Abstract
Background: Preoperative airway assessment and anticipation of a difficult airway is of utmost critical value in anaesthesiology as failure to secure airway can lead to morbidity and mortality. The study evaluated ratio of height-to-thyromental distance (RHTMD) and ratio of height-to-sternomental distance (RHSMD) as predictors of a difficult airway.
Methods: The prospective observational study evaluated 131 adult participants scheduled for elective surgery under general anaesthesia. In addition to the preoperative airway assessment, RHTMD and RHSMD were calculated. Correlation of these ratios with the Cormack–Lehane grading of glottis visualisation on direct laryngoscopic view following induction of anaesthesia was analyzed. The optimal cut-off point for RHTMD and RHSMD were identified using receiver operating characteristic curve analysis.
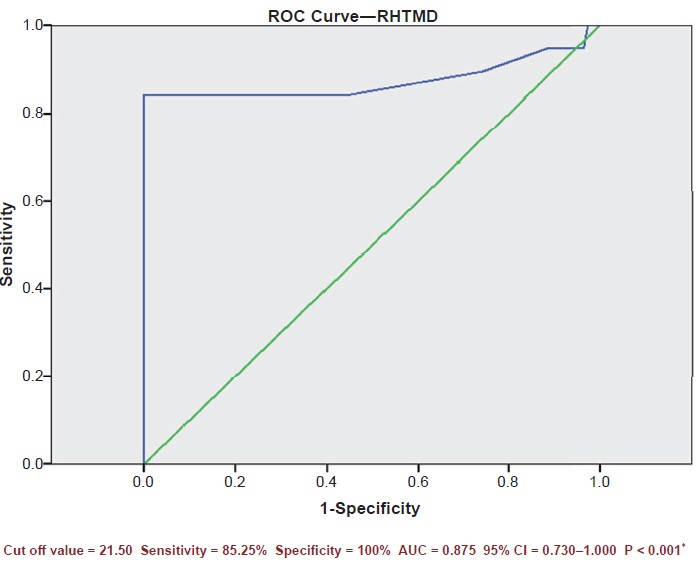
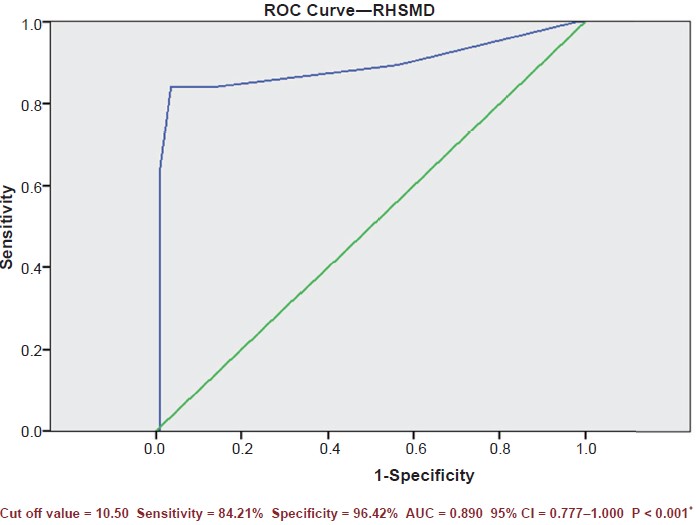
Results: The incidence of difficult intubation was 14.50%. The cut-off values for RHTMD and RHSMD were < 21.50 (sensitivity 85.25%, specificity 100.00%) and < 10.50 (sensitivity 84.21%, specificity 96.42%) respectively for predicting difficult airway. The area under the curve with 95% confidence interval for RHTMD was 0.875 (0.730–1.000) and that for RHSMD was 0.890 (0.777–1.000).
Conclusion: RHTMD was found to be a better predictor of difficult intubation and restricted laryngoscopic view compared to RHSMD.
