Outline
Abstract
Background: The choice between a double-lumen tube (DLT) and a bronchial blocker (BB) for lung isolation remains controversial. The aim of this study was to determine if the features of these lung isolation devices affect postoperative pulmonary outcomes.
Methods: We retrospectively identifi ed claims by patients who underwent surgery under lung isolation in 2000–2012 in the Taiwan National Health Insurance Research Database. Afte matching for age, sex, and year of surgery, 1,898 patients were enrolled in a BB group and 5,694 in a DLT group. The risks of readmission in the first postoperative year with pulmonary complications in-hospital death, and one-year mortality were estimated using conditional logistic regression analysis.
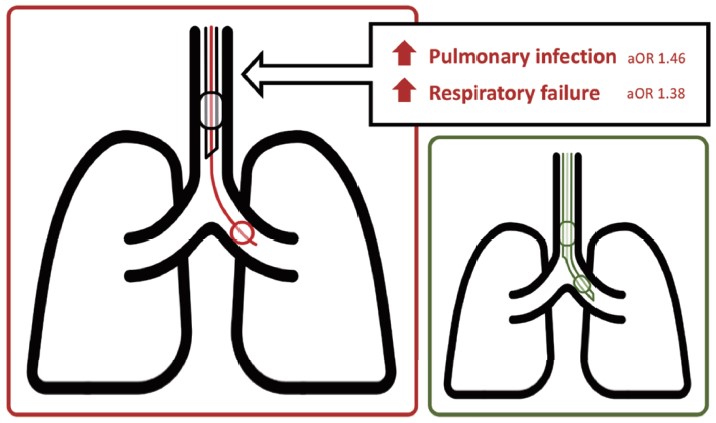
Results: Patients in the BB group had higher risks of readmission with pulmonary infection (adjusted odds ratio [aOR], 1.46; 95% confidence interval [CI], 1.22–1.74) or respiratory failure (aOR, 1.38; 95% CI, 1.09–1.76) in the first postoperative year as well as in-hospital deat (aOR, 2.03; 95% CI, 1.40–2.94) and one-year mortality (aOR, 1.94; 95% CI, 1.60–2.35) than those in the DL group after adjustment for the types of the surgeries, hospital accreditation level, underlyin comorbidity, and a potentially diffi cult airway. Patients in the BB group had longer median (interquartile range) stay in the intensive care unit (1 [0–4] vs. 1 [0–3] days, P < 0.001) and in hospital (16 [10–26] vs. 13 [8–22] days, P < 0.001).
Conclusion: Patients undergoing thoracic surgery are more likely to experience postoperative pulmonary complications if a BB than a DLT is used.
Keywords
bronchial blocker, double-lumen tube, lung separation, postoperative outcomes
Introduction
Lung isolation was first described in 1931 as a solution to potentially fatal pneumothorax.1 Onelung ventilation is used routinely in thoracic surgery, particularly in video-assisted thoracoscopy surgery, to improve the visibility of the surgical field. Satisfactory lung isolation can be achieved using a double-lumen tube (DLT) or a bronchial blocker (BB). Both devices have been in clinical use for decades, but controversy persists regarding which device is superior.2-7 A BB can be added to a regular tracheal tube and is the preferred device for patients in whom a difficult airway is anticipated.8-12 In contrast, the DLT has been used widely for lung separation since the 1950s when its introduction by Carlens was considered as a milestone in thoracic anesthesia.13 A DLT can be easily, rapidly, and accurately inserted, but there is concerned with the risks of tracheobronchial injury.14-18 The final choice between the two devices is usually made according to the status of the patient and the experience of the practitioner.
Some important information remains unclear with regard to the use of these lung isolation devices. First, the basic characteristics of patients in whom a DLT or a BB is used for one-lung ventilation management in contemporary thoracic surgery are not clear. Second, the association between these different airway devices and postoperative pulmonary complications is not yet known.
It has long been debated whether a BB or a DLT is the better choice. In cases without strong indications, the preferences of the surgeon and anesthesiologist influence selection of the lung isolation device. In spite of widespread agreement that a BB is a reasonable option as a lung isolation device, the overwhelming preference has been for a DLT because of its cost-effectiveness, ability to allow rapid intubation, and reliable features.19-21 It is believed that a BB is of comparable quality in terms of lung deflation, but intraoperative displacement occurs more frequently with a BB than with a DLT22 and may incidentally re-expand the lung undergoing surgery. In addition, the lack of a lumen in a BB for suctioning of blood or secretions may expose the contralateral lung to contamination. We hypothesised that these flaws in a BB may be associated with pulmonary infection or further adverse postoperative outcomes.
