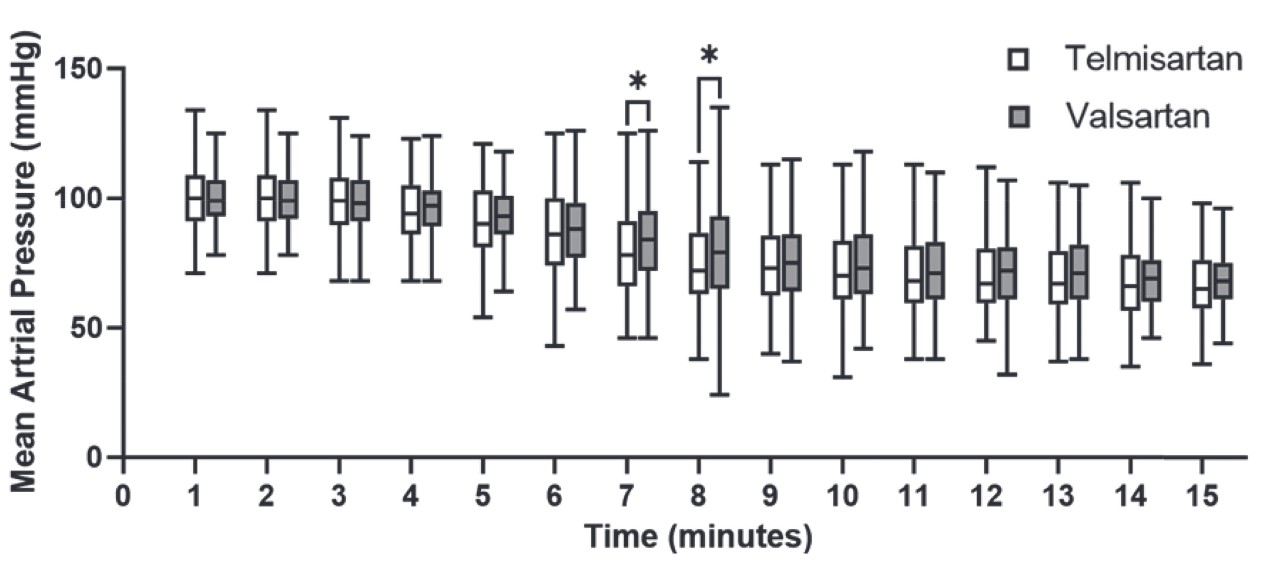
BP was compared during anesthesia induction (from the administration of anesthetics to the start of surgery), considering the hemodynamic effects of surgical invasion. The primary outcome was the time (minutes) during which patients had a MAP < 60 mmHg during induction of general anesthesia. Hypotension was defined as a MAP of < 60 mmHg because a previous review reported that a MAP of < 60–70 mmHg was associated with organ damage in non-cardiac surgery.15 The secondary outcome was the frequency and amounts of vasopressors used during anesthesia induction. Additionally, the maximum and minimum mean BP were extracted during the period, and MAP was extracted every minute up to 15 minutes from the start of anesthesia induction.
Continuous variables were determined as parametric or nonparametric data using the Shapiro–Wilk test. Parametric data are expressed as means ± standard deviations and were compared using Student’s
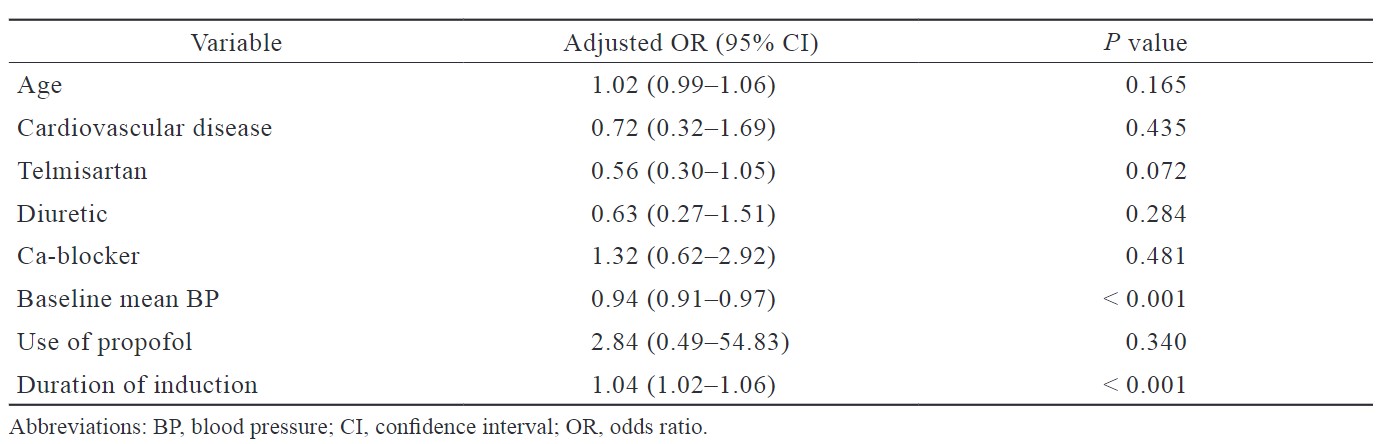
Patients with MAP < 60 mmHg at induction of anesthesia were defined as the hypotensive group, and multivariate logistic regression analysis was performed to identify independent risk factors for hypotension at anesthesia induction. Covariates included in the analysis were age, coexisting cardiovascular disease, MAP before general anesthesia, propofol use, and concomitant diuretics, which have been reported to be risk factors for hypotension.16-18 In addition to these factors, concomitant Ca blockers, duration of anesthesia induction, and oral telmisartan were also included in this analysis.
