Abstract
Background
Anesthesia for interventional bronchoscopy (IB) presents significant challenges, primarily due to unpredictable responses such as coughing, airway spasms, and desaturation, even with monitored anesthetic care. However, the nociception inducing such responses and the impact of adding topical anesthesia (TA) have rarely been investigated. This study aims to map the timing and intensity of nociception, determine TA onset, and clarify TA’s role in blocking nociception with subsequent IB procedures.
Methods
Analgesia nociception index (ANI) and mean arterial blood pressure (MBP) were collected in patients undergoing IB procedures with bispectral index (BIS)-controlled intravenous anesthesia. Data were compared and analyzed along with various stages: anesthetic induction with iGel insertion, fibro-optic bronchoscopy (FOB) insertion, and applying TA with the spray-as-you-go (SAYGO) method using xylocaine, up to 30 minutes with subsequent IB procedures.
Results
Data from 82 patients were analyzed. Under BIS-controlled anesthesia, iGel insertion decreased ANI significantly (
Conclusions
ANI offers a valuable perspective on nociception, serves as a helpful reference for precise anesthetic management for IB. The key action, such as an ultrashort-acting anesthetic just before FOB insertion to block nociception from the establishment of TA without prolonged effect, is suggested for smooth, subsequent IB procedures.
Keywords
anesthesia, interventional bronchoscopy, nociception
Introduction
With the rapidly growing demand for anesthesia in interventional bronchoscopy (IB) for airway 1,2 and pulmonary diseases using various probes, anesthetic planning must be tailored to achieve both successful interventions and patient comfort. 3,4 However, coughing 5-7 and associated desaturation remain the most undesirable and unpredictable response along with IB procedures, occurring in both awake 8,9 and sedated 10-12 patients. Besides coughing, other adverse events such as breath-holding, airway spasms 13 , and significant hemodynamic changes 14 often arise in response to nociception from airway stimulation. These episodes can lead to complications such as desaturation and arrhythmias, which hinder IB procedures.
For advanced IB procedures requiring extended durations, monitored anesthetic care (MAC) has gained popularity. 15 Strategies, such as adding topical anesthesia (TA) by applying local anesthetics 9,12,16 , have also been recommended for decades as a standard for bronchoscopy with its 1A-level guideline evidence 17 . However, fibro-optic bronchoscopy (FOB) insertion and direct bronchoscopic spray with local anesthetics to establish TA are well-known to trigger coughing before TA onset. For instance, Fadaizadeh et al. 18 reported that achieving “stable bispectral index (BIS)” levels for safe IB practice took an average of 7.9 ± 6.0 minutes, with BIS levels maintained between 40 and 60 (mean 52.0 ± 13.5). Limited research has focused on the most challenging timing, examining the events occurring during this transition period from FOB insertion to effective TA. A smooth, cough-free condition during bronchoscopic spray could enhance the uniformity and completeness of spraying, help to achieve adequate TA for subsequent IB procedures. Moreover, the onset, effects, and role of TA in mitigating nociception from the following IB procedures involving variable probes have not been clearly elucidated with measurable evidence.
Recently, the analgesia nociception index (ANI) has proven effective in monitoring intraoperative nociception. 19 Combining EEG and ANI monitoring has further facilitated precise anesthetic management in response to nociceptive stimuli. 20,21 In this study, we analysed changes in ANI over timeline along IB practice under BIS-controlled sedation. Our objectives were to map the timing and intensity of nociception along the clinical practice for IB, determine TA onset, and clarify TA’s role in blocking nociception with subsequent IB procedures.
Methods
Ethics
This retrospective study was approved by the Research Ethics Committee of National Taiwan University Hospital, Taipei, Taiwan (20241013RINA; approval date: November 25, 2024) and was performed under an approved waiver of informed consent.
Settings
IB procedures were performed in the hybrid bronchoscopy room in National Taiwan University Cancer Center.
