Abstract
Pain management is one of the main focuses on coronavirus disease 2019 (COVID-19) patients treatment. Based on the review, we make some pain management recommendations f Indonesian COVID-19 patients based on the Indonesian Society of Anesthesiology for Pain Manageme meeting. We follow some recommendations by health organizations and make some recommendations for gener pain management and postoperative pain management for Indonesian COVID-19 patients including, the choice of analgesic, pain management post-operative, and personal protective equipment.
Keywords
analgesic, COVID-19, ISAPM, pain management, post-operative, PPE
Introduction
Pain management is one of the main focuses on coronavirus disease 2019 (COVID-19) patients treatment. The information regarding drug choices or pain management techniques for COVID-19 patients is still needed due to the minimal number of publications. Below is some review regarding pain management on COVID-19 patients and the recommendation of pain management in Indonesian COVID-19 patients based on the Indonesian Society of Anesthesiology for Pain Management (ISAPM) meeting.
Literacture Review
American Society of Regional Anesthesia and Pain Medicine (ASRA) and European Society of Regional Anesthesia and Pain Therapy (ESRA) recommendation:1
General recommendation:
(1) All elective schedules, direct patient visits must be canceled. If possible, telemedicine facilities can be used.
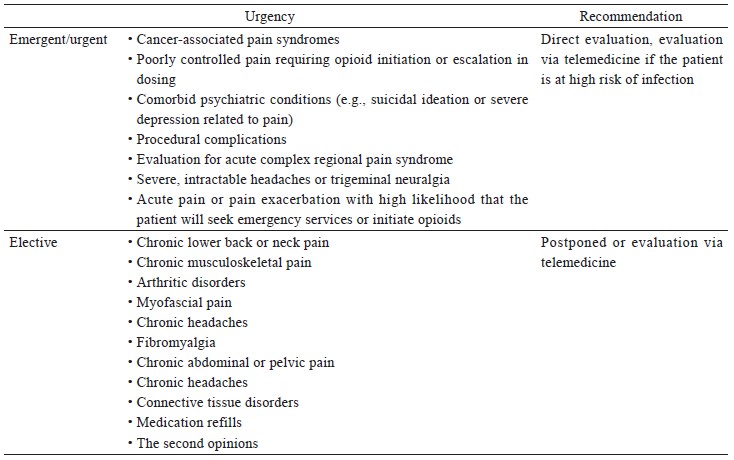
(2) Elective pain management procedures must be postponed, except for semi-urgent procedures. Pain management actions are classifi ed into elective, urgent, and emergent categories (Table 1).2
Download full-size image
(3) Although most chronic pain interventions are elective, there are several conditions in which actions can be categorized as urgent or emergent.
(4) Regional anesthesia is preferred over general anesthesia to reduce the risk of transmission.
(5) Use block that reduce respiratory interference (e.g., peripheral nerve block [axillary or infraclavicular brachial plexus block]).
(6) Risk-benefit should be considered for perineural adjuvants and continuous perineural catheters.
The Choice of Analgesic for COVID-19 Patients
The use of analgesics in COVID-19 patients is still under discussion. During this time, analgesics used include non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, steroid, or opioids. The following is some information related to the use of analgesic drugs based on medical associations.