Power analysis was not performed because of the retrospective study design and the lack of previous studies for reference. GraphPad Prism (v10.0.2; GraphPad Software, San Diego, CA, USA) was used to analyze the data.
Results
During the study, 8,791 patients received general anesthesia at the hospital. Of these, 361 and 232 patients were regularly taking telmisartan and valsartan, respectively. In the telmisartan and valsartan groups, emergency surgery was performed in 49 and 12 cases, respectively. Only NIBP was available in 96 and 76 cases, and cardiac surgery was performed in 20 and 9 cases of groups T and V, respectively. An LMA was used in 6 and 3 cases, respectively. After excluding these cases, the analysis included 190 patients in the telmisartan group and 132 patients in the valsartan group (Figure 1). Patients withdrew from the intake of telmisartan or valsartan on the day of surgery. There were no significant differences in patient background in terms of age, body size, preoperative comorbidities, eGFR, or timing of ARB administration on the day before the surgery. The only difference, however, was the concomitant use of calcium channel blockers, which was less common in the telmisartan group than in the valsartan group (69.4% vs. 82.5%, respectively,
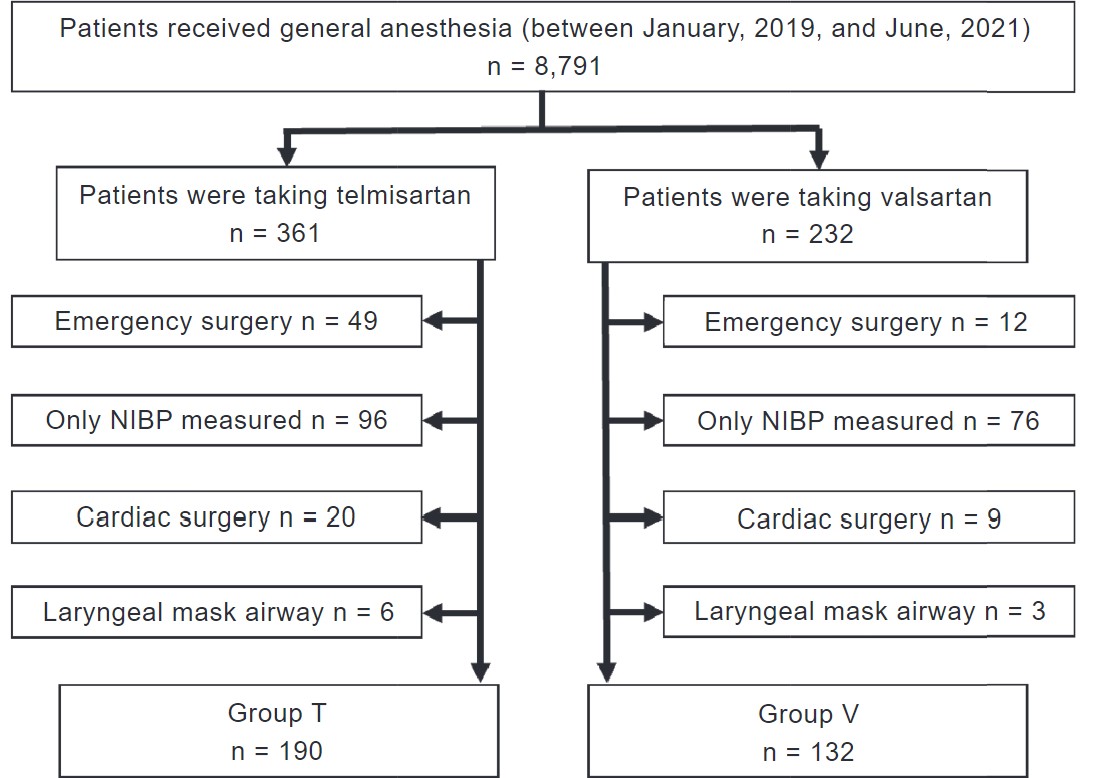
Download full-size image
Abbreviation: NIBP, non-invasive arterial blood pressure.