Anaesthetic management and sequential timeline for IB procedures:
The timeline for intravenous and topical anesthetic managements for IB procedures was as follows: (1) Anesthetic preparation: With the monitors including ECG, non-invasive blood pressure, pulse oximetry, BIS, and ANI. Preintervention cone beam CT was performed to ensure the planned BI procedures. (2) Anesthetic induction: Anaesthesia was induced with intravenous midazolam, alfentanil, and propofol infusion with target-controlled infusion adjusted to maintain anesthesia with BIS levels between 40 and 60. Supraglottic airways (iGel) were inserted after anesthetic induction with spontaneous breathing. (3) TA application: Following at least 3 minutes’ stabilization after iGel insertion, FOB was inserted through the fixed route of iGels. Bronchoscopic spray with 2% xylocaine with “spray as you go, SAYGO” method after FOB insertion was performed from vocal cords down to bilateral bronchioles to achieve TA. 9,22 (4) Starting IB procedures: IB procedures started immediately after completion of SAYGO with any required interventional probe. Anesthesia was maintained with BIS level between 40 and 60 as well as maintaining ANI > 50. Additional intravenous alfentanil 5 μg/kg was injected while ANI < 50 for more than 30 seconds. 23,24 Ce of propofol infusion was increased while BIS levels ≥ 70, and decreased while BIS levels ≤ 40. After completion of IB procedures, postoperative cone-beam CT was performed to detect possible atelectasis, pneumothorax, and pneumomediastinum. All patients were sent to the post-anaesthesia care unit (PACU) with BIS levels reached 85 after an absence of complications was confirmed.
Data Collection
Data were collected from electronic anaesthetic records which included both BIS levels, mean blood pressure (MBP) and ANI records. IB procedural records including procedure types, time, etc., were also collected. For analyse the effective time of TA, the records of BI procedures less than 30 minutes were excluded.
Statistical Analysis
Data are expressed as the mean
±
standard deviation unless otherwise specified. Comparisons of continuous data along anesthetic timeline were performed using repeated measures analysis of variance (Sigmaplot, Softhome International, Inc.) Pearson correlations were applied to analyze the relationship between BIS and ANI. A
Results
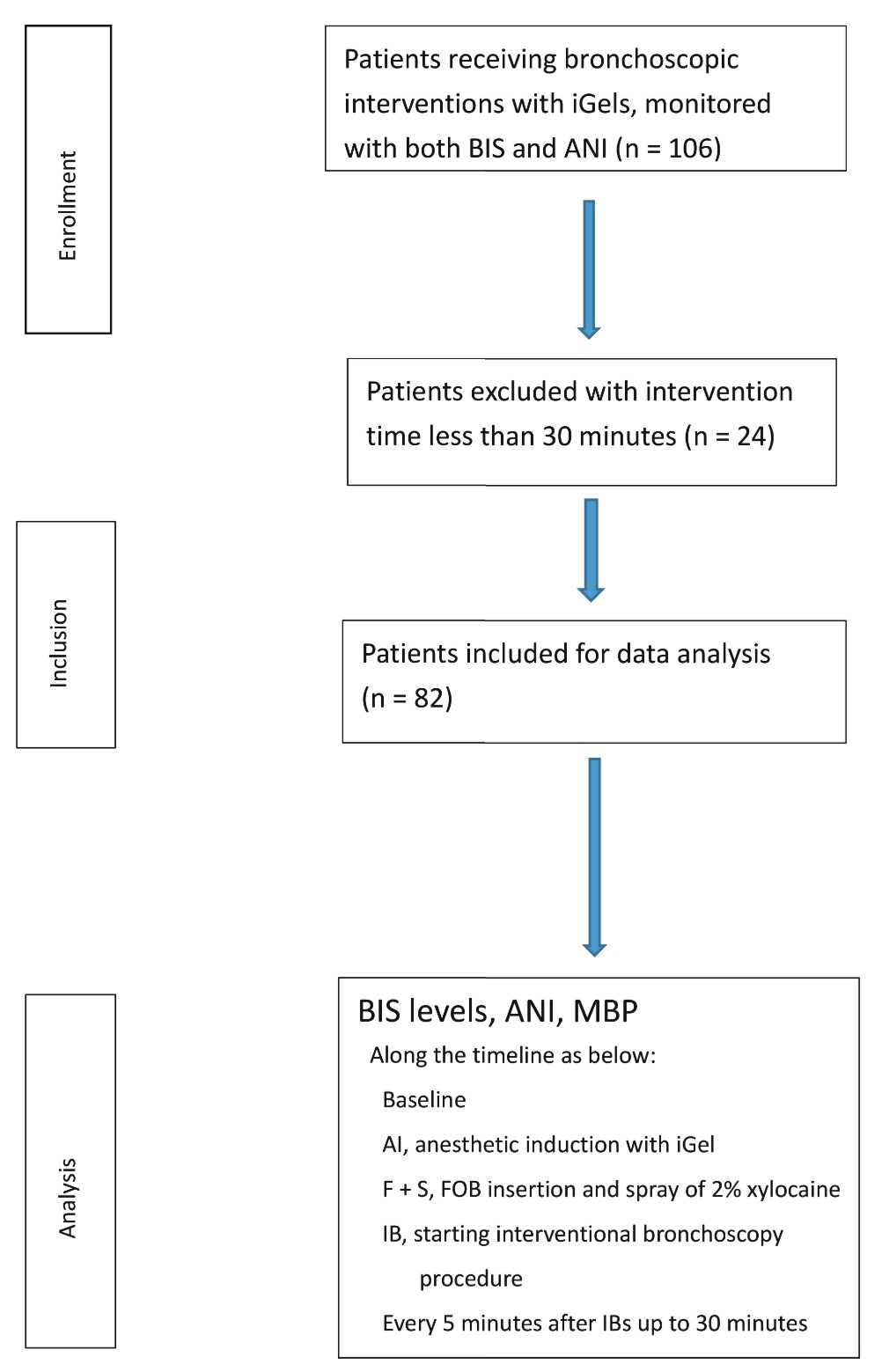
As shown in Figure 1, data from 82 patients were included and analyzed in this study.
