To the Editor,
Failed back surgery syndrome (FBSS) was defined as a clinical term used to describe those patients who had recurrent or persistent low back or leg pain after received a spinal surgery or the outcome of spinal surgery do not meet the expectations of the patients and surgeon.1,2 Caudal epidural steroid injection (CESI) was considered as a treatment option for patients suffering from FBSS.3,4 CESI was a relatively safe procedure especially injected with ultrasound-guided.5,6 Severe complications, such as transient paraplegia, arachnoiditis, and hematomas, are still published.7,8 Here, we described a rare case with a discordant subdural hematoma after ultrasound-guided CESI.
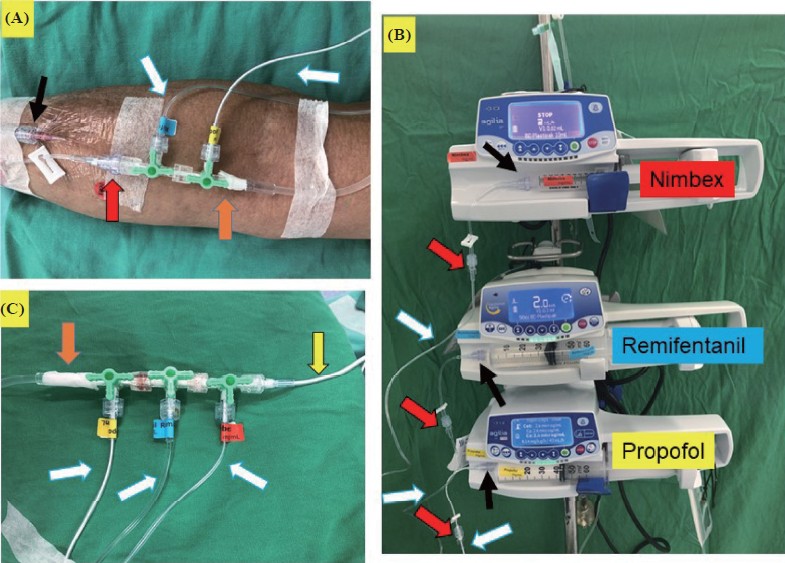
A 78-year-old female had the history of degenerative disc disease and lumbar spine compression fracture and received second spinal operations about 20 months ago (T12–L3 posterior fusion and laminectomy plus L2–3 and L4–5 discectomy, fi rst spine operation performed about 7 years ago). She was also comorbid with diabetes and hypertension under regular control. Her first visit to our pain clinic was 18 months ago for severe low back and leg pain even after the spinal operation. Lumbar spine X-ray revealed posterior fusion and bone cement leakage since then. Anticonvulsants, antidepressants, non-steroidal anti-infl ammatory drugs, and weak opioid were all given but her visual analogue scale (VAS) were still high around 6–8/10. She received 5 times ultrasound-guided CESI before (each injection was between 3 and 4 months) with excellent improvement and VAS was decreased to 2–3/10 for every injection. This time, she came to our pain clinic with her recurred low back pain (VAS = 8–10/10) and we arranged another ultrasound-guided CESI as before. Pre-injection physical examination revealed bilateral radiculopathy with slight paresthesia over L3 or L4 dermatome and mild weakness of bilateral leg muscle power with a grading between 4 and 5. She still can walk with a cane for her daily life. Her blood coagulation test for the caudal injection was within a normal range. As the procedure begins, she was in a prone position with a pillow under her abdomen. We introduced a 23 G spinal needle and punctured through the sacrococcygeal ligament under ultrasound in-plane technique (Figure 1A). Then, we pushed a 14 mL injectate (triamcinolone acetonide 40 mg plus 0.1% levobupivacaine) via syringe by hand and checked the injectate with ultrasound color flow mapping (Figure 1B). No red fluid (blood) was found before injection. At first, she complained of severe sharp pain and tingling when injectate pushed. We stop the injection process and adjusted the needle position immediately. The rest injectate was then given after we mildly pull out the needle under ultrasound monitoring. The tingling pain was decreasing during the second injection and we completed the CESI treatment. Unfortunately, she complained of bilateral radiation pain and weakness on both legs just after we finished CESI. Immediately physical examination revealed bilateral radiation pain from buttock to posterior and lateral legs and both legs muscle power grading was decreased to 3–4/5 (lift off the bed) but no urinary incontinence. We then closely monitor the patient’s neurological condition and vital signs for several hours. Because her neurological symptoms were not improved, we arranged a lumbar magnetic resonance imaging survey and revealed the subdural hematoma at the level of L5–S1 junction (Figure 2A). We explained the fi nding to the patient and the decompression operation possibility concomitantly. She initially received oral pain analgesics for her discomfort. Fortunately, her muscle power improved to 4–5/5 on the next day and symptoms subsided. She was still regularly followed up in our pain clinic.
Download full-size image
In (A), the yellow arrow illustrates 23 G spinal needle, and the white arrow represents the apex of sacral hiatus. In (B), steroid with local anesthetic injectate through the spinal needle was found in the caudal epidural space under ultrasound color flow mapping.
Download full-size image
(A) presents 2 magnetic resonance imaging cutting image for the location of the subdural hematoma (yellow arrow at the level of L5–S1). (B) presents the previous 4 safe caudal injections with no significant difference in ultrasound color flow mapping.