Keywords
airway assessment, Cormack–Lehane’s grading, difficult intubation, sternomental distance, thyromental distance
Introduction
Anticipating and managing difficult intubation is a vital skill to the practice of anaesthesiology. Difficult/failed intubation is one of the major causes of anaesthesia related morbidity and mortality.1 Closed claims analysis study for management of difficult airway found that the vast majority (85%) of airway related events involve brain damage, and one-third of mortality was attributable solely to anaesthesia, which was due to inability to maintain a patent airway and oxygenation.2 Task Force on Management of the Difficult Airway by the American Society of Anaesthesiologists (ASA) recommends that a patient must be assessed preoperatively for airway difficulties.3 Difficult laryngoscopy and intubation is described in 1.5 to 16.0% of patients.4 Hence preoperative evaluation of the airway is one of the fundamental steps in anaesthesia.
Difficult airway may manifest as difficulty in ventilation, difficult laryngoscopy, or difficult intubation. Manipulation of the airway by multiple attempts during direct laryngoscopy often leads to airway trauma, bleeding, and oedema which ultimately interfere with vocal cord visualization.5
Many preoperative airway assessment tests like inter-incisor gap, mouth opening, Mallampati grading, head and neck movement, upper lip bite test, sternomental distance (SMD), and thyromental distance (TMD) are used to predict difficult intubation, but sensitivity and positive predictive values (PPVs) of these individual tests are low while false positive results are high.6
Ratio of height-to-thyromental distance (RHTMD) introduced by Schmitt et al.7 and ratio of height-to-sternomental distance (RHSMD) are considered as useful screening tests for predicting difficult laryngoscopy; however, very few studies exist comparing these two predictive tests.8
The present study was carried out to evaluate the ability of RHTMD and RHSMD to predict difficult laryngoscopy.
Methods
This prospective analytical cross-sectional study was carried out in 131 patients in a tertiary care teaching hospital. Approval from the Institutional Ethics Committee was obtained before conducting the study. Written informed consent was obtained from the patients for participation in the study. Patients of either gender, from 18 to 60 years of age, belonging to ASA physical status 1 and 2 scheduled for elective surgery under general anaesthesia and tracheal intubation were included in the study. Patients with restricted neck mobility, major airway abnormalities, tumours or mass in the neck or airway, post burn neck contractures, pregnancy, kyphoscoliosis, obesity (BMI [body mass index] > 30), and those requiring rapid sequence intubation were excluded from the study. Sample size was calculated with the anticipated sensitivity and specificity of RHTMD 93% and 62% respectively4 and 95% confidence level. Consecutive patients fulfilling the inclusion and exclusion criteria were enrolled for the study. Anaesthesiologists with > 5 years of experience were involved in the preoperative airway assessment and grading of glottis exposure on direct laryngoscopy. All the enrolled patients underwent a thorough preoperative evaluation including a detailed history and clinical examination and advised standard preoperative fasting guidelines. Laboratory investigations, chest X-ray, electrocardiography (ECG), and echocardiography were assessed relevant to the patient and surgical requirements. Airway assessment was done by a single anaesthesiologist in all the cases who would not participate in the endotracheal intubation. Parameters included modified Mallampati classification (MMC), inter incisor gap, TMD, SMD, weight (kg), height (cm), BMI, and neck mobility. The Mallampati grading was done in the sitting position, with mouth open and tongue protruded without phonation. Patients were graded as class 1 if soft palate, faucial pillars, and uvula were visible; class 2 if soft palate or/and uvula were visible; class 3 if only soft palate and the base of uvula were visible; and class 4 if soft palate is not visible and only hard palate is visible.