Download full-size image
Abbreviations: ANI, analgesia nociception index; BIS, bispectral index; FOB, fibro-optic bronchoscopy; IB, interventional bronchoscopy; MBP, mean arterial blood pressure.
Patients’ demographic and IB data were shown as in Table 1. The intervention procedures or probes applied were decided by pulmonologists in accordance with the results of pre-interventional cone-beam CT, bronchoscopic or endobronchial ultrasound (EBUS) findings, and rapid on-site examinations.
|
Demographic and procedural data |
Outcome |
|---|---|
|
Sex |
|
|
M, n (%) |
44 (53.7) |
|
F, n (%) |
38 (46.3) |
|
Age, years, mean ± SD |
54.36 ± 8.28 |
|
Height, cm, mean ± SD |
164.22 ± 8.11 |
|
Weight, kg, mean ± SD |
64.26 ± 12.94 |
|
BMI, mean ± SD |
23.69 ± 3.55 |
|
Comorbidity |
|
|
Hypertension, n (%) |
23 (28.0) |
|
CAD, n (%) |
3 (3.7) |
|
CVA, n (%) |
2 (2.4) |
|
DM, n (%) |
5 (6.1) |
|
COPD, n (%) |
1 (1.2) |
|
Smoking |
26 (31.7) |
|
Renal disease |
1 (1.2) |
|
Hepatic disease |
16 (19.5) |
|
ASA status |
|
|
I, n (%) |
6 (7.3) |
|
II, n (%) |
66 (80.5) |
|
III, n (%) |
10 (12.2) |
|
BI procedures |
|
|
With ROSE, n (%) |
61 (74.4) |
|
With Cryoprobe, n (%) |
54 (65.9) |
|
With EBUS-TBNA, n (%) |
44 (53.7) |
|
Anesthetic time, minutes, mean ± SD |
80.0 ± 23.8 |
|
IB procedure time, minutes, mean ± SD |
64.2 ± 24.1 |
|
PACU stay, minutes, mean ± SD |
29.5 ± 15.5 |
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; CVA, cerebrovascular accident; DM, diabetes mellitus; EBUS-TBNA, endobronchial ultrasound and transbronchoscopic needle aspiration; IB, interventional bronchoscopy; PACU, postanesthetic care unit; ROSE, rapid on-site microscopic examination; SD, standard deviation.
The changes of BIS levels, ANI, and MBP were demonstrated along the timeline as follows: Preanesthetic baseline, AI (anesthetic induction and iGel insertion), F + S (FOB insertion and SAYGO), IB (start IB procedures after completion of bronchoscopic spray), and every 5-minute interval after IB procedures up to 30 minutes.
The time period from anesthetic induction to FOB insertion was 7.1 ± 4.1 minutes. The time from FOB insertion to complete SAYGO was 4.3 ± 1.1 minutes. The volume of 2% xylocaine for bronchoscopic spray from vocal cords to bilateral bronchioles was 15–20 mL. To maintain ANI and BIS levels during SAYGO, 69/82 (84.1%) patients received extra alfentanil injections. Ce of propofol was increased in 13/82 (15.9%) patients; and decreased in 4/82 (4.9%) patients. No additional alfentanil was given after the completion of SAYGO.