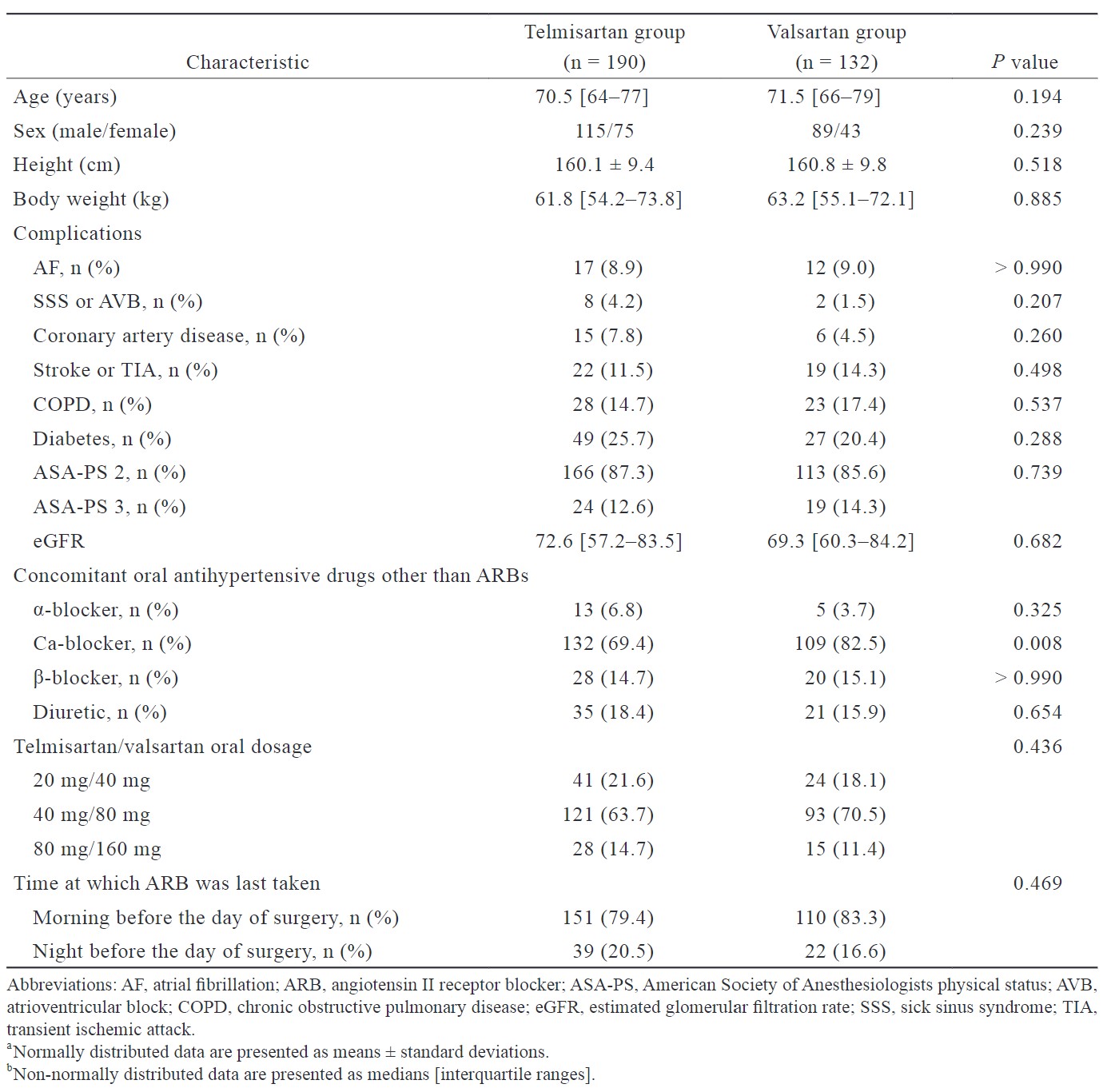
Download full-size image
Download full-size image
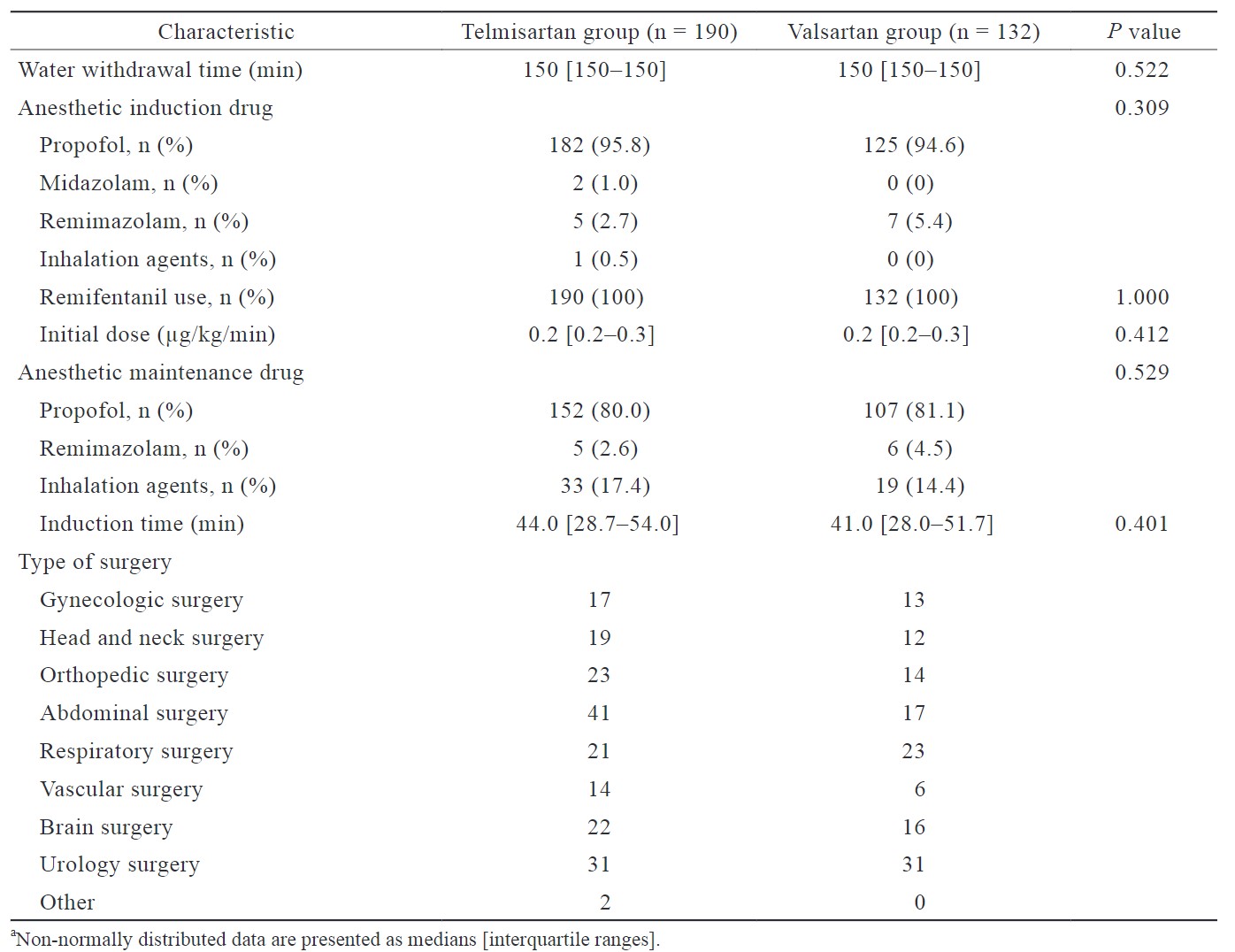
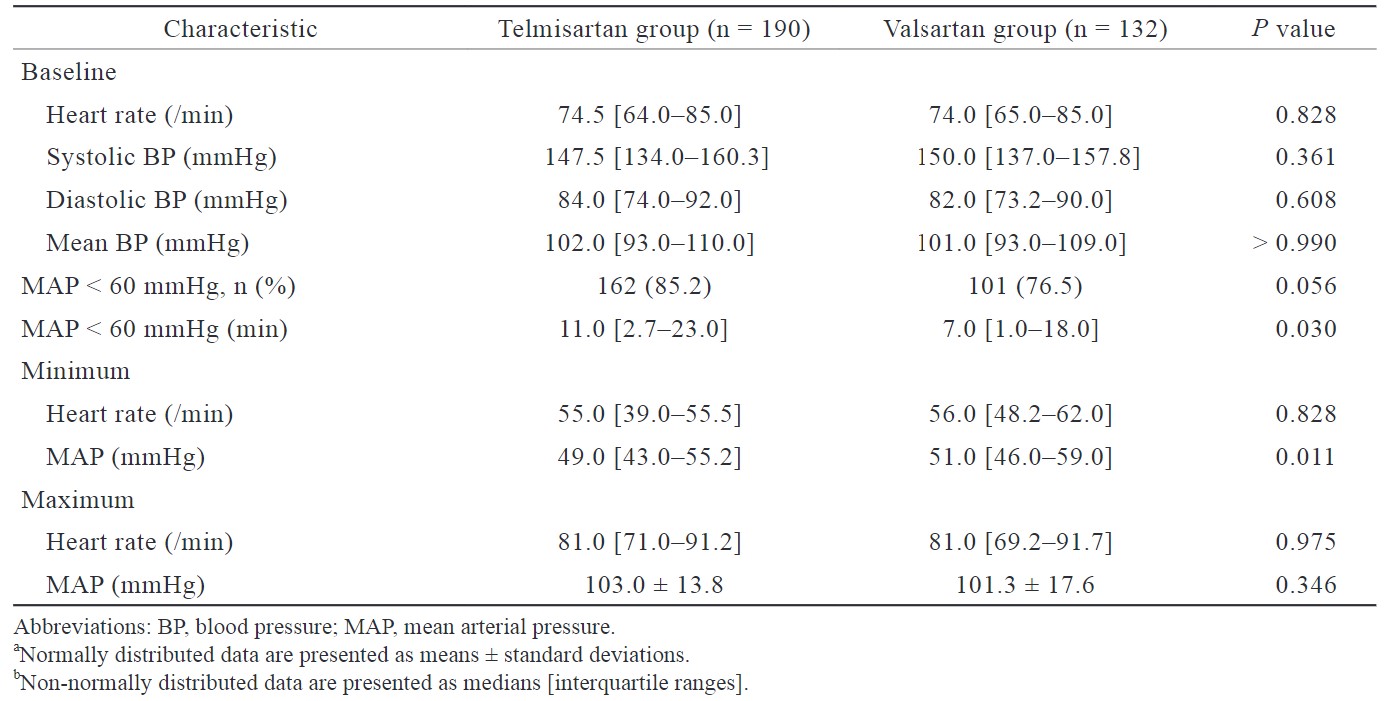
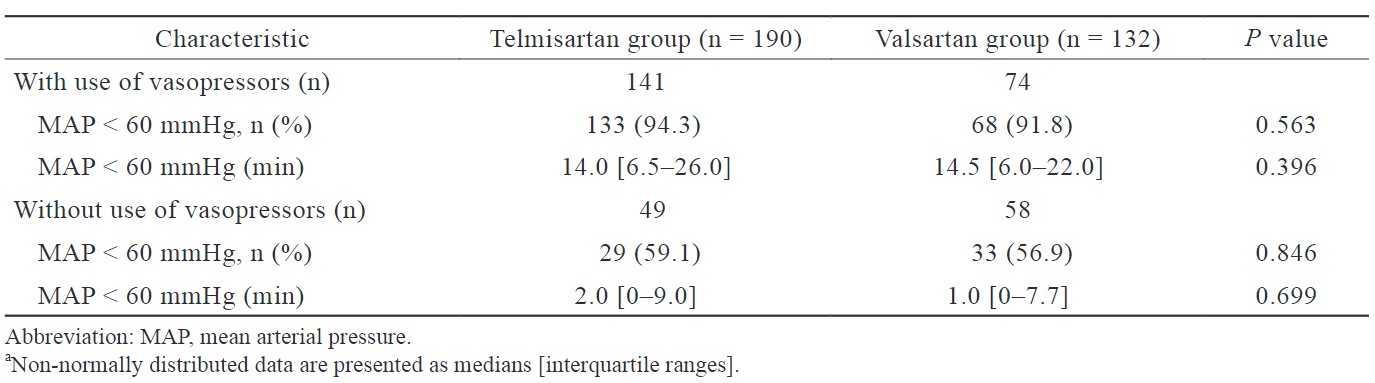
There were no significant differences in BP or heart rate upon entry into the operating room or the induction time of anesthesia between the two groups. There was no significant difference in the percentage of cases in which MAP was < 