TMD (in cm) was measured from bony point of mentum to thyroid notch with head in extension and mouth closed. SMD (in cm) was measured from bony point of mentum to manubrium sterni with head in extension and mouth closed. RHTMD was calculated from the ratio of height and TMD. RHSMD was calculated from the ratio of height and SMD. Mallampati class 3 and 4, TMD < 6.0 cm, SMD < 13.5 cm, RHTMD > 23.5,7 and RHSMD > 12.58 were considered as predictors of difficult intubation. On arrival at the operation theatre, baseline vital parameters were recorded. Standard general anaesthesia procedure was performed as per the institutional practice. Difficult airway carts with bougie, stillette, videolaryngoscopes, laryngeal mask airway, and fiberoptic bronchoscope of appropriate sizes were made available in the operating room. Intraoperative monitoring included pulse oximetry, non-invasive blood pressure, capnography, and ECG.
All patients were given intravenous premedication with ondansetron 0.10 mg/kg, midazolam 0.02 mg/kg, glycopyrrolate 0.02 mg/kg, and fentanyl 2.00 μg/kg. Following preoxygenation with 100% oxygen for 3 minutes induction was achieved with inj. propofol 1.0–2.0 mg/kg and muscle relaxation was achieved by vecuronium 0.1 mg/kg. An anesthesiologist with > 5 years of experience did a direct laryngoscopy with an appropriate sized macintosh blade and graded the glottis exposure. The best view obtained at the first attempt by the laryngoscopy without using any external manoeuvre was considered for the Cormack–Lehane classification.9 Grade 1—visualization of the entire laryngeal aperture, grade 2—visualization of parts of the laryngeal aperture or the arytenoids, grade 3—visualization of only the epiglottis, and grade 4—visualization of only the soft palate.
Intubation was considered difficult if the view on laryngoscopy was Cormack–Lehane grade 3 or 4, more than 3 attempts at tracheal intubation, duration taken for intubation longer than 10 minutes, failure to intubate or if special manoeuvres or additional aids such as stylets/bougie/video laryngoscopy/fiberoptic bronchoscope were required to facilitate intubation. If difficulty was experienced in tracheal intubation external laryngeal manipulation and backward, upward and rightward pressure on thyroid cartilage was applied as it improved visualization of glottis on direct laryngoscopy.
After endotracheal intubation with appropriate size endotracheal tube anaesthesia was maintained with O2, N2O, isoflurane and vecuronium with controlled ventilation and further anaesthetic management continued.
The preoperative airway assessment data and the findings during intubation were assessed to establish the incidence of difficult intubation, and the ability of RHTMD and RHSMD to predict difficult airway was noted in each patient. Data were analyzed using SPSS software v.23 (IBM Statistics, Chicago, USA) and Microsoft office 2007 and were represented using mean ± standard deviation, sensitivity, specificity, percentages, diagrams, chi-square test, and receiver operating characteristic curve (ROC) curve analysis. P < 0.05 was considered statistically significant.
Results
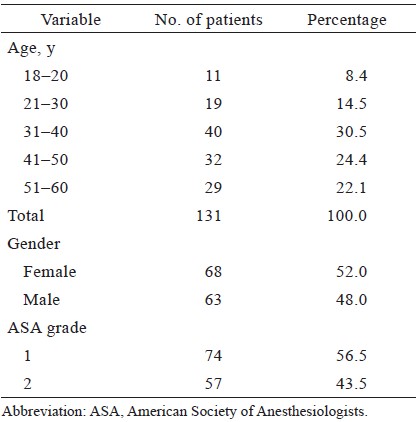
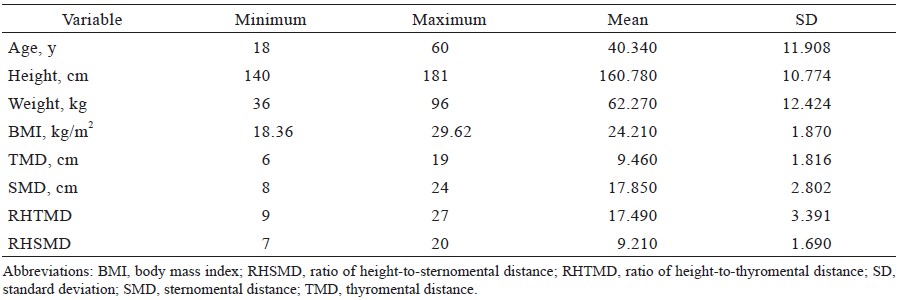
All the enrolled 131 patients completed the study. The mean age of the patients was 40.340 ± 11.908 years. The mean height of patients was 160.780 ± 10.774 cm. The mean weight of patients was 62.270 ± 12.424 kg. The mean BMI (kg/m2) was 24.210 ± 1.870 (Tables 1 and 2).