Methods
Study Design and Data Source
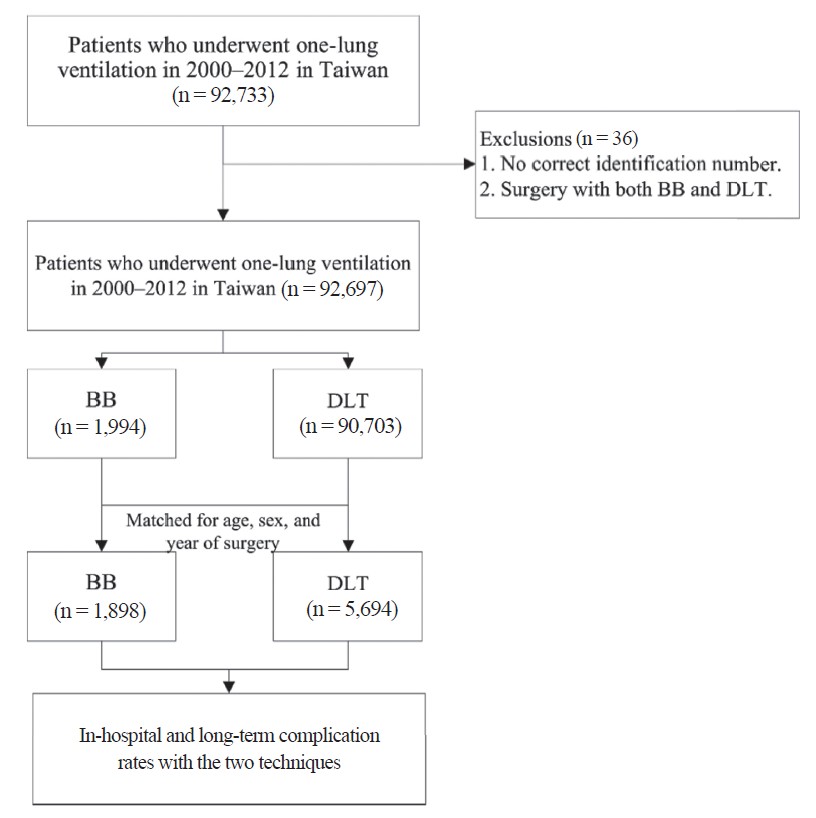
Using the population-based nationwide insurance database in Taiwan, we designed a matched-pairs study controlling for patient age, sex, and year of surgery to investigate and estimate the relative risks of adverse postoperative outcomes including pulmonary infection, respiratory failure, and mortality associated with use of DLTs and BBs for one-lung ventilation (Figure 1).
Download full-size image
Abbreviations: BB, bronchial blocker; DLT, double-lumen tube.
The data used in this study were collected from the inpatient claims database for 2000–2012 released by the National Health Insurance Research Dataset (NHIRD) in Taiwan. The Taiwan National Health Insurance Program was launched in 1995 and by 2011 covered more than 99% of the population.23,24 The high coverage rate makes the NHIRD one of the largest population-based databases in the world. The accuracy of the advers event records held in this database, including those for ischemic stroke, acute myocardial infarction, and in-hospital mortality, has been validated elsewhere.25-28 The database provides an encrypted identification number for each patient as well as age, sex, admission details, and International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for diagnoses and procedures. All secondary data are de-identified. The protocol for this study was granted exemption from full review by the Institutional Review Board of Chi Mei Medical Center, Tainan, Taiwan (Chairperson Prof. Chung-Hsi Hsing) on 25 May 2016 (IRB-10505-E05) in view of the anonymity of the data. The need for informed consent was waived for the same reason.
Patients
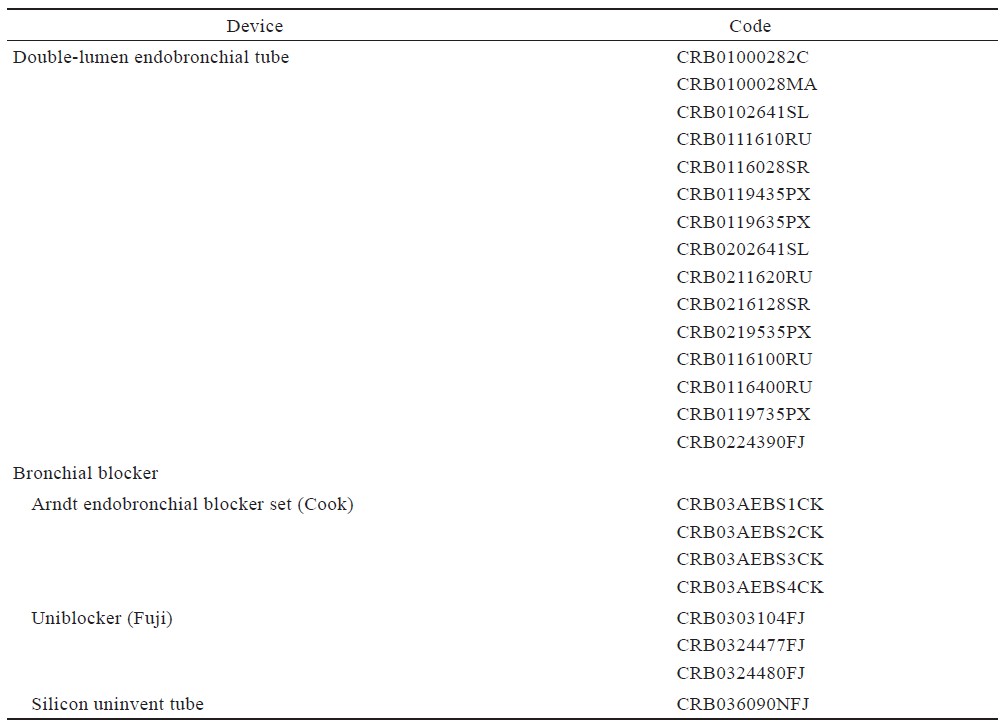
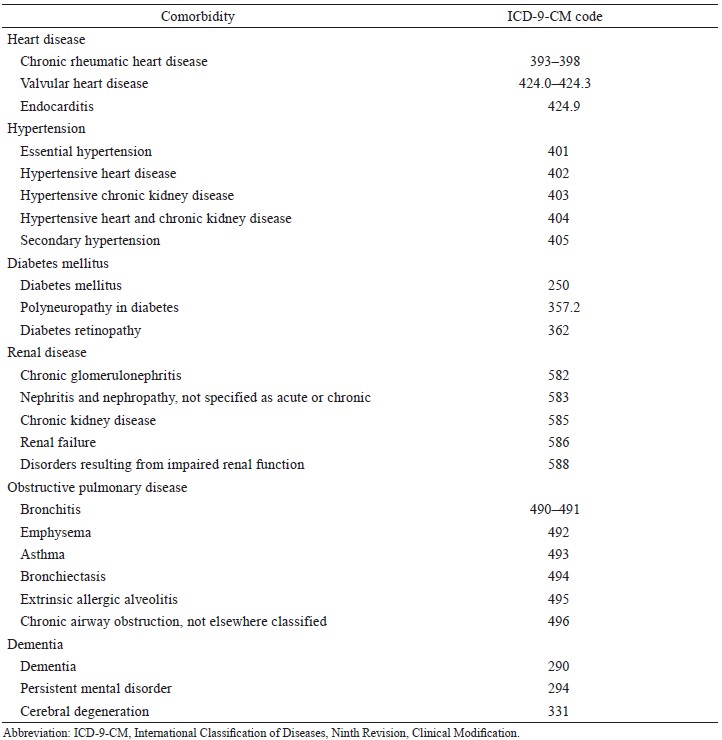
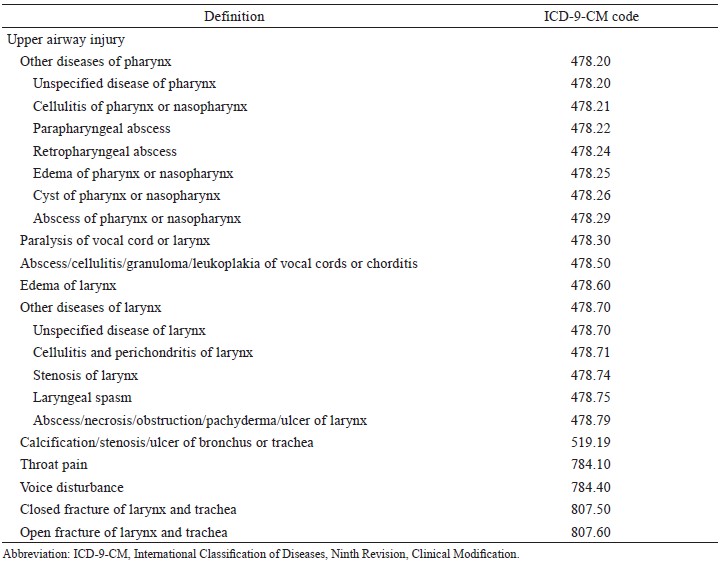
This retrospective, nationwide, population-based study included patients identified to have undergone a surgical procedure in 2000–2012 that included lung separation by placement of a BB or a DLT (Figure 1). The codes for the lung isolation devices used were identified (Supplement Table 1). To eliminate any influence of previous surgical events, only first inpatient surgical procedures that included lung isolation were collected. Cases with missing data or a record of multiple isolation devices being used for the same surgical procedure (i.e., charges for both a DLT and a BB) were excluded. Each patient in whom a BB was used was matched for age, sex, and