Opioid
- The use of opioids in patients with high body temperature (fever) associated with COVID-19 infection might increase the absorption of transdermal opioid patches and might increase opioid side effects (The British Pain Society [BPS], March 26, 2020)3
- Opioids are also cough suppressants and may be able to mask or inhibit the appearance of early symptoms of COVID-19 infection (BPS, March 26, 2020)3
- Opioids and neuropathic pain medications can worsen COVID-19-related symptoms such as tiredness, nausea, and gastrointestinal symptoms. (BPS, March 26, 2020).3
- ESRA and ASRA do not recommend any changes to the ongoing opioid treatment regimen when there is no change in pain scale or changes in function.1
- ASRA and ESRA recommend monitoring transdermal opioids for patients with fever because the rate of absorption cannot be predicted (ASRA and ESRA, March 27, 2020).1
NSAIDs
- In a paper published in British Medical Journal on March 17, 2020, it was mentioned that the use of ibuprofen and NSAIDs for pain and fever management in COVID-19 patients could increase complications in respiratory infections or prevent healing of COVID-19 patients.4 So far, there has been no evidence to confirm ibuprofen to worsen the condition of COVID-19 patients. However, the role of ibuprofen as an anti-inflammatory and antipyretic drug may mask the symptoms and signs of COVID-19 infection (BPS, March 26, 2020).3
- The Medicine and Healthcare Regulatory Agency (MHRA) and the National Institute for Health and Care Excellence (NICE) then review and find if patients who are confirmed to be COVID-19, are advised to get paracetamol (acetaminophen) compared to NSAID ibuprofen. (BPS, March 26, 2020).3
- The European Medicines Agency (EMA) recommends the use of paracetamol and NSAIDs for the treatment of pain and fever in COVID-19 patients, with paracetamol (acetaminophen) as the first choice for pain and fever management (EMA, March 18, 2020).5
- The EU National Treatment Guidelines state that NSAIDs (e.g., ibuprofen) still can be used for COVID-19 patients, with the recommendation of using the lowest effective dose or according to conditions (EMA, March 18, 2020).5
- ASRA and ESRA recommend patients who have received NSAIDs to continue using NSAIDs, by educating patients to report new fever or myalgia after receiving NSAIDs (ASRA and ESRA, March 27, 2020).1
- There is not enough evidence that NSAIDs are not recommended for COVID-19 patients (Public Health Ontario, April 3, 2020).6
- The Center for Evidence-Based Medicine recommends that the use of NSAIDs in patients with an acute respiratory infection should be done carefully, including by considering risk factors, side effects such as contraindications, interactions between drugs, patient’s medical history, and other monitoring needs (NICE, April 14, 2020).7
Steroid
- Patients receiving steroids have the potential for secondary adrenal insufficiency and decreased immune system (ASRA and ESRA, March 27, 2020).1
- Corticosteroid injection in joints shows a link with a higher risk of influenza (ASRA and ESRA, March 27, 2020).1
- Evaluation of the benefits/risks of steroid injection and dose use should be carried out especially for patients with high risk (ASRA and ESRA, March 27, 2020).1
- The effect of corticosteroid injection in COVID-19 patients is unknown, but the nature of corticosteroids that can decrease the immune system allows corticosteroids to reduce survival benefits and have possible dangers such as avascular necrosis, psychosis, diabetes, and inhibition of virus clearance (BPS, March 26, 2020).3
- The duration of immune system suppression can be reduced using dexamethasone and betamethasone (ASRA and ESRA, March 27, 2020).1
Acetaminophen (paracetamol)
- The use of acetaminophen and NSAIDs as pain or fever management in COVID-19 patients can be tolerated when used for short-term pain or fever management (Public Health Ontario, April 3, 2020).6
- Acetaminophen (Tylenol®) is recommended to remain the first choice for COVID-19 patients, with the least possible side effects (Public Health Ontario, April 3, 2020).6
- When acetaminophen is not possible, the NSAIDs can be used with consideration of comorbidities and risk factors of each patient (Public Health Ontario, April 3, 2020).6
- MHRA and NICE then conducted a review and found if patients who were confirmed to be COVID-19 positive, were advised to get paracetamol (acetaminophen) than ibuprofen (BPS, March 26, 2020).3
- Acetaminophen is preferred over NSAIDs.2
- Pan American Health Organization recommends the use of paracetamol to be prioritized over ibuprofen.8
Relationship Between Analgesics and Immune Responses
COVID-19 patients experience significant immune system changes. COVID-19 patients have normal or decreased leukocyte levels and lymphocytopenia. Besides, thrombocytopenia also appears in some severe cases.1 Therefore, further knowledge of the interactions of analgesic drugs used for COVID-19 patients with the immune system is needed to prevent the emergence of high risks.
