Abstract
Background: Patients undergoing total hip replacement (THR) experience severe postoperative pain. The advantage of pain relief by continuous epidural anesthesia (CEA) is offset by variou adverse effects. Ultrasound guided (USG) continuous lumbar plexus block (LPB) has emerged as an alternative approach for postoperative analgesia in patients undergoing THR, especially where epidura is diffi cult or contraindicated.
Methods: This randomized controlled trial compared USG-LPB with CEA for postoperative pain relief until 48 hours in patients undergoing THR, with 0.5% ropivacaine (15 mL) used as boluse for both CEA and LPB.
Results: The mean time to the first bolus was 380.60 ± 77.66 min in the LPB group whereas it was 307.40 ± 83.60 min in the epidural group (P = 0.002). Thus, patients in the LPB group too more than one hour longer than the epidural group to take their fi rst bolus, which is clinically meaningful besides being statistically signifi cant. The pain score on movement was also signifi cantly lower, an patient satisfaction higher, in the LPB group. There were no signifi cant intergroup differences about moto power, pain at rest, total ropivacaine consumption, and adverse effects.
Conclusion: USG-LPB is an effective alternative to CEA combined with general anesthesia for postoperative analgesia after THR.
Keywords
continuous epidural anesthesia, postoperative analgesia, randomized controlled trial, total hip replacement, ultrasound guided lumbar plexus block
Introduction
Total hip replacement (THR) surgery causes severe pain in patients in the postoperative period.1 Intense uncontrolled pain delays early ambulation and recovery, and increases hospital expenses due to prolonged stay and physical rehabilitation of the patient. Further, some patients continue to experience acute pain developing into chronic pain after surgery.1 Therefore, proper postoperative pain management strategy needs to be planned.
Anesthetic management involves the use of neuraxial blocks, peripheral nerve blocks, and/or intravenous analgesics. Of these, epidural anesthesia (EA) has been considered the gold standard for postoperative pain management in patients undergoing hip arthroplasty.2 However, the main side-effects associated with the epidural block are hypotension, inadvertent puncture of the epidural venous plexus, accidental misplacement of a catheter in the subarachnoid space, meningitis, abscesses, hematoma formation, etc.3
Lumbar plexus block (LPB) is an effective and reliable means of managing postoperative pain. Further, a unilateral anesthesia/analgesia can be achieved and there is a lack of complete sympathectomy. LPB can be performed blindly or under ultrasound guidance. Blind needle insertion may cause various complications, like epidural spread, total spinal anesthesia, intraperitoneal injection, retroperitoneal hematoma, and renal puncture.4 Ultrasound guided (USG)-LPB is a more effective way to identify and locate the lumbar plexus and also to avoid associated complications.
This study aims to compare the efficacy of continuous EA (CEA) and USG-LPB, with the provision of patient-controlled boluses for control of postoperative pain for patients undergoing unilateral THR.
Methods
The prospective, randomized, controlled trial was conducted in the Department of Anaesthesia, in collaboration with the Department of Orthopaedics, after obtaining approval from the Hospital Ethics Committee (ECR/658/PB/2014, 13-02-2018) and prospective trial registration with the Clinical Trials Registry—India (CTRI/2018/04/013332, 18-04-2018).
Patients of either sex scheduled for unilateral THR meeting the selection criteria were recruited after obtaining written informed consent. The inclusion criteria were: American Society of Anesthesiologists physical status I and II, age 20–80 years, and body mass index 18–35 kg/m2. The exclusion criteria included patient-refusal, ASA III–IV patients, history of drug allergy to ropivacaine and fentanyl, coagulation disorders, cardiovascular, respiratory, neurological illness, uncontrolled diabetes mellitus, local or systemic Infection, aberrant anatomy of the landmarks, patients having hemodynamic instability, and pregnant and lactating women.
Fifty patients were randomly allocated to 2 groups using computer-generated random number table using coded sealed opaque envelopes. Group I (n = 25) received USG-LPB with 0.5% ropivacaine (15 mL) and Group II (n = 25) received CEA with 0.5% ropivacaine (15 mL).