60 mmHg at anesthesia induction, although the time (minutes) during which MAP was < 60 mmHg at anesthesia induction was significantly longer in the telmisartan group than in the valsartan group (11 min [interquartile range: 2.7–23.0] vs. 7 min [1.0–18.0], respectively,
Download full-size image
Download full-size image
*The telmisartan group had a significantly lower mean arterial pressure than the valsartan group (
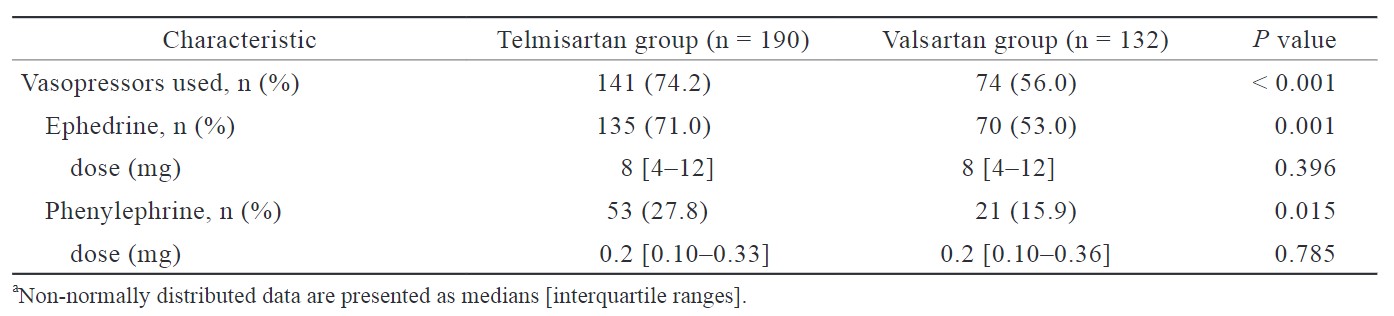
The proportion of patients in the telmisartan group who used vasopressors, such as ephedrine and phenylephrine, was significantly higher than that in the valsartan group (74.2% vs. 56.0%, respectively,
Multivariate logistic regression analysis revealed that baseline mean BP (odds ratio [OR]: 0.94, 95% confidence interval [CI]: 0.91–0. 97,
No postoperative complications, such as myocardial damage or stroke, were observed in either group.