Opioids
Opioids are one of the strong analgesics for pain treatment. However, opioids have several side effects such as respiratory depression, addiction, nausea, anxiety disorders, and potential hyperalgesia due to opioids. Another side effect that needs attention is the potential to suppress or inhibit the immune system. However, the results of the study are not consistent. Some studies show different results.9 Research using exogenous opioids (morphine and fentanyl) shows if there is an inhibition of the function of macrophages, natural killer cells, and T-cells. In-vivo studies and in experimental animals have shown a weakening of the intestinal mucosal immunity (gut barrier). In epidemiological studies, high-dose opioids and opioid therapy for non-malignant pain correlate with the risk of infectious diseases such as pneumonia. However, in endogenous opioids (opioids-peptides) which are secreted by neutrophils, macrophages, and T-cells can bind to opioid receptors to eliminate inflammation and neuropathic pain. Further research is still needed to determine the role of opioids in the immune system.10
NSAIDs
NSAIDs are anti-inflammatory drugs that target inflammatory cells such as macrophages and neutrophils. NSAIDs also inhibit T-cell proliferation, inhibit the expression of cell markers such as cluster of differentiation (CD)25 and CD71, and inhibit the production of cytokines (IL-2, IFN-γ, and TNF-α). NSAIDs also have immunosuppressive activity by blocking some of the transcription factors needed in gene expression that are triggered by the activation of T-cell antigen receptors (TCR) by antigens. NSAIDs will also affect one or more stages in the TCR-signaling cascade that aims to activate transcription factors. Cyclooxygenases (COX) activity is one of the main pathways that is inhibited by NSAIDs. COX is a catalyst for prostaglandin (PG) biosynthesis.11 PGs play a role in maintaining homeostasis, mediating pathogenic mechanisms, and also contributing to inflammatory pain.12 NSAIDs are used as analgesics by inhibiting the formation of PGE 2.13
Steroid
Steroids or corticosteroids are one of the anti-inflammatory drugs. Steroid drugs inhibit vasodilation and increase vascular permeability that accompanies inflammation. Steroids also reduce the emigration of leukocytes into the area of infection. One type of steroids, glucocorticoid, can inhibit the crucial activity of the transcriptional regulator of the pro-inflammatory gene, NF-kB and AP-1. NF-kB and AP-1 play an important role in the expression of genes involved in inflammation. Glucocorticoids inhibit the transcription of several genes that encode pro-inflammatory cytokines and chemokines, cell adhesion molecules, and several enzymes that play a role in the initiation and response of the immune system to antigens.14 Glucocorticoids also induce glucocorticoid-induced genes. These genes include IL-10 encoding genes. IL-10 is an anti-infectious immunomodulator and cytokine. Besides, glucocorticoids induce glucocorticoid-induced leucine zipper (GILZ), a protein that interacts and can inhibit the function of NF-kB and AP-1.14
Acetaminophen
Acetaminophen potentially becomes a hepatotoxic agent. The use of a high dose or overdose can cause liver injury. Acetaminophen that enters the body will be broken down into fractions that will be metabolized. Small fractions (10–15%) will be metabolized in the liver by the cytochrome P450 isoform to become N-acetyl-p-benzoquinone imine (NAPQI). Antioxidant glutathione (GSH) will transform NAPQI into a harmless form. The overdosed acetaminophen makes GSH cannot fully convert all NAPQI into inactive/harmless forms. NAPQI then binds to mitochondrial proteins and causes hepatocyte necrosis.15
Liver injury is not only caused by acetaminophen dose but also occurs due to an inflammatory response due to acetaminophen-induced liver injury. Damaged hepatocytes synthesize danger-associated-molecular patterns, which will be recognized by immune cells in the liver such as macrophages, Kupffer cells (KCs), and neutrophils. These cells will be activated and synthesize various pro-inflammatory cytokines such as TNF-α or IL-1β which will increase the inflammatory process in the liver. Activation of the immune system will increase the rate of inflammation that can trigger hepatocyte necrosis.15,16
Cheadle in 202017 identified the effects of several NSAIDs on proteins regulated by Acute Respiratory Distress Syndrome (ARDS) using protein interaction modeling. Drugs used include aspirin, ibuprofen (Advil®, Motrin®), acetaminophen (Paracetamol®, Tylenol®), and naproxen (Aleve®, Naproxen®). Based on the analysis it is known if:
- There are 22 potential proteins whose activation is upregulated by ARDS.