Procedure for Group I
In the operating room, the patient was connected to 12-lead electrocardiography, non-invasive blood pressure cuff, and pulse oximeter. After obtaining baseline parameters, the patient was made to lie in the lateral position with the concerned side up and the hip and knees flexed. LPB was performed using the Shamrock method. An Ultrasound unit (Esaote MyLab OneTM, Maastricht, The Netherlands) with a 2–5 MHz, curvilinear microarray array probe was used. The patients were in the lateral decubitus position with the side to be anesthetized facing upwards. The transducer was placed in the transverse plane on the flank of the patient cranially to the iliac crest. The quadratus lumborum muscle was identified medial to the aponeurosis of the transversus abdominis muscle. The transverse process and vertebral body of L4 were identified and the pattern of a shamrock with 3 leaves was identified. The nerve roots were seen within the psoas muscle about 2 cm anterior to the transverse process. The transducer was shifted until the transverse process of L4 disappeared from the ultrasound image. The needle insertion was on the back of the patient, 4 cm lateral to the midline on a line representing the intersection of the ultrasound beam with the skin. A 20-gauge, 150 mm SonoPlex Stim cannula (Pajunk GmbH, Geisingen, Germany) was advanced in-plane and in the anterior direction. After the needle tip was positioned lateral to the L3 spinal nerve, electrical nerve stimulation (Stimuplex DIG/HNS11; B. Braun, Melsungen, Germany) was applied (0.1 ms impulse duration, 2Hz) to reduce the risk of intraneural needle tip positioning.
After local infiltration a volume of 15 mL, ropivacaine 0.5% was administered. A negative aspiration test together with a clear ultrasound visualization of the spread of the 5 mL bolus of ropivacaine 0.5% was mandatory prior to injection of the residual volume in order to reduce the risk of intravascular or subarachnoid injection. A perineural catheter was inserted 2 cm deeper than the needle tip. The catheter was used for continuous infusion of ropivacaine 0.2% with fentanyl 2 mcg/mL, at 5 mL/h after surgery.
The blocks were assessed by a temperature test, using an ice pack, repeatedly touching, and by loss of pin prick sensation, 15, 30, 45 and 60 minutes after the local anesthetic injection had been completed.
Motor block assessment was evaluated by the ability to extend the knee after the hip was passively flexed. Block success was determined 60 minutes after local anesthetic injection.
Procedure for Group II
For patients receiving epidural blockade, all patients were positioned in sitting position and the back was cleaned and draped with an antiseptic cleansing agent along with all universal precautions. Using the midline technique with a disposable 18 G Touhy’s needle epidural space was identified by loss of resistance to saline technique. After the identification of epidural space, the distance between the space and skin was noted by using the markings on the epidural needle. A disposable 20 gauge epidural catheter (PortexR, UK) was threaded through the needle into space 3–4 cm deeper than the needle tip and 15 mL of (0.5%) ropivacaine was injected through the catheter tip.
After placement of EA or LPB (confirmed by loss of pin prick sensation), all patients received a standard general anesthetic technique per departmental protocol. Induction was done using intravenous (i.v.) glycopyrrolate 0.2 mg, i.v. fentanyl 2 mcg/kg, i.v. propofol 2 mg/kg and i.v. vecuronium 0.1 mg/kg to facilitate endotracheal intubation. Anesthesia was maintained with isoflurane and N2O/O2 in a ratio of 60:40. After ensuring bilateral air entry, the endotracheal tube was secured. During the surgery, there was the provision to supplement fentanyl in the dose of 1 mcg/kg if there was 20% increase from the baseline parameters.
After induction, all patients received i.v. ondansetron 0.1 mg/kg. At the end of the procedure, the residual neuromuscular block was reversed with i.v. neostigmine 50 mcg/kg and glycopyrrolate 10 mcg/kg. Subsequently, a trachea was extubated and patients were shifted to post-anesthesia care unit.
Patients were connected to PCA (Master PCA, Fresenius Kabi, Finland) providing 0.2% ropivacaine plus 2 mcg/mL fentanyl as an analgesic in both the groups. The pump was set to deliver a continuous infusion of 5 mL/h of 0.2% ropivacaine and fentanyl with the provision of patient-controlled boluses of the same drug with a lock-out interval of 30 minutes. Time to the first bolus was taken during the study period and total drug consumption and any adverse effects were noted. Patient satisfaction using a visual analogue scale was noted at the end of the 48-hour study period.
Demographic (age, gender, comorbidities) and morphometric (height, weight) characteristics of participating patients were recorded. After the surgery, the pain was assessed using a numeric rating scale (NRS)5 at 1, 4, 12, 24, 36, 48 hours. All the observations (e.g., age, sex, vital parameters including NRS for pain, Bromage Score,6 occurrence of adverse effects, time to the first bolus, an total analgesic requirements) was recorded.
The primary outcome included NRS over 48 hours study period. Secondary outcomes included total postoperative analgesic consumption, patient satisfaction, motor power, and adverse effects.