Spinal subdural hematoma (SSDH) was a rare complication and only found after neuraxial anesthesia rather than pain control.9 Caudal injection-induced SSDH had not been reported yet. There is one report described a discordant lumbar epidural hematoma after caudal steroid injection but not subdural.10 They thought that the possible reasons for epidural hematoma may be coagulopathy, high spinal canal pressure, or interventional violence. Our patient had no coagulopathy by history and CESI was performed under an in-plane ultrasound technique with no significant ultrasound color flow image change during injections (Figure 2B). And the location of this SSDH has some distance for our puncture site (SSDH at a level near lumbosacral junction rather than sacral hiatus) plus the subdural space is quite narrow and almost avascular. The direct subdural puncture induced hematoma is less likely. Therefore, we thought that the high pressure-induced blood vessels rupture during CESI has a high possibility for this event. Certainly, subtle vessel weakness due to previous spinal surgery with several CESI may predispose this SSDH. But the real true mechanism of this SSDH may need more surveys.
The etiology of SSDH was divided into traumatic, coagulopathy-related, vascular malformation, tumors, infection, and iatrogenic.10 Cranial/spinal surgery and invasive spinal procedures attributed to iatrogenic SSDH.9 Pathogenesis of spinal procedure-related SSDH remains unclear but could theoretically be direct or indirect to vascular injury. Interestingly, the indirect rupture of spinal vessels was caused via the sudden increase of abdominal or thoracic pressure11 which may resemble CESI. Although this hypothesis has not been proven, it reminds us that even minor pressure change within the spine canal may cause SSDH if the structure is abnormal.
The remote spinal SSDH after CESI may be caused by the rupture of small extra-arachnoid vessels on dual surface12 which may be induced by the high pressure within the spinal canal when we pushed the caudal injectate. A case with remote retinal vascular rupture was also reported and may be caused by the sudden increase in epidural pressure.13 About the Injection pressure monitor during CESI, few data discuss this issue but one paper demonstrated that epidural pressure increase to 70–80 mmHg for patients with either herniated disk or spinal stenosis compared with 40 mmHg for normal patients.14 Further research for the epidural injection pressure is needed to solve this issue.
CESI is easy and safe alternative for FBSS but the neurological complications should be closely monitored during or after this procedure, especially when the spinal structure was changed. Once neurological symptoms occurred, stop the injection immediately, and rechecked the injectate is indicated. Once spinal SSDH happened, the conservative management strategy may be considered as a close neurological monitor. But percutaneous drainage and surgical evacuation were also be considered according to the patient’s clinical severity.15
References
| 1 |
Thomson S.
Failed back surgery syndrome—definition, epidemiology and demographics.
Br J Pain. 2013;7(1):56-59.
|
| 2 |
Daniell JR, Osti OL.
Failed back surgery syndrome: a review article.
Asian Spine J. 2018;12(2):372-379.
|
| 3 |
Manchikanti L, Singh V, Cash KA, Pampati V, Datta S.
Fluoroscopic caudal epidural injections in managing post lumbar surgery syndrome: two-year results of a randomized,double-blind, active-control trial.
Int J Med Sci. 2012;9(7):582-591.
|
| 4 |
Bansal K, Dahuja A, Bhowmik S, Gupta M, Rashmeet.
Role of caudal epidural injection in managing failed back syndrome: one year follow up result of a randomized study.
Int J Contemp Med Res. 2017;4(1):208-211.
|
| 5 |
Dawkins CJM.
An analysis of the complications of extradural and caudal block.
Anaesthesia. 1969;24(4):554-563.
|
| 6 |
Kao SC, Lin CS.
Caudal epidural block: an updated review of anatomy and techniques.
Biomed Res Int. 2017;2017:9217145.
|
| 7 |
Kim DH, Kim HJ.
Cauda equina syndrome following epidural adhesiolysis in a patient with spinal stenosis.
Korean Continence Soc. 2003;7(1):46-49.
|
| 8 |
Nanjayan SK, Swamy GN, Yallappa S, Bommireddy R.
Arachnoiditis following caudal epidural injections for the lumbo-sacral radicular pain.
Asian Spine J. 2013;7(4):355-358.
|
| 9 |
Riley CA, Spiegel JE.
Complications following large-volume epidural blood patches for postdural puncture headache. Lumbar subdural hematoma and arachnoiditis: initial cause or final effect?
J Clin Anesth. 2009;21(5):355-359.
|
| 10 |
Choi JJ, Chang YJ, Jung WS, Lee KC, Kim JH, Jo YY.
Discordant lumbar epidural hematoma after caudal steroid injection: a case report (CARE-compliant).
Medicine (Baltimore). 2017;96(24):e7127.
|
| 11 |
Rader JP.
Chronic subdural hematoma of the spinal cord: report of a case.
N Engl J Med. 1955;253(9):374-376.
|
| 12 |
Kakitsubata Y, Theodorou SJ, Theodorou DJ, et al.
Spontaneous spinal subarachnoid hemorrhage associated with subdural hematoma at different spinal levels.
Emerg Radiol. 2010;17(1):69-72.
|
| 13 |
Gill JB, Heavner JE.
Visual impairment following epidural fluid injections and epiduroscopy: a review.
Pain Med. 2005;6(5):367-374.
|
| 14 |
Dunbar SA, Manikantan P, Philip J.
Epidural infusion pressure in degenerative spinal disease before and after epidural steroid therapy.
Anesth Analg. 2002;94(2):417-420.
|
| 15 |
Lee JI, Hong SC, Shin HJ, Eoh W, Byun HS, Kim JH.
Traumatic spinal subdural hematoma: rapid resolution after repeated lumbar spinal puncture and drainage.
J Trauma. 1996;40(4):654-655.
|