year in which the surgery was performed with 3 randomly selected patients in whom a DLT was used. Patient age was classified as younger than 50 years, 50–64 years, or older than 65 years. The lung isolation technique was classified as being performed during pneumonectomy, lobectomy, segmentectomy, local excision, other pulmonary surgery, oesophageal surgery, cardiac surgery, vascular surgery, or other types of the surgeries. Pre-existing comorbidities determined from medical claims within the 3 years before surgery included heart disease, hypertension, diabetes mellitus, renal disease, obstructive pulmonary disease (chronic obstructive pulmonary disease or asthma), and dementia (Supplement Table 2). Patients readmitted to the hospital in the following year with upper airway injury recorded as one of the admission diagnoses were considered a possibly difficult airway (Supplement Table 3). The modified Charlson Comorbidity Index (CCI)29 was used as a surrogate for the American Society of Anesthesiologists physical status classification to indicate individual health status30,31 and was presented as the mean and standard deviation. The hospital accreditation level was also considered. According to the Taiwan Joint Commission on Hospital Accreditation, local Taiwanese hospitals with fewer than 300 beds provide primary medical care, whereas regional hospitals with 301–999 beds provide secondary care, and medical centers with 1,000–2,500 beds provide research facilities and are responsible for most of the staff training burden and tertiary medical care.
Outcomes
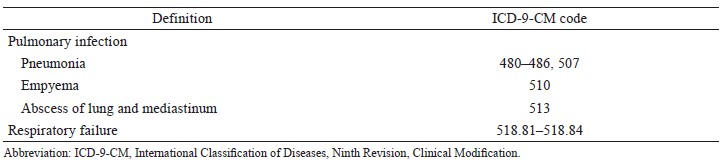
The primary outcomes were readmission within the first postoperative year with a diagnosis of pulmonary infection or respiratory failure (Supplement Table 4). The secondary outcomes were in-hospital mortality and one-year mortality after the index surgery. In-hospital mortality was identifi ed using the “in-hospital death” code at discharge or withdrawal from the National Health Insurance Program within 30 days after discharge because of the custom of choosing the “die at home” option in Taiwan. Enrolment in the National Health Insurance Program is mandatory and is withdrawn within 30 days of death. After index surgery, both primary and secondary outcomes were traced monthly for six months. The duration of ventilator support, length of stay in hospital, and duration of stay in the intensive care unit were also compared between the two study groups.