Sample Size Calculation
From the pilot data, it was seen that the mean postoperative pain score in patients undergoing THR and receiving standard epidural analgesia over 48h using NRS was 2, with a standard deviation (SD) of 0.5. It was decided that a 20% reduction in postoperative pain would be considered as clinically meaningful difference, yielding a value of 1.6 with an SD of 0.5 as the mean postoperative pain score in the LPB group. Thus, for this study, sample size analysis with the above assumption and with a β error of 0.20 (i.e., power of 80%) and an alpha error of 0.05 demonstrated that a sample size of 25 per group would detect a 20% difference in mean postoperative pain score over 48 hours using NRS.
The statistical analysis was carried out using Statistical Package for Social Sciences (IBM Corp., Armonk, NY, version 22.0 for Windows). The primary outcome of the mean postoperative pain score over 48h was compared by Student’s t test. Continuous variables were tested for normal distribution using Kolmogorov–Smirnov test. To test for the significance of the difference between the two groups on single-measure data (patient satisfaction score at the end of 48 hours study period, and total postoperative analgesic consumption till 48 hours postoperatively), between-group comparisons was performed using Student’s t test for normally distributed continuous variables, Mann-Whitney U test for non-normally distributed continuous variables, chi-square test for binary variables, and Wilcoxon test for ordered categorical variables. For repeated-measures data assessment over time, including pain scores at rest and with activity, postoperative sensory and motor scores, heart rate, and blood pressure, two-way repeated-measures analysis of variance with post-hoc Scheffe’s test were used for analysis. The significance level was set at 0.05.
Results
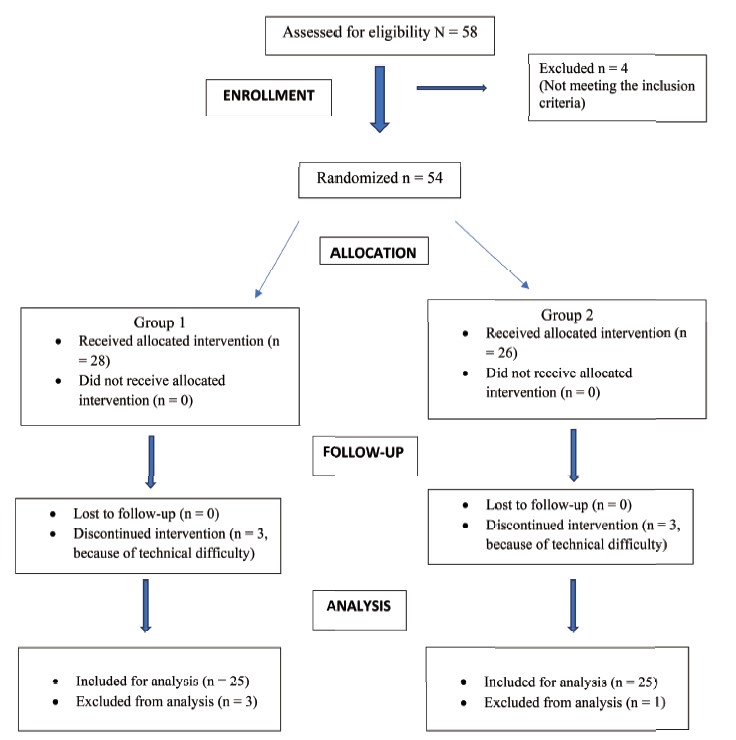
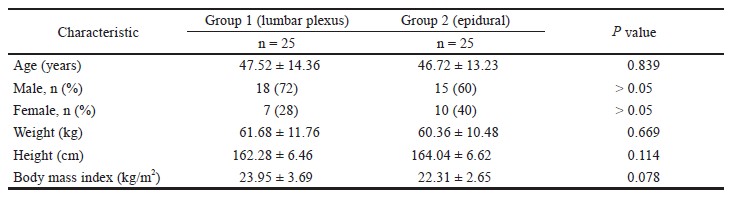
Fifty patients were recruited for the study. Figure 1 shows the CONSORT flow chart. The differences in demographic and baseline factors between the 2 groups were statistically not significant (Table 1).
Download full-size image
Download full-size image
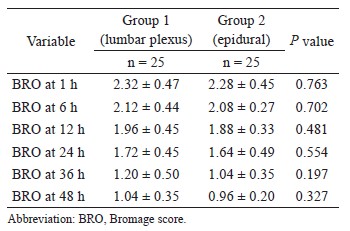
The mean modified Bromage score (BRO) on a scale of 0–3 was measured in both the groups. There was no statistical difference in the BRO up to 48 hours. The BROs are shown in Table 2.
