Abstract
An 81-year-old male, weighing 47 kg and measuring 166 cm in height, presenting a medical history of a major cerebrovascular accident and hypertension, underwent a low anterior resection for rectal carcinoma. Following standard physiologic monitoring, a Bispectral index with density spectral array (BIS-DSA) monitor (BIS-Vista™ monitors, Aspect Medical Systems, Newton, MA, USA) was employed, and general anesthesia was maintained by using target-controlled infusion (TCI, Fresenius Orchestra Primea; Fresenius Kabi AG, Bad Homburg, Germany) with propofol at an effect-site concentration of 1.8 mcg mL -1 and remifentanil at an effect-site concentration of 0.5–3.0 ng mL -1 . At the end of the surgery, a transversus abdominis plane block was performed using a mixture of 15 mL of 2% lidocaine and 15 mL of 1% ropivacaine, followed by discontinuing the TCI system with the train-of-four (TOF) count of 2. After administration of 100 mg of sugammadex and achieving a TOF ratio > 0.9 (Figure 1, red arrow), the patient was extubated smoothly with reactivity and coughing response but no respiratory compromise or spontaneous eye-opening. Subsequently, he exhibited apnea, bradycardia (36 bpm), and hypotension (63/38 mmHg) without pain responses. At that time, there was a sudden drop in the BIS value to 27, along with a concurrent rise in the suppression ratio to 47%, indicating significant cerebral suppression. During the period of bradycardia and hypotension after sugammadex administration, concurrent DSA showed delta arousal and alpha dropout. Spectral edge frequency (SEF) and median frequency (MF) were recorded at 3 Hz and 1 Hz, respectively (Figure 2, red arrow). The suppression ratio was 47, and the suppression time was 6 minutes 16 seconds, which included post-induction hypotension. Emergent interventions, including respiratory support, intravenous administration of atropine (0.5 mg) and calcium chloride (400 mg), resulted in a marked improvement in hemodynamic parameters and level of consciousness. Concurrently, BIS with DSA readings demonstrated a return to the expected electroencephalography (EEG) emergence trajectory (Figure 2). No apparent sequelae were observed throughout this transition.
Download full-size image
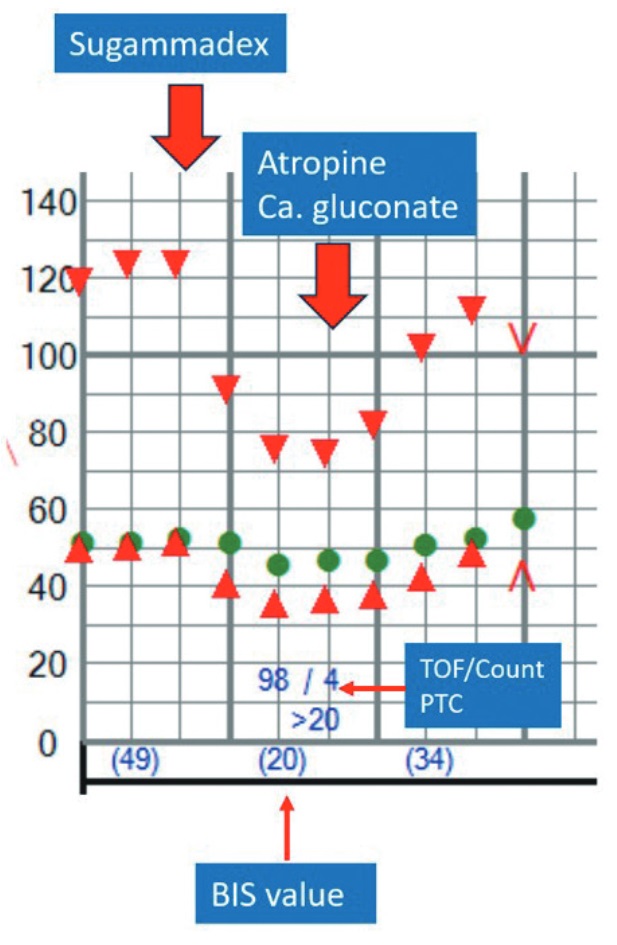
Red downward-pointing triangles represent systolic blood pressure (SBP), red upward-pointing triangles indicate diastolic blood pressure (DBP), and green circles represent heart rate (HR). After administration of sugammadex, neuromuscular monitoring showed a train-of-four (TOF) ratio of 98% with a count of 4 and a post-tetanic count (PTC) > 20, indicating successful recovery from neuromuscular blockade. However, a significant hemodynamic disturbance occurred, with bradycardia and concomitant decreases in both SBP and DBP. Atropine and calcium gluconate were subsequently administered to manage the hemodynamic instability. The Bispectral index (BIS) value remained around 20 during this episode.