- Aspirin regulates 17 of the 22 target proteins. Aspirin is identified as a net-inhibitor of 15 proteins and activates 2 proteins.
- Ibuprofen (NSAID) regulates 9 of 22 target proteins, where ibuprofen acts as an inhibitor by inhibiting 7 of 9 proteins and activating 2 target proteins.
- Naproxen® interacts with 9 of the 22 target proteins. However, Naproxen® does not have a specific function because there are two balanced mechanisms between inhibitors and activators.
- Acetaminophen interacts with 13 of the 22 target proteins. Acetaminophen is identified as an activator by activating 11 of 13 target proteins and inhibiting 2 of 13 target proteins.
- Paracetamol® and Tylenol® may not be helpful in patients with severe cases of ARDS caused by pathogens such as coronavirus.
- These are related to the fact that high dose of acetaminophen can cause acute liver injury. Besides, most of the hepatotoxic pro-inflammatory proteins also increase in ARDS.
- Giving high doses of acetaminophen (e.g., Tylenol®) in patients at risk of respiratory failure must be considered because it increases the possibility of a synergistic negative reaction.
Other Pain Management Alternative Therapy
ASRA and ESRA recommendation:1
- The use of regional anesthesia, both neuraxial block and peripheral nerve block (e.g., by continuous epidural catheters) reduces the risk of aerosol in patients.
- Axillary block and infraclavicular brachial plexus block also reduce respiratory interface.
- In patients who are intraoperatively facilitated with peripheral nerve block, it is recommended to use a peripheral nerve catheter so that it can be used as continuous postoperative pain therapy.
Personal Protective Equipment in COVID-19 Pain Management
Personal protective equipment used in pain management of positive or suspected COVID-19 patients includes goggles, face masks, face shields, gloves, and gown.
Goggles
The characteristics of goggles used including fully enclose the eye area and its surroundings (fit and good seal with the skin), accommodates the use of glasses, clear plastic lenses, scratch, and fog-resistant, the strap can be adjusted according to the size of the head, and maybe re-usable.18
Face Mask
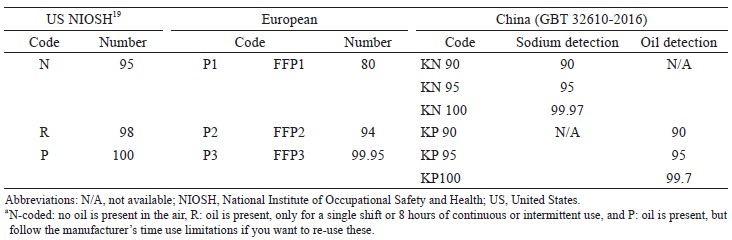
Face masks can be classified based on their resistance to oil and how many air particles they filter. Based on the US National Institute of Occupational Safety and Health, the resistance of masks to oil was divided into three groups (NRP). The number shows the percentage of air that is filtered. The number 95 indicates that 95% of the air particles will be filtered. There are several versions of the coding of marker types, including according to European or Chinese standards (Table 2).19 The N95 or FFP2 face mask is recommended for pain management in COVID-19 patients.18,20
Download full-size image
Face Shield
The face shield that is used must have characteristics including high visibility, made of plastic, fit the user’s forehead, resistant to moisture, and cover the entire face area. The face shield can be disposable or reusable (reusable: has been disinfected before use).18
Gloves
Gloves can prevent the transmission of the virus when in contact with patients. The gloves that recommend are nitryl gloves, powder-free, and single-use. We also recommended the use of double gloves. Due to the potential to cause irritation or allergies, latex gloves with powder are not recommended.18,20
Gown
Healthcare workers should wear gowns recommended by the Food and Drug Administration. Gown selection is based on the level of risk of the disease. For COVID-19 patients, which is a high risk, a coverall gown is recommended. The coverall dress used has characteristics including polyethylene coated, lightweight material, and high resistance (tear or abrasion resistance), zippers allow perfect closure, and disposable.21
Conclusion
Base on the review, below is the recommendation for Indonesian COVID-19 patients based on the ISAPM meeting:
- Classifying pain management into elective, urgent, and emergent categories.