Download full-size image
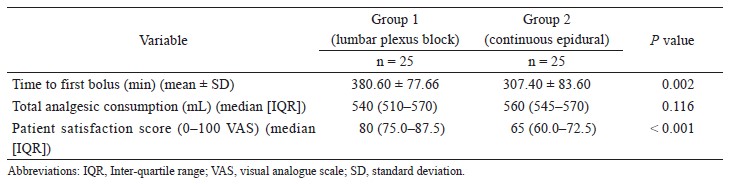
The mean time to the first bolus was significantly longer in the LPB group (380.60 ± 77.66 min) than the CEA group (307.40 ± 83.60 min) with P = 0.002 (Table 3).
Total mean ropivacaine consumption between the groups was comparable (LPB group, 540 mg; CEA group, 560 mg; P = 0.116 (Table 3).
Patient satisfaction was significantly higher in the LPB compared to the CEA group (median score, 80 vs. 66; P < 0.001) (Table 3).
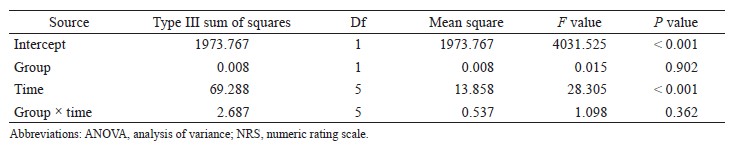
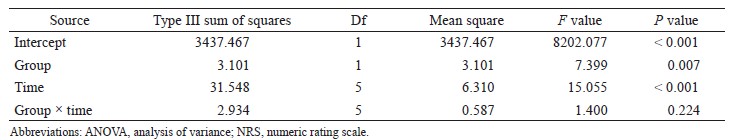
Download full-size image
There was no significant difference between the 2 groups regarding pain scores at rest (F value = 0.015; P = 0.902, Table 4) but there was a significant difference between NRS on the movement of the hip joint (F value = 7.399; P = 0.007) (Table 5). Within each group, the differences across various time points of observation were significant on rest (F value = 28.305; P < 0.001) and also on movement (F value = 15.055; P < 0.001). Group × time interaction was not significant for both NRS at rest (F value = 1.098; P = 0.362) and NRS at movement (F value = 1.400; P = 0.224), confirming the similar pattern of pain relief over time in the two groups (Tables 4 and 5).
Download full-size image
Download full-size image
The adverse effects noted were numbness in 2 of the 25 patients in the LPB group, and hypotension in 2 and numbness in 7 of the 25 patients in the epidural group.
Discussion
In this randomized controlled trial that compared USG-LPB with CEA for postoperative pain relief till 48 hours in patients undergoing THR, it was observed that patients in the LPB group took more than 1 hour longer than the epidural group to take their first additional analgesic dose compared with the CEA group. This is clinically meaningful besides being statistically significant. This indicates that the patients who underwent LPB were pain-free for a longer period than those with epidural block. This is the most important clinical finding of this study wit obvious clinical implications.
Total analgesic consumption was not significantly different between the 2 groups, though the trend favored the LPB group. The patient satisfaction was significantly higher in the LPB group. Hence overall the findings were more in favor of USG-PLB for THR in our study.
Postoperative pain, measured as the mean NRS score over 48 hours postoperatively, was comparable between the groups when assessed at rest. However, and importantly, the 2 groups differed significantly when pain on movement was compared using 48 hours mean postoperative NRS score, LPB group showing significantly less pain on movement. This is also very relevant clinically because the pain on movement emphasizes a dynamic relationship among the nervous system, pain processing, movement adaptations, and recovery. This is also what is really meaningful for the patients, and may have contributed to higher patient satisfaction in the LPB group.
Postoperative analgesia can be achieved by techniques such as i.v. patient-controlled analgesia with morphine, fentanyl, epidural, and continuous perineural blockade. Each has its own merits and demerits. The advantage of pain relief by continuous epidural is offset by the adverse effects such as urinary retention, hypotension, etc. LPB has emerged as an alternative approach for post-operative analgesia in patients undergoing THR and also for the patients in whom epidural is difficult or contra-indicated. Unilateral LPB is associated with fewer side effects, but the main concern with LPB is the experience of the concerned anesthetist. Important structures are present in the vicinity of the lumbar plexus (neuraxis, inferior vena cava, renal fasciae, and renal capsule).4 Further, an epidural spread of the local anesthetic is the most important complication of the LPB.7
The findings of the present study are in line with the existing literature,8-10 which shows that USG guided LPB is a good alternative to epidural block for the post-operative pain relief after THR surgery. Fentanyl used as an adjuvant increases the duration and quality of analgesia.