The Changes in BIS Levels
As shown in Figure 2, BIS levels decreased significantly after anesthetic induction (
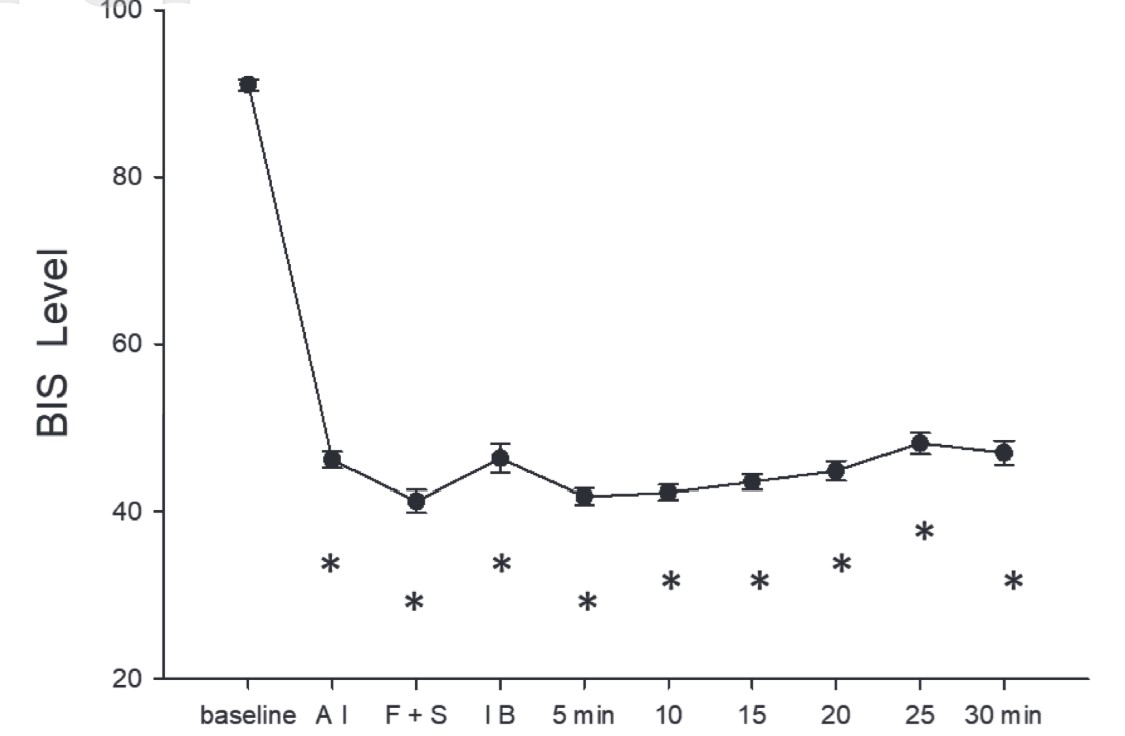
Download full-size image
Data were expressed as means ± standard error (SE)
*: significantly lower than baseline data
Time point: baseline (preanesthetic baseline), AI (anesthetic induction and iGel insertion), F + S (FOB insertion and bronchoscopic spray of 2% xylocaine), IB (start interventional bronchoscopy after completion of bronchoscopic spray), and every 5 minutes with IB procedures up to 30 minutes.
The Changes of ANI
As shown in Figure 3, ANI was significantly decreased with iGel insertion (
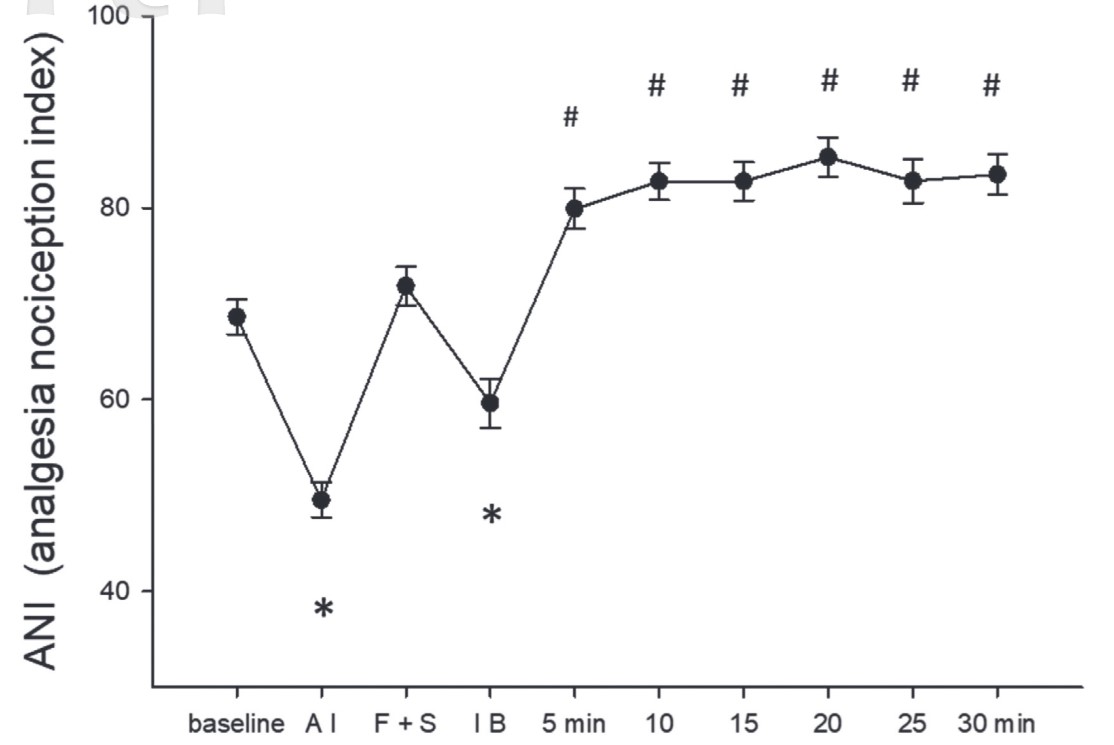
Download full-size image
Data were expressed as means ± standard error (SE)
*: significantly lower than baseline data
#: significantly higher than baseline data
Time point: baseline (preanesthetic baseline), AI (anesthetic induction and iGel insertion), F + S (FOB insertion and bronchoscopic spray of 2% xylocaine), IB (start interventional bronchoscopy after completion of bronchoscopic spray), and every 5 minutes with IB procedures up to 30 minutes.
