To the Editor,
In 1986, Altemir introduced an alternative submental route for endotracheal intubation.1 After three decades passed, over 2,000 patients undergone this surgical airway were reviewed and reported with fewer complications comparing to conventional tracheostomy with fewer risks of emphysema and scar revision.2,3
A 16-year-old female patient was diagnosed with Le Fort I plus II fracture due to a traffic accident. The nasotracheal intubation was not appropriate for the involvement of bony structure around the nasal area, and the patient also denied the tracheostomy. Submental intubation was suggested and performed by the oral and maxillofacial surgeons.
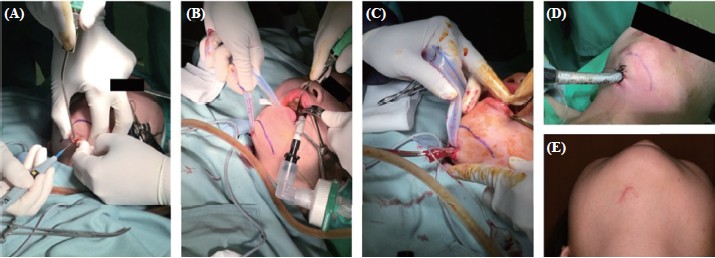
There was no anatomical facial defect on the outer appearance of the patient, and the preoxygenation was done with 100% O2. The propofol (150.0 mg), fentanyl (0.1 mg), and rocuronium (50.0 mg) were induced, and the orotracheal intubation was performed with a non-kinking endotracheal (7.0 mm ID, Lo-Contour Oral/Nasal Tracheal Tube Cuffed; Mallinckrodt, Staines, UK) underuse of video-assisted laryngoscope (McGRATHTM MAC Video Laryngoscope Evolution; Aircraft Medical Ltd, Edinburgh, UK) by an experienced anesthesiologist, and the endotracheal tube was then supplied with 60% O2 and 2% sevoflurance for maintenance. Another submental line was marked by the oral and maxillofacial surgeon, where a 1.5 cm incision was performed one fingering aside the submental line (Figure 1A). With blunt dissection by mosquito forceps, a cutaneo-hypoglossal tunnel was constructed. Kelly forceps, accompanied with a long Penrose drain, were introduced to make sure the tunnel patent (Figure 1B). After disconnection of the connector of the endotracheal tube, Kelly forceps were used to grasp the tube and pull it out from the hypoglossal area (Figure 1C). The non-kinking endotracheal tube was then fixed at 24.0 cm on the skin with 3.0 Nylon suture line after checking in the right position with bilateral clear breathing sound, which was soon applied with maintained inhalation gas (Figure 1D). As the operation was finished, the endotracheal tube was pulled out from the mouth, and the incised wound was sealed with a suture.
Download full-size image
(A) A 1.5 cm incision made one fi ngering aside the submental line. (B) A cutaneo-hypoglossal tunnel created after blunt dissection and a long Penrose drain to ensure the tunnel patent. (C) Using Kelly forceps to grasp the endotracheal tube and pull it out from the hypoglossal area after removal of the connector. (D) A non-kinking endotracheal tube fi xed at 24.0 cm on the skin. (E) Scar after submental incision in this patient.
Complex fractures of multiple facial bones and mandible contribute to a challenge for our anesthesiologist due to sharing the same upper airway field with the surgeon.4 The instability of bone structure and hidden fracture of nasoorbitoethmoidal unit might be the contraindication of nasal airway placement. Though tracheostomy was a temporally selection, the difficulty of post-operative care and dissatisfactions seem to be trouble.5 The major advantage of submental intubation was the facilitation of oronasal surgery, which shared the same opening with the airway. Comparing to tracheostomy, submental intubation exhibited fewer complications such as pneumothorax, pneumonia, surgical emphysema, tracheal stenosis, and tracheomalacia.6 However, surgical wounds increased the risk of infection, and later the scar contributes post-operative dissatisfaction (Figure 1E). Besides, the invasive tunneling procedure needed a thoroughly pre-operative planning, which also increased the risk of trauma to sublingual nerves and vessels. People with obesity, retracted mandible, heavy beard, undergone radiation therapy, or any anatomical anomalies were also potentially not suitable for submental intubation.7 The most important thing is that post-operative care for submental intubation became difficult for the increasing possibility of accidentally pulled out, and the wound care also increased the burden of clinical care. Pulling out the endotracheal tube from the oral space and sealing the incision wound was inevitable after surgery.
Though there is a limitation that the submental intubation was only suitable for patients not requiring prolonged intubation and with lots of concerns about post-operative care, it remains an ideal alternative to nasotracheal, orotracheal intubation, and even tracheostomy for people with complex facial bone fractures.
References
| 1 |
Jundt JS, Cattano D, Hagberg CA, Wilson JW
Submental intubation: a literature review.
Int J Oral Maxillofac Surg. 2012;41(1):46-54.
|
| 2 |
Lim D, Ma BC, Parumo R, Shanmuhasuntharam P.
Thirty years of submental intubation: a review.
Int J Oral
Maxillofac Surg. 2018;47(9):1161-1165.
|
| 3 |
Goh EZ, Loh NHW, Loh JSP.
Submental intubation in oral
and maxillofacial surgery: a systematic review 1986–2018.
Br J Oral Maxillofac Surg. 2020;58(1):43-50.
|
| 4 |
Cheong Y, Kang SS, Kim M, Son HJ, Park J, Kim JM.
Submental
intubation in patients with complex maxillofacial
injuries.
J Lifestyle Med. 2016;6(2):68-71.
|
| 5 |
Das S, Das TP, Ghosh PS.
Submental intubation: a journey
over the last 25 years.
J Anaesthesiol Clin Pharmacol. 2012;28(3):291-303.
|
| 6 |
Kita R, Kikuta T, Takahashi M, et al.
Efficacy and complications
of submental tracheal intubation compared with
tracheostomy in maxillofacial trauma patients.
J Oral Sci.
2016;58(1):23-28.
|
| 7 |
Emara TA, El-Anwar MW, Omara TA, Anany A, Elawa IA, Rabea MM.
Submental intubation versus tracheostomy in maxillofacial fractures.
Oral Maxillofac Surg.
2019;23(3):337-341.
|