Download full-size image
Download full-size image
Download full-size image
Discussion
In this study, patients taking telmisartan were significantly more hypotensive during anesthesia induction than those taking valsartan, even if the drug was withdrawn on the day of surgery. The number of vasopressor users was also significantly higher in the telmisartan group. To the best of our knowledge, this study is the first to show that different types of ARBs have different effects on BP during general anesthesia.
The major difference between telmisartan and valsartan is their half-lives. The half-lives of ARBs vary; the reported half-lives of valsartan, candesartan, azilsartan, and telmisartan are 4.0–9.0 hours, 3.5–11.0 hours, 13.0 hours, and 20.0–24.0 hours, respectively.19-21 Valsartan has a short half-life, while telmisartan has a long half-life. Refractory hypotension can occur before surgery despite the withdrawal of telmisartan, owing to its long half-life.22 At our institution, all the patients were asked to withdraw the intake of ARBs on the day of surgery, and there was no difference in the timing of oral administration of both drugs on the day before surgery (Table 1). The difference in the half-lives of valsartan and telmisartan may have affected hypotension during anesthesia induction; therefore, we deemed it necessary to examine each drug separately rather than grouping all ARBs. However, definite conclusions cannot be drawn from this study, necessitating future prospective studies.
The difference in median time (minutes) during which the MAP was < 60 mmHg between groups T and V was only 4 minutes (11 min vs. 7 min; Table 3), although this was only during a short, specific period at anesthesia induction. Once surgery begins, invasive procedures may be added, and BP may increase; however, if the duration of surgery and anesthesia is prolonged, MAP may stay below 60 mmHg for a longer time in the telmisartan group than in the valsartan group. We believe that this difference may be clinically significant, as MAP of < 60 mmHg for 20 minutes or more reportedly increases the risk of acute stroke and AKI,5,23 and MAP of < 60–70 mmHg is associated with organ damage during non-cardiac surgery.15 This means that in patients taking telmisartan, hypotension after anesthesia induction should be anticipated and prepared for vasopressors ready and monitoring circulatory dynamics more frequently than usual. Fortunately, no postoperative cardiovascular complications were observed in this study. Previous reports have shown that the incidence of postoperative ischemic stroke in non-cardiac surgery was 0.3%,5 myocardial injury after surgery was 7.4%, and myocardial infarction was 2.8%.24 The lack of postoperative complications in this study may be attributed to the small number of cases included, as well as to the fact that all patients were elective surgical cases, and the majority were ASA-PS2. Thus, the patients may have been in good preoperative condition, which is why no complications were observed.
There was almost no difference in patient background between groups T and V; however, only the concomitant use of calcium channel blockers was significantly higher in the valsartan group. A previous study reported that the concomitant use of diuretics with ACE-I/ARB contributed to intraoperative hypotension; however, this was not observed with calcium channel blockers.16 In this study, the use of diuretics did not significantly differ between the two groups. Although there was a difference in the use of calcium channel blockers, this difference was less pronounced in the telmisartan group, which had significantly lower BP. Thus, it had less influence on the results of this study. In Japan, fixed-dose combination tablets of ARB and calcium channel blockers are available. Telmisartan is available as Micamlo® Combination Tablets (telmisartan/amlodipine, 40 mg/5 mg or 80 mg/5 mg; Nippon Boehringer Ingelheim Co., Ltd., Tokyo), and valsartan is available as EXFORGE® Combination Tablets (valsartan/amlodipine, 80 mg/5 mg; Novartis Pharma K.K., Tokyo, Japan) and ATEDIO® Combination Tablets (valsartan/cilnidipine, 80 mg/10 mg; Mochida Pharmaceutical Co., Ltd., Tokyo). Since the fixed-dose combination tablet of valsartan is more widely available than telmisartan, and since EXFORGE® is also available in an orally disintegrating tablet form, it is possible that many patients in the valsartan group were taking calcium channel blockers in this study. In our facility, fixed-dose combination drugs are prescribed separately after admission so that only ARB and calcium channel blockers can be discontinued and continued, respectively.