The Changes of MBP
As shown in Figure 4, MBP decreased significantly (
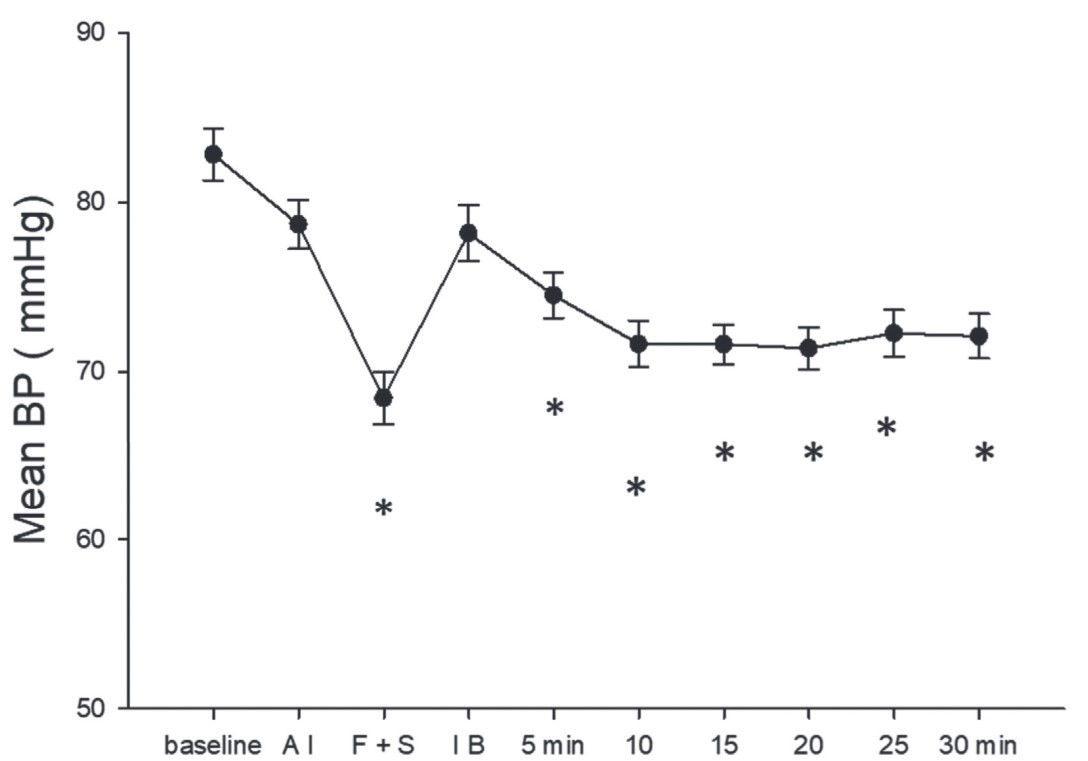
Download full-size image
Data were expressed as means ± standard error (SE)
*: significantly lower than baseline data
Time point: baseline (preanesthetic baseline), AI (anesthetic induction and iGel insertion), F + S (FOB insertion and bronchoscopic spray of 2% xylocaine), IB (start interventional bronchoscopy after completion of bronchoscopic spray), and every 5 minutes with IB procedures up to 30 minutes.