Download full-size image
Download full-size image
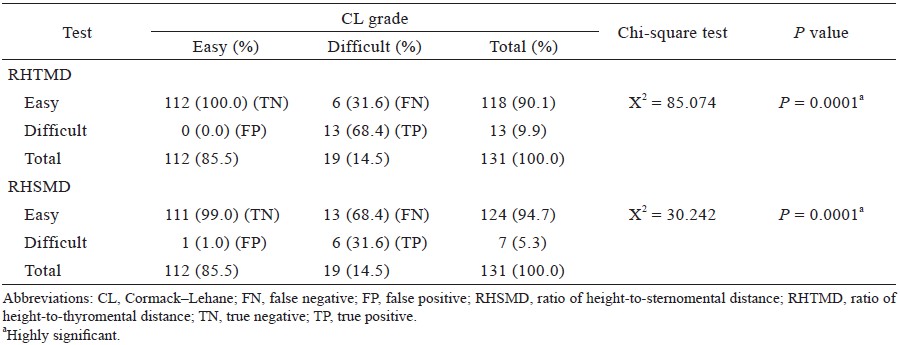
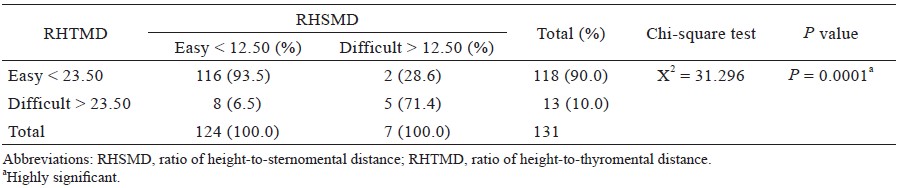
Difficult intubation was seen in 19 patients (incidence 14.5%) based on Cormack–Lehane grading (grade 3 and 4 was seen in 12 and 7 patients respectively) (Table 3). There was no failed intubation in our study. Of the 19 cases of difficult intubation, 16 were intubated in the first attempt with external laryngeal manipulation, and the remaining 3 patients were intubated using gum elastic bougie. On analysing RHTMD and RHSMD using chi-square test RHTMD is found to have more predictive value than RHSMD (Table 4). ROC curves were constructed for RHTMD (Figure 1) and RHSMD (Figure 2). The optimum cut-off value derived from the ROC curve for RHTMD and RHSMD was 21.50 and 10.50 respectively. RHTMD was found to be more sensitive and specific compared to RHSMD, both RHTMD and RHSMD were comparable on ROC curve analysis without much difference in area under the curve (AUC). Using RHTMD in combination with RHSMD increases the chance of predicting difficult intubation, rather than using them alone, and both the predictive tests were found to be highly statistically significant.
Download full-size image
Download full-size image
Download full-size image
Abbreviations: AUC, area under the curve; CI, confi dence interval.
Download full-size image
Abbreviations: AUC, area under the curve; CI, confi dence interval.
Discussion
Various clinical trials have outlined the importance of preoperative airway assessment plans to aid the anaesthesiologists in managing difficult airway. Several methods using both single and multiple tests have been employed to predict difficult airway.9 A screening test employed for prediction of difficult intubation should have high specificity and sensitivity, resulting in minimal false positive and false negative values. The consequences of false negative results are deleterious and life threatening.