In this study, vasopressors were used more frequently in the telmisartan group. Because this was a retrospective study, the timing of vasopressor use was determined by the anesthesiologist in charge, and the criteria for its use were not standardized. Therefore, the telmisartan group may have had over- or under-utilized vasopressors compared to the valsartan group. However, stratified comparisons of patients with and without vasopressors showed no significant difference in hypotension between the two groups (Table 5). It is unlikely that either group was biased toward the use of vasopressors, and we believe that they were used appropriately. Although vasopressors were more frequently used in the telmisartan group, BP in this group remained < 60 mmHg for a longer period; this could be due to the greater degree of hypotension in the telmisartan group. The lowest MAP during anesthesia induction was significantly lower in the telmisartan group. The effect of RA system inhibition may have been stronger with telmisartan than with valsartan, resulting in reduced responsiveness to vasopressors.25
At 7 or 8 minutes after anesthesia induction, the MAP was significantly lower in the telmisartan group than in the valsartan group. In a previous report, BP decreased until 7–10 minutes after anesthesia induction,26 and BP did not significantly differ in the first 4 minutes with and without ARBs but was significantly lower at 5 minutes with ARBs.27 In this study, the BP significantly differed between groups V and T at similar time points. Thereafter, no significant differences were observed after 8 minutes in the two groups, presumably due to the appropriate use of vasopressors at the time of the BP decrease.
MAP was < 60 mmHg in 85.2% of patients in the telmisartan group and 76.5% in the valsartan group. Other reports indicate that the systolic BP was < 85 mmHg during general anesthesia in 65%11 and 60%8 of patients taking ACE-I/ARBs. Although the incidence of hypotension is not comparable to that in previous studies owing to differences in the backgrounds of the included patients and in the definition of hypotension, it was particularly high in the telmisartan group. This may be due to telmisartan having a longer half-life than other ARBs; hence, even withdrawal on the day of surgery may not have been sufficient.
In the present multivariate logistic regression analysis, low mean BP before general anesthesia and a long anesthesia induction time were identified as independent risk factors for the occurrence of hypotension during the induction of general anesthesia. The low baseline mean BP was a risk factor for the occurrence of hypotension, which is consistent with previous reports.18 Since a longer anesthesia induction time induces a longer time for the analysis of this study, we believe that a MAP < 60 mmHg even once was an independent risk factor when defined as being included in the hypotension group. In the present results, comparing telmisartan and valsartan, neither was a significant risk factor for hypotension during induction of anesthesia. However, we also investigated the duration (minutes) of MAP < 60 mmHg and the frequency of vasopressors used during induction of anesthesia, and although telmisartan was not a significant risk factor for the incidence of hypotension compared with valsartan, the duration of hypotension during anesthesia induction was significantly longer in patients who were taking oral telmisartan.
This study had certain limitations. First, although we obtained patient background and surgical information possibly related to hypotension, the retrospective study design may have entailed unknown confounding factors. Second, we were unable to obtain detailed information on the amount of anesthetic used, although the type of anesthetic used in the two groups did not differ; therefore, we could not examine this issue. Third, we could not assess the volume of infusion during anesthesia induction or preoperative dehydration. Finally, we could not calculate the required sample size for the current study. Future studies should calculate and ensure an appropriate sample size to generalize these results. Prospective study designs should also be considered to control variables and reduce bias relevant to the analysis.
In non-cardiac surgery, patients taking telmisartan, an ARB with a long half-life, were more likely to be hypotensive during anesthesia induction, even after withdrawal on the day of surgery, compared to patients taking valsartan.
Conflict of Interest
The authors have no competing interests to declare.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
| 1 |
Roshanov PS, Rochwerg B, Patel A, et al.
Withholding versus continuing angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers before noncardiac surgery: an analysis of the Vascular events In noncardiac Surgery patIents cOhort evaluatioN Prospective Cohort.
Anesthesiology. 2017;126(1):16-27.
|
| 2 |
Park KS, Yoo KY.
Role of vasopressin in current anesthetic practice.
Korean J Anesthesiol. 2017;70(3):245-257.
|
| 3 |
Zainudheen A, Scott IA, Caney X.
Association of renin angiotensin antagonists with adverse perioperative events in patients undergoing elective orthopaedic surgery: a case-control study.
Intern Med J. 2017;47(9):999-1005.
|
| 4 |
Brabant SM, Bertrand M, Eyraud D, Darmon PL, Coriat P.
The hemodynamic effects of anesthetic induction in vascular surgical patients chronically treated with angiotensin II receptor antagonists.
Anesth Analg. 1999;89(6):1388-1392.
|
| 5 |
Mazzeffi M, Chow JH, Anders M, et al.
Intraoperative hypotension and perioperative acute ischemic stroke in patients having major elective non-cardiovascular non-neurological surgery.
J Anesth. 2021;35(2):246-253.
|
| 6 |
Monk TG, Bronsert MR, Henderson WG, et al.
Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery.
Anesthesiology. 2015;123(2):307-319.
|
| 7 |
Hollmann C, Fernandes NL, Biccard BM.
A systematic review of outcomes associated with withholding or continuing angiotensin-converting enzyme inhibitors and angiotensin receptor blockers before noncardiac surgery.
Anesth Analg. 2018;127(3):678-687.
|
| 8 |
Comfere T, Sprung J, Kumar MM, et al.