Correlations Between BIS Levels and ANI
As shown in Table 2, the correlation was weak and without statistical significance.
|
Variable |
Correlations |
|
|---|---|---|
|
Baseline |
0.12 |
0.29 |
|
Induction |
0.06 |
0.59 |
|
F + S a |
0.06 |
0.56 |
|
IB b |
0.19 |
0.09 |
|
5 min |
0.08 |
0.49 |
|
10 min |
0.19 |
0.09 |
|
15 min |
0.26 |
0.017 |
|
20 min |
0.16 |
0.16 |
|
25 min |
0.10 |
0.38 |
|
30 min |
0.06 |
0.60 |
Abbreviation: interventional bronchoscopy. a Fibrobronchoscopic insertion and bronchoscopic spray of 2% xylocaine b Interventional bronchoscopy after complete bronchoscopic spray
Discussion
By analyzing the changes of ANI in clinical practice along IB procedures with BIS-controlled intravenous anesthesia, our findings over time reveal the following: (1) Significant nociception was observed with a decrease of ANI at the time of iGel insertion. (2) Another peak of nociception with a significant fall of ANI was induced by FOB insertion and SAYGO, despite the fixed route of iGels. 69/82 (84.1%) patients present with ANI < 50 under adequate systemic anesthesia. (3) ANI significantly returned within 5 minutes of completing SAYGO, remained stably high up to 30 minutes with variable IB procedures. (4) No significant correlation was observed between changes in ANI and BIS levels.
This is the first report documenting the timing and the intensity of nociception using ANI along the sequence for IB procedures. The observed changes in MBP were consistent with ANI trends. iGel insertion induces significant nociception. Following restabilized anesthesia with acceptable BIS level and ANI with the existing iGel, FOB insertion and SAYGO still elicited a significant rise in BP as well as a fall of ANI, underscoring the occurrence of strong nociception despite well-maintained anesthesia. Significant nociceptive stimuli can arise from various anatomical sites within the airway, necessitating a tailored approach to anesthesia that considers these factors. Our results demonstrate what happens in the most challenging timing. More patients (84.1%) required alfentanil injection with low ANI than those (15.9%) required higher propofol infusion during bronchoscopic spray. Notably, following the completion of SAYGO, effects of TA onset with an increase of ANI within 5 minutes, effectively mitigating the nociception from the consequential IB procedures up to 30 minutes, as evidenced by high ANI and stable MBP without requirement for more narcotics.
Our study highlights the timing of TA onset and the role it takes to block nociception from subsequent IB procedures. This finding supports the superiority of TA over systemic narcotics for managing nociception during these procedures, minimizing the side effects such as hypotension and hypoventilation with systemic anesthetics. With stability on both ANI and MBP, TA showed its advantages over adjusting the infusion of short-acting narcotic 25 by waiving systemic influences. Our results agree with the cruciality of TA for IB procedures since IB procedures are associated with the nociception with the greatest disparity with suction, biopsy, cryoprobe treatment, injection of normal saline for washing, withdrawal from airways, etc. The temporal trends in ANI and MBP underscore the key timing of providing sufficient anesthesia to counteract the anticipated nociception with SAYGO. This advancement suggests a paradigm shift towards more personalized anesthesia strategies. Deepening anesthesia immediately before FOB insertion and SAYGO could be favorable for providing a smooth, cough-free bronchoscopic spray to achieve complete TA. With 4-minute average time for bronchoscopic spray, a short-acting narcotic would be favorable. We did not investigate how long TA effects last in this study, but our results agreed with those in a previous report 10 . However, repeated bronchoscopic spray could be indicated for prolonged, advanced IB if ANI starts to decline.
ANI monitoring provided a unique and timely perspective on nociception during IB procedures, often undetectable through BIS levels. Unlike oral or nasal FOB insertion, our results showed that there remains significant nociception arising from the trachea and bronchi during FOB insertion through the fixed route of the existing iGel. Our results could demonstrate what happened in the period before achieving a stable BIS level suitable for IB procedures
18
. Although the BIS level at time point IB after SAYGO (46.5
±
14.0) was significantly higher than that with F + S (42.1
±
12.7,
Our findings, incorporating ANI measurements, help address the challenge of achieving stable BIS levels for safe intraprocedural bronchoscopy (IB), as highlighted by Fadaizadeh et al. 18 . Since BIS monitors primarily reflect the depth of consciousness and not nociceptive responses 26 —particularly those originating from airway stimulation—ANI and systolic blood pressure trends offer valuable complementary information. Therefore, while BIS is useful for monitoring sedation depth and patient comfort after TA onset, it does not adequately capture airway-related nociception.