A test to predict difficult intubation should have high sensitivity so that it will identify most patients in whom intubation will be truly difficult. The incidence of difficult intubation in various studies range from 1–18%, and that of failed intubation is between 0.05–0.35%.10 The incidence of difficult intubation and failed intubation in the present study was 14.5% and 0.0% respectively. This wide variation in the incidence of difficult laryngoscopy and intubation can be attributed to factors such as ethnic differences among populations, experience of the attending anaesthesiologist, sniffing position, and use of external laryngeal manipulation. External laryngeal manipulation increases thyromental height and improves laryngoscopic view.11
The cut-off value for TMD ranges from 5.5–7.0 in different studies. According to previous studies, TMD ≤ 6 cm improved the prediction of difficult intubation.12 In the present study among 19 patients who were found to have difficult intubation 14 patients had a TMD ≤ 6 cm. Ramadhani et al.13 evaluated SMD as a sole predictor of difficult laryngoscopy in the obstetric population. SMD and laryngoscopic view were documented in parturient patients undergoing Caesarean section under general anaesthesia, and the incidence of difficult laryngoscopy in the study was 3.5%. The study concluded that SMD of < 13.5 cm can predict difficult laryngoscopy. In the present study of the 19 patients who were found to have difficult intubation, 16 patients had SMD of ≤ 12.5 cm.
The primary aim of our study was to evaluate the efficacy of 2 predictive tests RHTMD and RHSMD. Schmitt et al. introduced RHTMD as a better predictor of difficult laryngoscopy than TMD.7 RHTMD takes into consideration the body proportions of the patient, and hence it is a better predictor than TMD.
Kaniyil et al.12 conducted a prospective observational study on adult patients to evaluate RHTMD as a predictor of difficult laryngoscopy. Airway indices like RHTMD, TMD, MMC, and the upper lip bite test were assessed and correlated with Cormack–Lehane laryngoscopic grading. The incidence of difficult laryngoscopy in the study was 5.33%. Among the 4 indices, RHTMD was found to be the single best test with sensitivity of 62.5% and specificity of 96.1% with a good PPV. A combination of all the indices resulted in 100% sensitivity and high specificity; the optimal cut-off value derived from the ROC curve for RHTMD was found to be 22.10. The optimal cutoff value derived from the ROC curve for RHTMD for our study population is 21.50 which is comparable with earlier studies, with AUC 0.875 which is a measure of discriminative power and accuracy. The cut-off value established by other studies in the past for RHTMD ranges from 23.5 to 25.0, which may be attributed to variations in the anthropometric measurements among the population. According to Safavi et al.14, the cut-off value for RHTMD for prediction of difficult laryngoscopy is race dependent, and the cut-off value for each population has to be calculated separately. Farzi et al.8 conducted a study on adult patients to compare airway tests RHTMD, RHSMD, and assessment of oropharyngeal view by MMC. The study demonstrated that RHSMD had the least false negative value, cut off point of RHSMD > 12.5 was not different between men and women, and RHSMD ≥ 12.5 had direct relationship with difficult laryngoscopy. In our study, RHSMD had good specificity and accuracy with a cut-off of 10.50. Ray et al.4 conducted an observational study in 138 children aged between 1 and 12 years scheduled for elective surgery under gene anaesthesia. They compared RHTMD with RHSMD as predictors of difficult laryngoscopy; 2b restricted view (Cormack–Lehane view as per Cooks modification) was used for predicting difficult laryngoscopy as there were no 3a, 3b, or grade 4 view in the entire study population; the incidence of difficult laryngoscopy was found to be 10.1%. ROC curve analysis was done for predicting difficult laryngoscopy. RHTMD was found to be a better predictor of restricted laryngoscopic view with AUC of 0.792 compared to RHSMD (AUC = 0.463). The study concluded that in children aged 1 to 12 years, RHTMD is a better predictor of restricted laryngoscopic view compared to RHSMD.