- The use of acetaminophen (Paracetamol®), is recommended to be the first/basic option for pain and fever management in COVID-19 patients.
- The use of NSAID drugs such as ibuprofen can be given as a single administration or combine with paracetamol.
- The use of NSAIDs must consider each patient’s comorbid and risk factors.
- There is no strong evidence that shows NSAIDs can worsen the condition of COVID-19 patients.
- Opioids can still be given as a modality of pain, especially in acute pain and cancer pain. Monitoring and utilization of telemedicine can be applied for side effects and drug abuse evaluation.
- Opioids for postoperative acute pain can be given using patient-controlled analgesia (PCA) techniques.
- Protein interactions modeling by Chris Cheadle shows that acetaminophen (high doses) may not help patients with ARDS. The use of Acetaminophen (high doses) must be done with consideration of comorbidities and risk factors of each patient.
- Analgesic drugs commonly used have a close relationship with the immune system. Therefore, evaluation of the patient’s immune condition is needed to choose the right analgesic drug for COVID-19 patients.
For post-operative pain management, it is necessary to consider the following:
- Using multimodal analgesia
- There are a lot of controversies regarding NSAIDs, especially ibuprofen, but there has not enough evidence.
- Paracetamol can be given as basic analgesia in all postoperative cases combined with opioids or local anesthesia.
- Opioid bases can be given with PCA techniques which good at controlling the patient’s analgesic needs, and reducing the direct contact of health workers when given intermittently and intravenously.
- The use of regional anesthesia, both neuraxial block and peripheral nerve block (for example by continuous epidural catheters) reduces the risk of aerosol in patients.
- In patients who are intraoperatively facilitated with peripheral nerve block, it is recommended to use a peripheral nerve catheter so that it can be used as continuous postoperative pain therapy.
Personal protective equipment for pain management:
- Personal protective equipment used in pain management of positive or suspected COVID-19 patients includes goggles, face masks, face shields, gloves, and gown.
- Goggles: fully enclose the eye area and its surroundings (fit and good seal with the skin), accommodates the use of glasses, clear plastic lenses, scratch and fog-resistant, the strap can be adjusted according to the size of the head, and maybe re-usable.
- Face mask: the N95 or FFP2 face mask is recommended for pain management in COVID-19 patients.
- Gloves: nitryl gloves, powder-free, and single-use. We also recommended the use of double gloves.
- Gown: polyethylene coated, lightweight material, and high resistance (tear or abrasion resistance), zippers allow perfect closure, and disposable.
Conflict of Interest
The authors declare there is no conflict of interest.
References
| 1 |
American Society of Regional Anesthesia and Pain Medicine
(ASRA), European Society of Regional Anesthesia
and Pain Therapy (ESRA).
COVID-19 Guidance for
Regional Anesthesia Neuraxial Anesthesia and Peripheral
Nerve Blocks.
Updated March 31, 2020. Accessed May 7, 2020.
|
| 2 |
Cohen SP, Baber ZB, Buvanendran A, et al.
Pain management
best practices from multispecialty organizations
during the COVID-19 pandemic and public health crises.