Statistical Analysis
Descriptive statistics and standardised differences were used to compare the relative balance of patient information in the DL group and the BB group. Patient characteristics as potential confounders associated with postoperative outcomes were included as covariates in the predicted model to evaluate the relative risks associated with the use of a DLT or a BB. The use of standardised differences32,33 indicated that the balance between the groups with regard to the types of the surgeries performed, hospital accreditation level, and underlying health status indicated by the CCI score and other comorbidities was acceptable. Conditional logistic regression analyses adjusted for the surgical procedure performed, hospital accreditation level, CCI score, and underlying comorbidities as well as a possibly difficult airway were performed to compare the risks of adverse postoperative outcomes between the two groups using the odds ratio (OR) and 95% confidence interval (CI). Correlations were considered statistically significant at P < 0.05. The detectable OR of 1.3 between cases and controls was estimated at 90% statistical power and the probability of type I error at 0.05. Statistical analyses were performed using SAS version 9.4 software (SAS Institute Inc., Cary, NC, USA).
Results
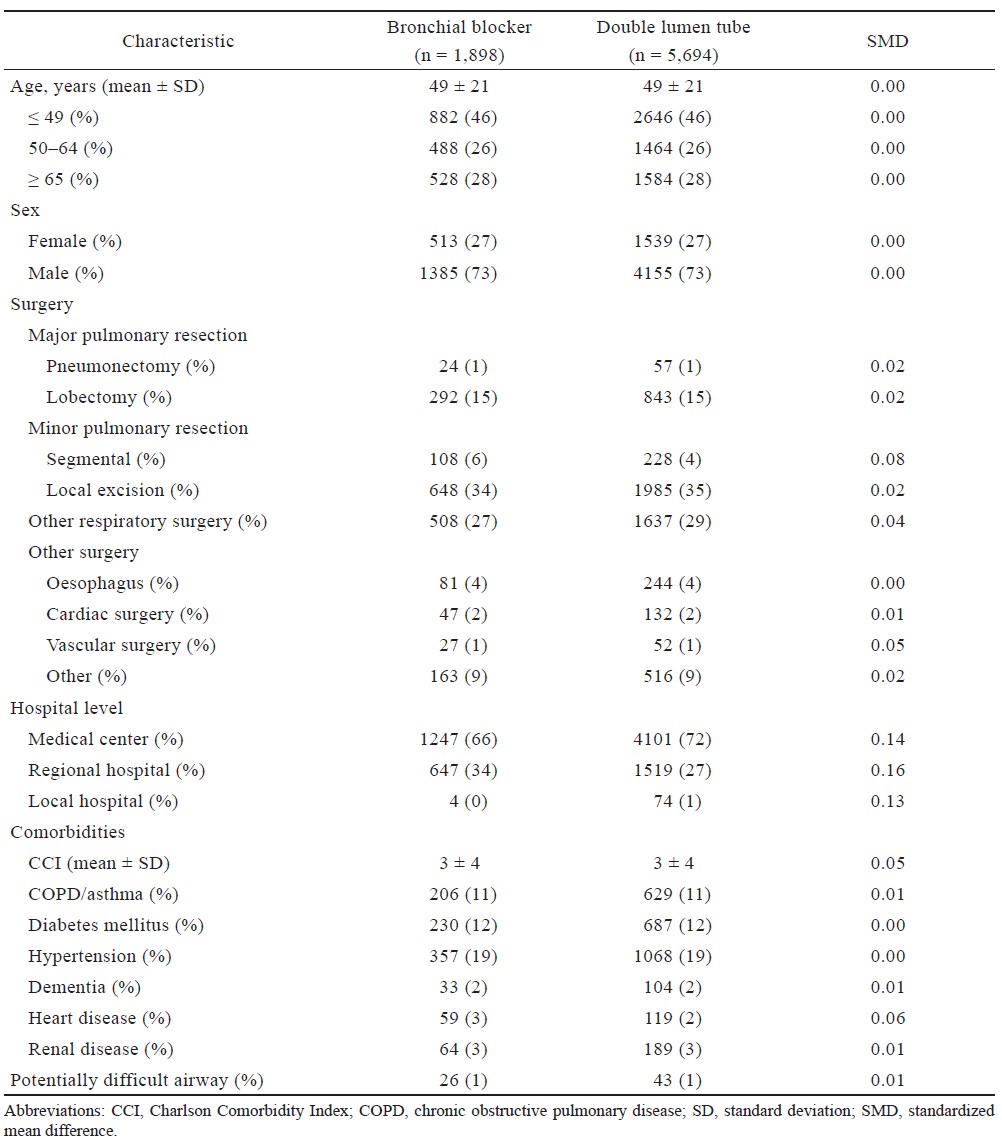
A total of 92,697 patients were identified to have undergone lung isolation; a DLT was used in 90,703 cases (98%) and a BB in 1,994 (2%). After matching for age, sex, and year of surgery, 1,898 patients were enrolled in the BB group and 5,694 in the DLT group (Table 1). All patients were tracked to identify any adverse events within the first postoperative year. The mean patient age was 49 ± 21 years and 73% of the patients were male.