In this study, we have compared RHTMD and RHSMD as predictors of difficult laryngoscopy. Grade 3 and 4 Cormack–Lehane view is considered as difficult laryngoscopic view. The incidence of difficult intubation in our study is 14.5%; RHTMD was found to have high sensitivity (85.25%) and specificity (100.00%) compared to RHSMD with sensitivity and specificity of 84.21% and 96.42% respectively, and the AUC of RHTMD is 0.875 compared to RHSMD with AUC = 0.890.
Conclusion
On analysing RHTMD and RHSMD, RHTMD is found to be a better predictor of difficult intubation and restricted laryngoscopic view than RHSMD. Using RHTMD in combination with RHSMD increases the chance of predicting difficult intubation, rather than using them alone.
Conflict of Interest
There are no conflicts of interest.
Financial Support and Sponsorship
None.
References
| 1 |
Shiga T, Wajima Z, Inoue T, Sakamoto A.
Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance.
Anesthesiology
2005;103(2):429-437.
|
| 2 |
Caplan RA, Posner KL, Ward RJ, Cheney FW
Adverse respiratory events in anesthesia: a closed claims analysis.
Anesthesiology 1990;72(5):828-833.
|
| 3 |
Apfelbaum JL, Hagberg CA, Caplan RA, et al.
Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway.
Anesthesiology 2013;118(2):251-270.
|
| 4 |
Ray S, Rao S, Kaur J, Gaude YK.
Ratio of height-to-thyromental
distance and ratio of height-to-sternomental
distance as predictors of laryngoscopic grade in children.
J Anaesthesiol Clin Pharmacol 2018;34(1):68-72.
|
| 5 |
Workeneh SA, Gebregzi AH, Denu ZA.
Magnitude and predisposing factors of difficult airway during induction of general anaesthesia.
Anesthesiol Res Pract
2017;2017:5836397.
|
| 6 |
Patil V, Stehling L, Zauder H, Watson C.
Fiberoptic endoscopy
in anesthesia.
Anesthesiology 1984;60(6):623.
|
| 7 |
Schmitt HJ, Kirmse M, Radespiel-Troger M.
Ratio of patient’s height to thyromental distance improves prediction of difficult laryngoscopy.
Anaesth Intensive Care
2002;30(6):763-765.
|
| 8 |
Farzi F, Mirmansouri A, Forghanparast K, Abdolahzade M, Shafai A.
Ratio of height to sternomental distance; a comparison of common upper airway tests for predicting difficult laryngoscopy in elective surgical patients.
Professional Med J 2012;19(6):863-871.
|
| 9 |
Cormack RS, Lehane J.
Difficult tracheal intubation in
obstetrics.
Anaesthesia 1984;39(11):1105-1111.
|
| 10 |
Tse JC, Rimm EB, Hussain A.
Predicting difficult endotracheal
intubation in surgical patients scheduled for general
anesthesia: a prospective blind study.
Anesth Analg
1995;81(2):254-258.
|
| 11 |
Knill RL.
Difficult laryngoscopy made easy with a “BURP”.
Can J Anaesth 1993;40(3):279-282.
|
| 12 |
Kaniyil S, Anandan K, Thomas S.
Ratio of height to thyromental distance as a predictor of difficult laryngoscopy: a prospective observational study.
J Anaesthesiol Clin Pharmacol 2018;34(4):485-489.
|
| 13 |
Ramadhani SAL, Mohamed LA, Rocke DA, Gouws E.
Sternomental distance as the sole predictor of difficult laryngoscopy in obstetric anaesthesia.
Br J Anaesth
1996;77(3):312-316.
|
| 14 |
Safavi M, Honarmand A, Zare N.
A comparison of the
ratio of patient’s height to thyromental distance with
the modified Mallampati and the upper lip bite test
in predicting difficult laryngoscopy.
Saudi J Anaesth
2011;5(3):258-263.
|