Pain Med. 2020;21(7):1331-1346.
|
| 3 |
The British Pain Society.
Pain Management during
COVID-19 viral infection.
Updated March 26, 2020.
Accessed May 7, 2020.
|
| 4 |
Day M.
COVID-19: ibuprofen should not be used for managing symptoms, say doctors and scientists.
BMJ.
2020;368:m1086.
|
| 5 |
European Medicines Agency.
EMA gives advice on the
use of non-steroidal anti-inflammatories for COVID-19.
Published March 18, 2020. Accessed May 7, 2020.
|
| 6 |
Public Health Ontario.
COVID-19 What We Know So Far
About… Use of Non-Steroidal Anti-Inflammatory Drugs
(NSAIDs).
Published April 3, 2020. Accessed May 6, 2020.
|
| 7 |
National Institute for Health and Care Excellence.
COVID-19 rapid evidence summary: acute use of non-steroidal anti-inflammatory drugs (nsaids) for people with or at risk of COVID-19.
Published April 14, 2020.
Accessed May 6, 2020.
|
| 8 |
Pan American Health Organization.
Ibuprofen and
COVID-19.
Published March 18, 2020. Accessed May 6, 2020.
|
| 9 |
Plein LM, Rittner HL.
Opioids and the immune system—
friend or foe.
Br J Pharmacol. 2018;175(14):2717-2725.
|
| 10 |
Roy S, Ninkovic J, Banerjee S, et al.
Opioid drug abuse
and modulation of immune function: consequences in the
susceptibility to opportunistic infections.
J Neuroimmune
Pharmacol. 2011;6(4):422-465.
|
| 11 |
Paccani SR, Boncristiano M, Ulivieri C, D’Elios MM,
Del Prete G, Baldari CT.
Nonsteroidal anti-inflammatory
drugs suppress T-cell activation by inhibiting p38
MAPK induction.
J Biol Chem. 2002;277(2):1509-1513.
|
| 12 |
Ricciotti E, Fitzgerald GA.
Prostaglandins and inflammation.
Arterioscler Thromb Vasc Biol. 2011;31(5):986-1000.
|
| 13 | |
| 14 |
Coutinho AE, Chapman KE.
The anti-inflammatory and
immunosuppressive effects of glucocorticoids, recent
developments and mechanistic insights.
Mol Cell Endocrinol.
2011;335(1):2-13.
|
| 15 |
Krenkel O, Mossanen JC, Tacke F.
Immune mechanisms
in acetaminophen-induced acute liver failure.
Hepatobiliary
Surg Nutr. 2014;3(6):331-343.
|
| 16 |
Fischer JE, Mckenzie TJ, Lillegard JB, et al.
Role of
Kupffer cells and toll-like receptor 4 in acetaminopheninduced
acute liver failure.
J Surg Res. 2013;180(1):147-
155.
|
| 17 |
Cheadle C.
Analgesics Use And The Coronavirus: Finding Answers Through Biological Knowledge Graph.
Elsevier.
Updated March 31, 2020. Accessed May 6, 2020.
|
| 18 |
Pan American Health Organization, World Health Organization
Regiaonal Office for the Americas
Requirements
and technical specifications of personal protective
equipment (PPE) for the novel coronavirus (2019-
ncov) in healthcare settings.
Published February 6, 2020.
Accessed May 6, 2020.
|
| 19 |
Virginia Tech (Environmental Health and Safety).
Information
for N, R, and P Particulate Respirator Categories.
Updated February 3, 2014. Accessed May 6, 2020.
|
| 20 |
Arif SK, Muchtar F.
Manajemen periopepatif: pasien
COVID-19.
PP. Perdatin. Published April 28, 2020. Accessed May 6, 2020. [in Indonesian]
|
| 21 |
Personal Protective Equipment for Infection Control.
U.S. Food & Drug Administration.
Updated February
10, 2020. Accessed May 6, 2020.
|