Download full-size image
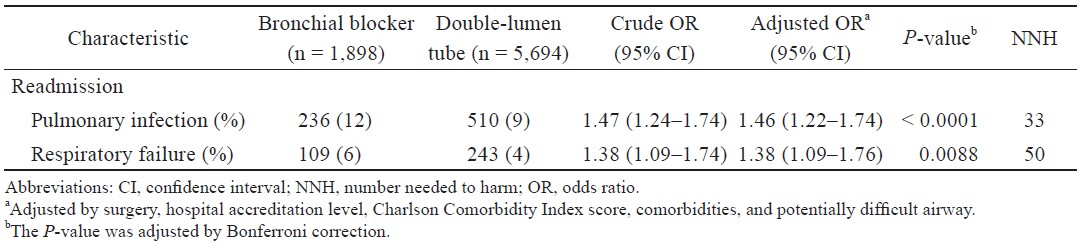
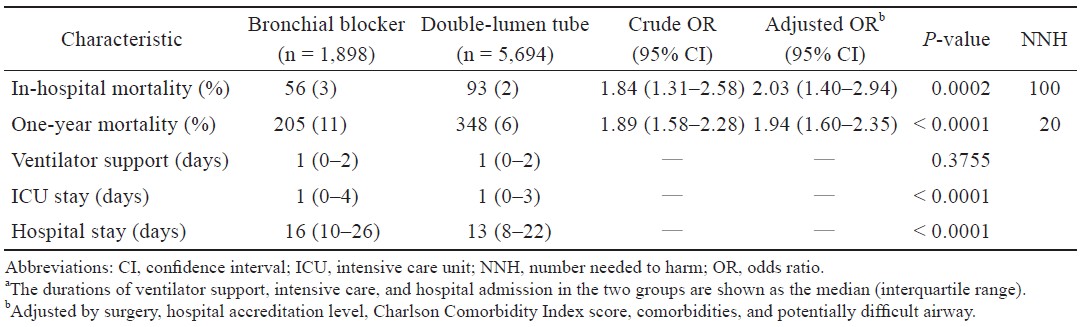
Patients in the BB group had a significantly higher risk of readmission for pulmonary infection (adjusted OR [aOR], 1.46; 95% CI, 1.22–1.74; P < 0.0001) or respiratory failure (aOR, 1.38; 95% CI, 1.09–1.76; P = 0.0088) in the first postoperative year after adjustment for potential confounders, including the types of the surgeries, hospital accreditation level, CCI score, underlying comorbidities, and a potentially difficult airway (Table 2). Higher rates of in-hospital death (aOR, 2.03; 95% CI, 1.40–2.94; P = 0.0002) and mortality in the first year following the index admission (aOR, 1.94; 95% CI, 1.60–2.35; P < 0.0001) were also found in the BB group after adjustment for confounding factors (Table 3). In addition, patients in the BB group had longer median stays in the intensive care unit and in hospital than those in the DLT group (1 [interquartile range 0–4] vs. 1 [0–3] day and 16 [10–26] vs. 13 [8–22] days, respectively, both P < 0.0001).
Download full-size image
Download full-size image
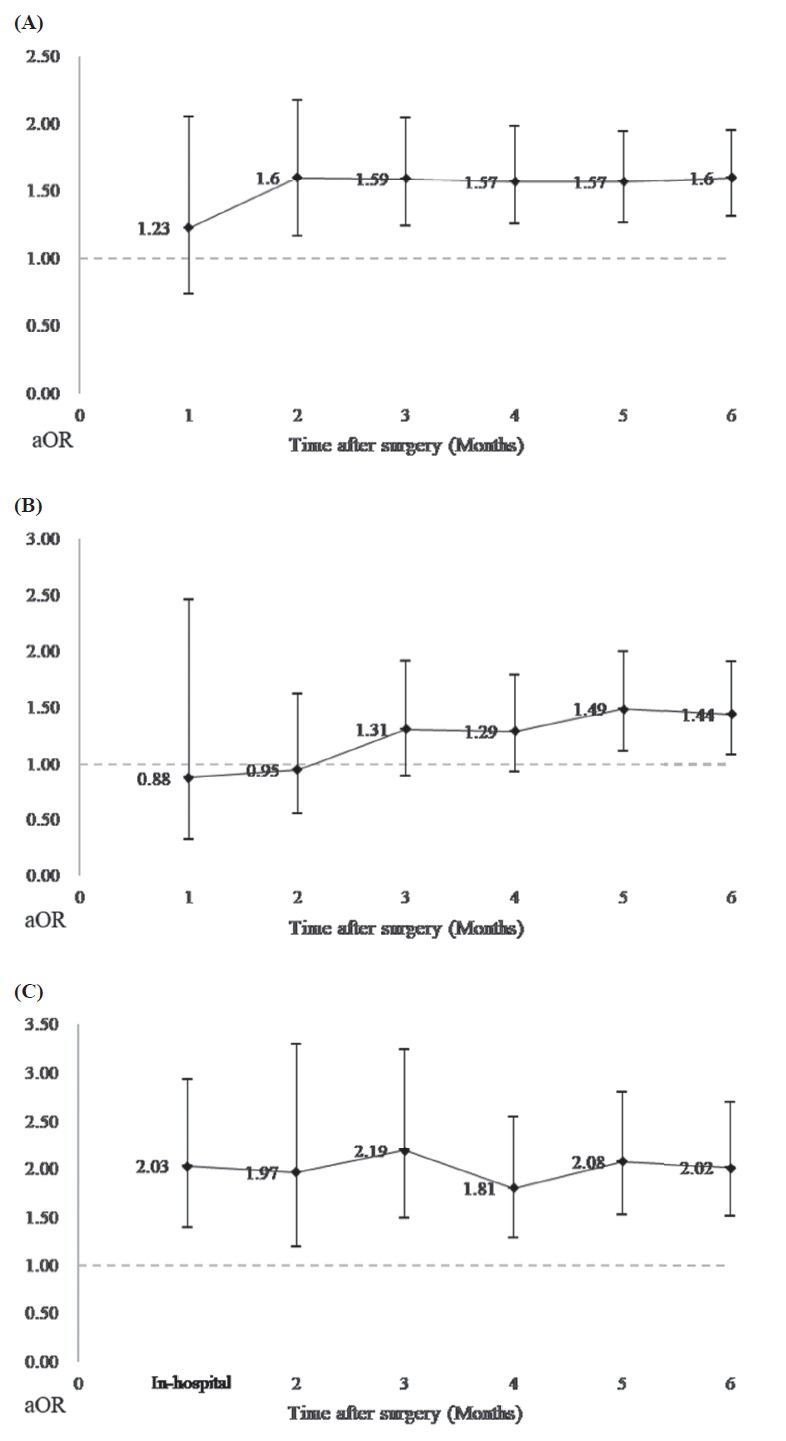
Outcomes were traced monthly after index surgery for up to 6 months (Figure 2). A significantly increased the risks of pulmonary infection was noted in the second month and of respiratory failure in the fifth month. Among the secondary outcomes, significant mortality was noted during the entire 6 months.