ANI could help to improve the understanding and cooperation between anesthesiologists and pulmonologists for timely goals in IB procedures. Some endoscopists prefer to spray local anesthetics over the tongue base or pharynx prior to flexible bronchoscope (FOB) or iGel insertion. However, as indicated by ANI measurements, the nociception induced by bronchoscopic spraying cannot be fully prevented by anesthesia sufficient for iGel placement alone. In addition to the discomfort caused by spraying local anesthetics in the oropharyngeal region, residual effects may impact post-procedural cough reflex and swallowing function.
General anesthesia with endotracheal intubation is commonly used for bronchoscopic interventions (BIs) requiring longer durations. However, procedure-related interruptions due to apnea and desaturation remain a concern. Managing anesthesia for BIs under spontaneous breathing poses challenges, particularly due to the risk of bronchospasm or coughing triggered by unpredictable nociceptive responses during airway manipulation. Our findings suggest that incorporating the ANI allows for a better assessment of the timing and adequacy of nociceptive blockade. Anesthetic goals should focus on ensuring a smooth application of TA. In this study, 2% xylocaine is administered for SAYGO, stable anesthesia can typically be maintained for over 30 minutes. Our results demonstrate that 2% xylocaine provides effective anesthesia for a variety of procedures, with a lower risk of systemic toxicity.
Additional strategies, such as the use of high-flow nasal oxygen, may improve oxygenation without the need for an indwelling device and potentially reduce nociception compared to iGels. However, the intense nociceptive response induced by the SAYGO technique remains a challenge. Further studies are warranted to refine anesthesia protocols and better evaluate the cost-benefit balance of managing nociception throughout the upper and lower airways
This retrospective study has several limitations: (1) Data were not collected from patients undergoing IB with endotracheal tubes, as our pulmonologists favor IB without them, achieving satisfactory outcomes 27 . (2) ANI is a measure of parasympathetic tone and has inherent limitations in clinical applications. Baseline autonomic function may vary in older patients or those with cardiovascular conditions such as hypertension. Additionally, we did not analyze the specific intensity of stimulation caused by different types of probes or procedures. However, more than half of our patients underwent EBUS-TBNA or procedures involving cryoprobes. Our findings suggest that TA was effective in managing the nociceptive stimuli associated with larger probes and procedures requiring greater precision.
Conclusions
To elucidate the responses before establishing a smooth operational field, ANI provides valuable insights into nociception along with systemic or TA for IB procedures. Significant nociceptive stimuli can arise from various anatomical sites within the airway, necessitating a tailored approach to anesthesia that considers these factors. Moreover, integrating real-time ANI monitoring could potentially refine the balance between consciousness-nociception and systemic-topical anesthetic management throughout their interventions. The continuous feedback on nociceptive levels informs anesthetic adjustments, ultimately leading to enhanced safety and efficacy in IB procedures.
References
| 1 |
Criner GJ, Eberhardt R, Fernandez-Bussy S, et al.
Interventional bronchoscopy.
Am J Respir Crit Care Med. 2020;202(1):29-50.
|
| 2 |
Perotin JM, Dewolf M, Launois C, Dormoy V, Deslee G.
Bronchoscopic management of asthma, COPD and emphysema.
Eur Respir Rev. 2021;30(159):200029.
|
| 3 |
Lentini C, Granlund B.
Anesthetic considerations for bronchoscopic procedures.
|
| 4 |
Goudra BG, Singh PM, Borle A, Farid N, Harris K.
Anesthesia for advanced bronchoscopic procedures: state-of-the-art review.
Lung. 2015;193(4):453-465.
|
| 5 |
Canning BJ.
Afferent nerves regulating the cough reflex: mechanisms and mediators of cough in disease.
Otolaryngol Clin North Am. 2010;43(1):15-25, vii.
|
| 6 |
Moe AAK, McGovern AE, Mazzone SB.
Jugular vagal ganglia neurons and airway nociception: a target for treating chronic cough.
Int J Biochem Cell Biol. 2021;135:105981.
|
| 7 |
Karlsson JA.
Airway anaesthesia and the cough reflex.
Bull Eur Physiopathol Respir. 1987;23 Suppl 10:29s-36s.
|
| 8 |
Huang CT, Chou HC, Chang HC, et al.
Spray nozzle for topical anaesthesia during flexible bronchoscopy: a randomised controlled trial.
ERJ Open Res. 2024;10(2):00913-02023.
|
| 9 |
Dhooria S, Chaudhary S, Ram B, et al.
A randomized trial of nebulized lignocaine, lignocaine spray, or their combination for topical anesthesia during diagnostic flexible bronchoscopy.
Chest. 2020;157(1):198-204.
|
| 10 |
Kobayashi F, Saraya T, Oda M, et al.