Download full-size image
During the period of bradycardia and hypotension after sugammadex administration, the density spectral array showed alpha wave dropout with delta arousal. Concurrently, the bispectral index (BIS), spectral edge frequency (SEF), and median frequency (MF) recorded values of 27, 3, and 1, respectively (red arrow). The suppression ratio was 47, and the suppression time was 6 min 16 s, which included post-induction hypotension.
The patient experienced shock following sugammadex administration. Concurrent monitoring revealed a diminished BIS value with burst-suppression patterns. Furthermore, DSA indicated alpha-wave suppression alongside delta-wave augmentation. The EEG signal attenuation was evidenced by reduced SEF and MF values. A burst suppression pattern on the EEG signifies a substantial reduction in neuronal activity, potentially caused by cerebral hypoperfusion. Cerebral hypoperfusion, referring to diminished blood flow to the brain, can cause numerous neurological impairments. Xu et al. 1 reported that an extended cumulative duration of intraoperative burst suppression may increase the risk of postoperative delirium. In line with our findings, a previous study suggested a connection between brain hypoperfusion and the loss of alpha alongside delta arousal in DSA in a patient experiencing hypovolemic shock. 2 Wu et al. 3 found that a larger infarct volume was linked to increased delta power, and EEG showed a strong correlation with acute stroke behavioral deficits. Furthermore, patients with corticosubcortical ischemic stroke exhibited higher delta power and lower alpha power than those with subcortical ischemic stroke. 4 To summarize, EEG and DSA may be valuable tools for identifying cerebral ischemia and predicting patient outcomes.
The patient’s condition improved after administration of atropine and calcium chloride. Sugammadex, a neuromuscular blockade reversal agent used to accelerate recovery from neuromuscular blockades and prevent residual blockades, has been reported to cause severe bradycardia with hypotension. 5 Consequently, we suggest that the observed alterations in BIS values and DSA patterns were attributable to cerebral hypoperfusion, which likely resulted from bradycardia and shock induced by sugammadex.
Given the possible relationship between the detected DSA changes and brain hypoperfusion, we emphasize the importance of early recognition of sugammadex-induced bradycardia and hypotension. Appropriate treatment with atropine or vasopressors is necessary. However, large prospective studies are warranted to ensure that BIS with DSA can reliably monitor cerebral perfusion for early damage detection.
Conflict of Interest
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
References
| 1 |
Xu N, Li LX, Wang TL, et al.
Processed multiparameter electroencephalogram-guided general anesthesia management can reduce postoperative delirium following carotid endarterectomy: a randomized clinical trial.
Front Neurol. 2021;12:666814.
|
| 2 |
Wu TS, Wu ZF, Lai HC.
Hypovolemic shock and changes in density spectral array of BIS during hepatectomy.
Asian J Anesthesiol. 2024;62(1):63-65.
|
| 3 |
Wu J, Srinivasan R, Burke Quinlan E, Solodkin A, Small SL, Cramer SC.
Utility of EEG measures of brain function in patients with acute stroke.
J Neurophysiol. 2016;115(5):2399-2405.
|
| 4 |
Fanciullacci C, Bertolucci F, Lamola G, et al.
Delta power is higher and more symmetrical in ischemic stroke patients with cortical involvement.
Front Hum Neurosci. 2017;11:385.
|
| 5 |
Boo KY, Park SH, Park SK, Na C, Kim HJ.
Cardiac arrest due to coronary vasospasm after sugammadex administration—a case report.
Korean J Anesthesiol. 2023;76(1):72-76.
|