Angiotensin system inhibitors in a general surgical population.
Anesth Analg. 2005;100(3):636-644.
|
| 9 |
Yoon U, Setren A, Chen A, Nguyen T, Torjman M, Kennedy T.
Continuation of angiotensin-converting enzyme inhibitors on the day of surgery Is not associated with increased risk of hypotension upon induction of general anesthesia in elective noncardiac surgeries.
J Cardiothora Vasc Anesth. 2021;35(2):508-513.
|
| 10 |
Vijay A, Grover A, Coulson TG, Myles PS.
Perioperative management of patients treated with angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers: a quality improvement audit.
Anaesth Intensive Care. 2016;44(3):346-352.
|
| 11 |
Trentman TL, Fassett SL, Thomas JK, Noble BN, Renfree KJ, Hattrup SJ.
More hypotension in patients taking antihypertensives preoperatively during shoulder surgery in the beach chair position.
Can J Anaesth. 2011;58(11):993-1000.
|
| 12 |
Legrand M, Futier E, Leone M, et al.
Impact of renin-angiotensin system inhibitors continuation versus discontinuation on outcome after major surgery: protocol of a multicenter randomized, controlled trial (STOP-or-NOT trial).
Trials. 2019;20(1):160.
|
| 13 |
Israili ZH.
Clinical pharmacokinetics of angiotensin II (AT1) receptor blockers in hypertension.
J Hum Hypertens. 2000;14(Suppl 1):S73-S86.
|
| 14 |
Belz GG, Breithaupt-Grögler K, Butzer R, Fuchs W, Hausdorf C, Mang C.
The pharmacological potency of various AT(1) antagonists assessed by Schild regression technique in man.
J Renin Angiotensin Aldosterone Syst. 2000;1(4):336-341.
|
| 15 |
Sessler DI, Bloomstone JA, Aronson S, et al.
Perioperative Quality Initiative consensus statement on intraoperative blood pressure, risk and outcomes for elective surgery.
Br J Anaesth. 2019;122(5):563-574.
|
| 16 |
Kheterpal S, Khodaparast O, Shanks A, O’Reilly M, Tremper KK.
Chronic angiotensin-converting enzyme inhibitor or angiotensin receptor blocker therapy combined with diuretic therapy is associated with increased episodes of hypotension in noncardiac surgery.
J Cardiothorac Vasc Anesth. 2008;22(2):180-186.
|
| 17 |
Ishikawa Y, Tanaka H, Fujiwara M, et al.
Incidence and predictors of intraoperative hypotension during transurethral bladder tumor resection with oral 5-aminolevulinic acid.
Int J Urol. 2024;31(3):238-244.
|
| 18 |
Hojo T, Kimura Y, Shibuya M, Fujisawa T.
Predictors of hypotension during anesthesia induction in patients with hypertension on medication: a retrospective observational study.
BMC Anesthesiol. 2022;22(1):343.
|
| 19 |
Michel MC, Foster C, Brunner HR, Liu L.
A systematic comparison of the properties of clinically used angiotensin II type 1 receptor antagonists.
Pharmacol Rev. 2013;65(2):809-848.
|
| 20 |
Barreras A, Gurk-Turner C.
Angiotensin II receptor blockers.
Proc (Bayl Univ Med Cent). 2003;16(1):123-126.
|
| 21 |
Mets B.
Management of hypotension associated with angiotensin-axis blockade and general anesthesia administration.
J Cardiothorac Vasc Anesth. 2013;27(1):156-167.
|
| 22 |
Hojo T, Shibuya M, Kimura Y, Otsuka Y, Fujisawa T.
Refractory hypotension during general anesthesia despite withholding telmisartan.
Anesth Prog. 2020;67(2):86-89.
|
| 23 |
Sun LY, Wijeysundera DN, Tait GA, Beattie WS.
Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery.
Anesthesiology. 2015;123(3):515-523.
|
| 24 |
Abbott TEF, Pearse RM, Archbold RA, et al.
A prospective international multicentre cohort study of intraoperative heart rate and systolic blood pressure and myocardial injury after noncardiac surgery: results of the VISION Study.
Anesth Analg. 2018;126(6):1936-1945.
|
| 25 |
Brabant SM, Eyraud D, Bertrand M, Coriat P.
Refractory hypotension after induction of anesthesia in a patient chronically treated with angiotensin receptor antagonists.
Anesth Analg. 1999;89(4):887-888.
|
| 26 |
Salvetti G, Di Salvo C, Ceccarini G, et al.
Chronic renin-angiotensin system (RAS) blockade may not induce hypotension during anaesthesia for bariatric surgery.
Obes Surg. 2016;26(6):1303-1307.
|
| 27 |
Bertrand M, Godet G, Meersschaert K, Brun L, Salcedo E, Coriat P.
Should the angiotensin II antagonists be discontinued before surgery?
Anesth Analg. 2001;92(1):26-30.
|