Download full-size image
Discussion
In this study, we undertook a large-scale comparison of the adverse postoperative outcomes associated with the use of DLTs and BBs. The data presented here indicate a significant correlation between the use of a BB for lung isolation and an increased risk of adverse postoperative events, including readmission with pulmonary infection, or respiratory failure within 1 year, as well as in-hospital death and one-year mortality after the index surgery.
Despite the advent of the BB, the DLT is still widely preferred for one-lung ventilation.7 The first section of this study describes the use of airway devices for one-lung ventilation in Taiwan. A DLT was used to achieve lung isolation in the majority of cases during the study period. This could be explained in part by the restricted claim rule for a BB implemented by the National Health Insurance Program in Taiwan. DLTs are also preferred by practitioners in other countries; over 96% of Italian, British and German surgeons used a DLT for one-lung ventilation during routine thoracotomy.19-21
BBs are widely accepted as a solution to potential upper airway problems in patients with a difficult airway. However, we have found an association between the use of a BB and the diagnosis of upper airway injury in the following year. This association may have been confounded by a predisposition to injury resulting from the airway abnormalities that led to the choice of the BB, and we considered this a possible confounding factor in our statistical model.
Known drawbacks of BBs include longer time to secure lung isolation22,34,35 and slow deflation of the lung, but the quality of lung isolation achieved is similar with both devices once the lung is fully deflated.22,36,37 A substantial body of literature has addressed practical differences between the two devices during the perioperative period,35,38,39 but there has been little research on their contribution to postoperative outcomes. Intraoperative displacement is a serious problem that occurs more frequently with a BB than with a DLT22 and might incidentally re-expand the operative lung and interfere with the surgery. Very serious consequences might result if herniation of the BB balloon into the trachea or contralateral bronchus is not recognised.40 The lack of a channel precludes adequate suctioning of the operative lung, potentially exposing the healthy lung to contamination. These features of the BB may have contributed to the higher rate of adverse pulmonary outcomes reported here. Patients in the BB group had a higher risk of readmission for pulmonary infection or respiratory failure in the year following discharge than their counterparts in the DLT group (Figure 3). In-hospital and one-year mortality rates were also higher in the BB group; however, the relationship is unclear because of the lack of detailed information on causes of death.
Download full-size image
Abbreviation: aOR, adjusted odds ratio.
Patients in the BB group were likely to remain longer in the intensive care unit and in hospital, which is compatible with the finding of poorer outcomes in this group. Although the stay in the intensive care unit was only slightly longer in the BB group, the median hospital admission time was 3 days longer in this group than in the DLT group (16 days vs. 13 days), suggesting a greater likelihood of further episodes of infection and higher medical costs.
This study has some limitations. The first concerns the quality and completeness of the data. The codes recorded in the database were reviewed and validated by auditors to ensure the accuracy of the claims. However, not all relevant supplementary information was entered into the database. Potential confounders, such as body mass index, socioeconomic status, environmental factors, postoperative pain scale scores, types of BBs, sizes, and sides of DLTs could not be identified. In terms of specific concerns about the condition of the airway, patients readmitted in the following year with a diagnosis of upper airway injury were considered as possible difficult airway cases, and we adjusted our model for this potential effect. Second, although some comorbidities were adjusted for in the conditional regression model, we could not control all underlying diseases. American Society of Anesthesiologists physical status classification data were not available in the database. Therefore, the CCI score, which has been validated as an independent predictor of postoperative complications and mortality,30,31 was used as a surrogate. Third, it was not possible to determine the temporal relationship between thoracic surgery with lung isolation and in-hospital adverse events using cross-sectional analyses, so we could not differentiate between in-hospital complications and co-existing diseases. Therefore, with the exception of postoperative mortality, in-hospital adverse outcomes were excluded from our analyses. Nevertheless, we were able to trace readmission with pulmonary complications by month following the index surgery for up to six months to ascertain when significant differences between the devices emerged. Finally, this study was further limited by its retrospective design. Although selection bias could not be completely avoided, it was decreased as much as possible at the study design stage.