In this study, no severe post-operative adverse effects were noted in either group. Only 2 patients had numbness in the LPB group while 2 had hypotension and 7 patients had numbness in the epidural group. Probably, local anesthetic injected under real-time visualization using ultrasonography might have avoided side effects and fatal complications.
This finding thus reiterates the importance of using ultrasound guidance for nerve blockade. LPB should be avoided in the anticoagulated patient. Renal capsular hematoma has been described after the block at L-3 level11 hence the block was performed at L-4 level. Overall, the findings of this study enhance confidence in the safety of the USG-LPB procedure is carried out by the experienced personnel. However, long term studies with a bigger sample size are needed to further confirm the safety aspect.
The strengths of this study are that it was a prospective, randomized, clinical trial. Randomization is essential in clinical trials to establish a cause and effect relationship for an intervention. The sample size was calculated a priori, and the adequate number of patients was enrolled for the study. Also, strict inclusion and exclusion criteria were followed during patient selection.
There were a few limitations to this study. First, it included only ASA physical status I and II patients, and the results of the study cannot be applied to patients of a higher grade of ASA physical status. Second, it did not include the measurement of serum ropivacaine and serum fentanyl levels. Third, the length of hospital stay and the evaluation of long term benefits of pain relief would have been more valuable and would have added more strength to the study. Fourth, the sensory block was not assessed using repeated neurological examination due to difficulty in assessing sensory block after surgery so the first analgesic request was used as a proxy measure for the end point of sensory block. Further trials with a longer study period assessing the 2 techniques could be done in the future. However, none of these limitations can invalidate the major findings of this study within the limits of their applicability and interpretability.
In conclusion, LPB can be used as an equally effective alternative to EA combined with general anesthesia for post-operative analgesia after THR. LPB may be a tangible alternative in patients in whom epidural is difficult (e.g., in ankylosing spondylitis). The utility of USG-LPB needs to be corroborated in future multicentre studies with a robust sample size.
References
| 1 |
Chung F, Ritchie E, Su J.
Postoperative pain in ambulatory surgery.
Anesth Analg. 1997;85(4):808-816.
|
| 2 |
Rawal N.
Epidural technique for postoperative pain: gold
standard no more?
Reg Anesth Pain Med. 2012;37(3):310-
317.
|
| 3 |
De Tommaso O, Caporuscio A, Tagariello V.
Neurological complications following central neuraxial blocks: are there predictive factors?
Eur J Anaesthesiol. 2002;19(10):705-
716.
|
| 4 | |
| 5 |
Jensen MP, McFarland CA.
Increasing the reliability and validity of pain intensity measurement in chronic pain patients.
Pain. 1993;55(2):195-203.
|
| 6 |
Breen TW, Shapiro T, Glass B, Foster-Payne D, Oriol NE.
Epidural anesthesia for labor in an ambulatory patient.
Anesth Analg. 1993;77(5):919-924.
|
| 7 |
Enneking FK, Chan V, Greger J, Hadzić A, Lang SA, Horlocker TT.
Lower-extremity peripheral nerve blockade: essentials of our current understanding.
Reg Anaesth Pain Med. 2005;30(1):4-35.
|
| 8 |
Costa GM, Carvalho IM, Castro AI, Lages NC, Correia CM.
Postoperative analgesia for hip arthroplasty: comparison of continuous lumbar plexus block and epidural analgesia.
Rev Dor. 2016;17(1):2-7.
|
| 9 |
Türker G, Uçkunkaya N, Yavaşçaoğlu B, Yilmazlar A, Özçelik S.
Comparison of the catheter-technique psoas compartment block and the epidural block for analgesia in partial hip replacement surgery.
Acta Anaesthesiol Scand. 2003;47(1):30-36.
|
| 10 |
Touray ST, de Leeuw MA, Zuurmond WW, Perez RS.
Psoas compartment block for lower extremity surgery: a meta-analysis.
Br J Anaesth. 2008;101(6):750-760.
|
| 11 |
Aida S, Takahashi H, Shimoji K.
Renal subcapsular hematoma after lumbar plexus block.
Anesthesiology. 1996;84(2):452-455.
|