Novel predictive factors for patient discomfort and severe cough during bronchoscopy: a prospective questionnaire analysis.
PLoS One. 2020;15(10):e0240485.
|
| 11 |
Antoniades N, Worsnop C.
Topical lidocaine through the bronchoscope reduces cough rate during bronchoscopy.
Respirology. 2009;14(6):873-876.
|
| 12 |
Müller JN, Kreuzer M, García PS, Schneider G, Hautmann H.
Monitoring depth of sedation: evaluating the agreement between the Bispectral Index, qCON and the Entropy Module’s State Entropy during flexible bronchoscopy.
Minerva Anestesiol. 2017;83(6):563-573.
|
| 13 |
Rex MA.
Laryngospasm and respiratory changes in the cat produced by mechanical stimulation of the pharynx and respiratory tract: problems of intubation in the cat.
Br J Anaesth. 1971;43(1):54-57.
|
| 14 |
El Chafic AH, Eckert G, Rex DK.
Prospective description of coughing, hemodynamic changes, and oxygen desaturation during endoscopic sedation.
Dig Dis Sci. 2012;57(7):1899-1907.
|
| 15 |
Strohleit D, Galetin T, Kosse N, Lopez-Pastorini A, Stoelben E.
Guidelines on analgosedation, monitoring, and recovery time for flexible bronchoscopy: a systematic review.
BMC Pulm Med. 2021;21(1):198.
|
| 16 |
Wahidi MM, Jain P, Jantz M, et al.
American College of Chest Physicians consensus statement on the use of topical anesthesia, analgesia, and sedation during flexible bronchoscopy in adult patients.
Chest. 2011;140(5):1342-1350.
|
| 17 |
Mohan A, Madan K, Hadda V, et al.
Guidelines for diagnostic flexible bronchoscopy in adults: Joint Indian Chest Society/National College of chest physicians (I)/Indian association for bronchology recommendations.
Lung India. 2019;36(Supplement):S37-S89.
|
| 18 |
Fadaizadeh L, Hoseyni MS, Shajareh E, Heydari G, Ardehali SH.
Use of bispectral index score for interventional bronchoscopy procedures.
Tanaffos. 2015;14(4):246-251.
|
| 19 |
Jiao Y, He B, Tong X, Xia R, Zhang C, Shi X.
Intraoperative monitoring of nociception for opioid administration: a meta-analysis of randomized controlled trials.
Minerva Anestesiol. 2019;85(5):522-530.
|
| 20 |
Renaud-Roy E, Morisson L, Brulotte V, et al.
Effect of combined intraoperative use of the nociception level (NOL) and bispectral (BIS) indexes on desflurane administration.
Anaesth Crit Care Pain Med. 2022;41(3):101081.
|
| 21 |
Gruenewald M, Ilies C, Herz J, et al.
Influence of nociceptive stimulation on analgesia nociception index (ANI) during propofol-remifentanil anaesthesia.
Br J Anaesth. 2013;110(6):1024-1030.
|
| 22 |
Kumar MP, Patro M, Panigrahy S, Samal S, Kartheek BS.
Comparison between intravenous dexmedetomidine and spray as you go with 4% lignocaine versus intravenous fentanyl and transtracheal injection of 4% lignocaine for awake nasotracheal intubation with flexible vedioscope—a randomized single-blind prospective study.
Anesth Essays Res. 2021;15(2):213-219.
|
| 23 |
Tribuddharat S, Sathitkarnmanee T, Sukhong P, Thananun M, Promkhote P, Nonlhaopol D.
Comparative study of analgesia nociception index (ANI) vs.
BMC Anesthesiol. 2021;21(1):50.
|
| 24 |
Daccache G, Jeanne M, Fletcher D.
The Analgesia nociception index: tailoring opioid administration.
Anesth Analg. 2017;125(1):15-17.
|
| 25 |
Lee H, Choe YH, Park S.
Analgosedation during flexible fiberoptic bronchoscopy: comparing the clinical effectiveness and safety of remifentanil versus midazolam/propofol.
|
| 26 |
Funcke S, Sauerlaender S, Pinnschmidt HO, et al.
Validation of innovative techniques for monitoring nociception during general anesthesia: a clinical study using tetanic and intracutaneous electrical stimulation.
Anesthesiology. 2017;127(2):272-283.
|
| 27 |
Fang Y, Lin CK, Yao ZH, Fan HJ, Cheng YJ.
Non-intubated bronchoscopic tracheobronchial surgeries with electroencephalogram-monitored intravenous anesthesia: feasibility and outcomes.
J Thorac Dis. 2024;16(5):3042-3050.
|