A randomised controlled trial comparing patient safety between the cohorts using the two devices could rectify some of these limitations. Nevertheless, despite its limitations, the large nationwide dataset that we used supports statistically robust conclusions. Further comprehensive research is needed to validate our results, preferably including a large international database. We consider our findings intriguing enough to warrant further investigations that might improve perioperative management and advance the quality of thoracic anesthesia.
In summary, there seems to be a relationship between the use of a BB for lung isolation and an increased risk of adverse postoperative events, including readmission with pulmonary infection or respiratory failure within the fi rst postoperative year, and an increased risk of in-hospital death and one-year mortality. The durations of intensive care unit stay and hospital admission were longer in patients who underwent lung isolation using a BB than in those in whom a DLT was used.
Acknowledgments
None.
Author Contributions
Chia-Hung Yu helped design the study and prepare and draft the manuscript; Yi-Chen Chen helped design the study, collect and analyse the data, and revise the manuscript; Fu-Wen Liang helped design the study, analyse the data, and revise the manuscript; Jen-Yin Chen helped design the study and revise the manuscript; Chung-Han Ho helped to design the study, analyse the data, and revise the manuscript; Chin-Chen Chu helped to design the study and prepare and revise the manuscript.
Conflict of Interest
None.
Financial Disclosures
This work was supported internally by a grant (number CMFHR-10585) from the Chi Mei Medical Center, Tainan, Taiwan.
Implications Statement
In this study, patients undergoing thoracic surgery with a DLT experienced more postoperative pulmonary complications than those undergoing this surgery with a DLT. We should be alert to the increased risks of these complications in patients in whom a BB rather than a DLT is used.
References
| 1 |
Brodsky JB, Lemmens HJ.
The history of anesthesia for
thoracic surgery.
Minerva Anestesiol. 2007;73(10):513-524.
|
| 2 |
Gayes JM.
Pro: one-lung ventilation is best accomplished
with the Univent endotracheal tube.
J Cardiothorac
Vasc Anesth. 1993;7(1):103-107.
|
| 3 |
Slinger P.
Con: the Univent tube is not the best method
of providing one-lung ventilation.
J Cardiothorac
Vasc Anesth. 1993;7(1):108-112.
|
| 4 |
Cohen E.
Pro: the new bronchial blockers are preferable
to double-lumen tubes for lung isolation.
J Cardiothorac
Vasc Anesth. 2008;22(6):920-924.
|
| 5 |
Slinger P.
Con: the new bronchial blockers are not preferable
to double-lumen tubes for lung isolation.
J Cardiothorac
Vasc Anesth. 2008;22(6):925-929.
|
| 6 |
Neustein SM.
Pro: bronchial blockers should be used
routinely for providing one-lung ventilation.
J Cardiothorac
Vasc Anesth. 2015;29(1):234-236.
|
| 7 |
Brodsky JB.
Con: a bronchial blocker is not a substitute
for a double-lumen endobronchial tube.
J Cardiothorac
Vasc Anesth. 2015;29(1):237-239.
|
| 8 |
Brodsky JB.
Lung separation and the difficult airway.
J Anaesth. 2009;103(suppl 1):i66-i75.
|
| 9 |
Campos JH.
Lung isolation techniques for patients with difficult airway.
Curr Opin Anaesthesiol. 2010;23(1):12-17.
|
| 10 |
Collins SR, Titus BJ, Campos JH, Blank RS.
Lung isolation in the patient with a difficult airway.
Anesth Analg. 2018;126(6):1968-1978.
|
| 11 |
Granell Gil M, Solís Albamonte P, Córdova Hernández C, Cobo I, Guijarro R, de Andrés Ibañez JA.
Intubation in
two patients with difficult airway management and tracheal
stenosis after tracheostomy in thoracic surgery.
Rev Esp Anestesiol Reanim. 2018;65(6):347-350.
|
| 12 |
Granell M, Parra MJ, Jiménez MJ, et al.
Review of difficult
airway management in thoracic surgery.
Rev Esp
Anestesiol Reanim. 2018;65(1):31-40.
|
| 13 |
Lewis JW Jr, Serwin JP, Gabriel FS, Bastanfar M, Jacobsen G.
The utility of a double-lumen tube for one-lung ventilation in a variety of noncardiac thoracic surgical procedures.
J Cardiothorac Vasc Anesth. 1992;6(6):705-710.
|
| 14 |
Benumof JL, Wu D.
Tracheal tear caused by extubation of
a double-lumen tube.
Anesthesiology. 2002;97(4):1007-
1008.
|
| 15 |
Kim HK, Jun JH, Lee HS, Choi YR, Chung MH.
Left
mainstem bronchial rupture during one-lung ventilation
with Robertshaw double lumen endobronchial tube—a
case report.
Korean J Anesthesiol. 2010;59suppl(suppl): S21-S25.
|
| 16 |
Bessa Júnior RC, Jorge JC, Eisenberg AF, Duarte WL, Silva MS.
Bronchial rupture after intubation with double lumen endotracheal tube. Case report.
Rev Bras
Anestesiol. 2005;55(6):660-664.
|
| 17 |
Liu H, Jahr JS, Sullivan E, Waters PF.
Tracheobronchial
rupture after double-lumen endotracheal intubation.
J Cardiothorac
Vasc Anesth. 2004;18(2):228-233.
|
| 18 |
Yüceyar L, Kaynak K, Cantürk E, Aykaç B.
Bronchial
rupture with a left-sided polyvinylchloride double-lumen
tube.
Acta Anaesthesiol Scand. 2003;47(5):622-625.
|
| 19 |
Defosse J, Schieren M, Böhmer A, et al.
Dexmedetomidine as an adjuvant
to local anesthetics in transversus abdominis plane
block: a systematic review and meta-analysis.
A Germany-wide
survey on anaesthesia in thoracic surgery. Anaesthesist.
2016;65(6):449-457. [In German]
|
| 20 |
Della Rocca G, Langiano N, Baroselli A, Granzotti S, Pravisani C.
Survey of thoracic anesthetic practice in Italy.
J Cardiothorac Vasc Anesth. 2013;27(6):1321-1329.
|
| 21 |
Shelley B, Macfie A, Kinsella J.
Anesthesia for thoracic surgery:
a survey of UK practice.
J Cardiothorac Vasc Anesth.
2011;25(6):1014-1017.
|
| 22 |
Narayanaswamy M, McRae K, Slinger P, et al.
Choosing a
lung isolation device for thoracic surgery: a randomized
trial of three bronchial blockers versus double-lumen
tubes.
Anesth Analg. 2009;108(4):1097-1101.
|
| 23 |
Chang CC, Liao CC, Chen TL.
Perioperative medicine
and Taiwan National Health Insurance Research Database.
Acta Anaesthesiol Taiwan. 2016;54(3):93-96.
|
| 24 |
Cheng SH, Chiang TL.
The effect of universal health
insurance on health care utilization in Taiwan. Results
from a natural experiment.
JAMA. 1997;278(2):89-93.
|
| 25 |
Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML.
Validation
of the National Health Insurance Research Database with
ischemic stroke cases in Taiwan.
Pharmacoepidemiol
Drug Saf. 2011;20(3):236-242.
|
| 26 |
Cheng CL, Lee CH, Chen PS, Li YH, Lin SJ, Yang YH.
Validation of acute myocardial infarction cases in the national
health insurance research database in Taiwan.
J Epidemiol.
2014;24(6):500-507.
|
| 27 |
Hsieh CY, Chen CH, Li CY, Lai ML.
Validating the diagnosis
of acute ischemic stroke in a National Health
Insurance claims database.
J Formos Med Assoc.
2015;114(3):254-259.
|
| 28 |
Cheng CL, Chien HC, Lee CH, Lin SJ, Yang YH.
Validity
of in-hospital mortality data among patients with
acute myocardial infarction or stroke in National Health
Insurance Research Database in Taiwan.
Int J Cardiol.
2015;201:96-101.
|
| 29 |
Deyo RA, Cherkin DC, Ciol MA.
Adapting a clinical
comorbidity index for use with ICD-9-CM administrative
databases.
J Clin Epidemiol. 1992;45(6):613-619.
|
| 30 |
Frenkel WJ, Jongerius EJ, Mandjes-van Uitert MJ, van Munster BC, de Rooij SE.
Validation of the Charlson
Comorbidity Index in acutely hospitalized elderly
adults: a prospective cohort study.
J Am Geriatr Soc.
2014;62(2):342-346.
|
| 31 |
Whitmore RG, Stephen JH, Vernick C, et al.
ASA
grade and Charlson Comorbidity Index of spinal surgery
patients: correlation with complications and societal
costs.
Spine J. 2014;14(1):31-38.
|
| 32 |
Austin PC.
Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research.
Commun Stat Simul Comput.
2009; 38(6): 1228-1234.
|
| 33 |
Rubin DB.
Using propensity scores to help design observational studies: application to the tobacco litigation.
Health Serv Outcomes Res Methodol. 2001;2:169-188.
|
| 34 |
Bauer C, Winter C, Hentz JG, Ducrocq X, Steib A, Dupeyron JP.
Bronchial blocker compared to double-lumen tube for one-lung ventilation during thoracoscopy.
Acta Anaesthesiol
Scand. 2001;45(2):250-254.
|
| 35 |
Clayton-Smith A, Bennett K, Alston RP, et al.
A comparison
of the efficacy and adverse effects of double-lumen
endobronchial tubes and bronchial blockers in thoracic
surgery: a systematic review and meta-analysis of randomized
controlled trials.
J Cardiothorac Vasc Anesth.
2015;29(4):955-966.
|
| 36 |
Campos JH, Kernstine KH.
A comparison of a left-sided
Broncho-Cath with the torque control blocker
univent and the wire-guided blocker.
Anesth Analg.
2003;96(1):283-289.
|
| 37 |
Campos JH, Hallam EA, Ueda K.
Lung isolation in the
morbidly obese patient: a comparison of a left-sided
double-lumen tracheal tube with the Arndt® wire-guided
blocker.
Br J Anaesth. 2012;109(4):630-635.
|
| 38 |
Bussières JS, Somma J, del Castillo JL, et al.
Bronchial
blocker versus left double-lumen endotracheal tube in
video-assisted thoracoscopic surgery: a randomized-controlled
trial examining time and quality of lung deflation.
Can J Anaesth. 2016;63(7):818-827.
|
| 39 |
Lu Y, Dai W, Zong Z, et al.
Bronchial blocker versus left
double-lumen endotracheal tube for one-lung ventilation
in right video-assisted thoracoscopic surgery.
J Cardiothorac
Vasc Anesth. 2018;32(1):297-301.
|
| 40 |
Sandberg WS.
Endobronchial blocker dislodgement leading to pulseless electrical activity.
Anesth Analg. 2005;100(6):1728-
1730.
|
Supplement
Download full-size image
Download full-size image
Download full-size image
Download full-size image