Abstract
During coronavirus disease 2019 (COVID-19) pandemic, efforts have been made to rethink the health system and provide various recommendations to the best care of patients and for the protection of health personnel. In patients with suspicion or confirmation of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) who require surgical intervention and anesthetic management, strategies must be established to minimize aerosol-generating procedures. Regional anesthesia (RA) is not considered an aerosol-generating procedure per se and is currently proposed such as a safe strategy and part of comprehensive perioperative care. However, the preoperative evaluation has undergone changes in the context of the COVID-19 pandemic, so in addition to routine preoperative evaluation, a patient-oriented history, clinical, laboratory, and radiologic evaluation should be performed, and a series of general recommendations should be taken into account before, during, and after the performance of RA procedure. A search of PubMed/MEDLINE, Web of Science, and Google Scholar databases was performed until August 22, 2020, using the words: “regional anesthesia or nerve block or peripheral nerve block or spinal anesthesia or epidural anesthesia and SARS-CoV-2 or COVID-19 or MERS or SARS-CoV-1 or infl uenza.” We included in this review all articles, regardless of design, published in the English language. Given the benefi ts reported with the use of RA techniques, both for the patient and for healthcare personnel, it has recently been suggested that RA should be considered as the fi rst choice. However, it is important to generate more precise and homogeneous management guidelines based on the evidence obtained every day during the care of patients with COVID-19.
Keywords
COVID-19 pandemic, neuraxial anesthesia, obstetric anesthesia, peripheral nerve blocks, regional anesthesia, SARS-CoV-2
Introduction
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Most coronavirus infections in humans are mild, although SARS-CoV-2, as well as SARSCoV and Middle East respiratory syndrome coronavirus (MERS-CoV), can cause potentially fatal severe respiratory tract infections.1-4 Patients who require surgical intervention and anesthetic management have the possibility of being sick or infected with SARS-CoV-2 without knowing it, so prevention strategies should be established to reduce exposure to respiratory tract secretions and minimize aerosol generating procedures such as general anesthesia (GA), and thus reduce the risk of perioperative viral transmission both for healthcare personnel and for other patients.5 For this reason, if possible and in order to avoid manipulation of the airway in surgical patients both confirmed and suspected of infection by SARS-CoV-2, the use of regional anesthesia (RA) techniques has been proposed, as a safe and attractive alternative.6 In order to synthesize the information available to date, we perform a narrative review focused on the use of RA techniques in the context of SARS-CoV-2 infection.
Search Strategy
A search of the literature available in PubMed/MEDLINE, Web of Science, and Google Scholar electronic databases up to August 22, 2020, was carried out. The keywords “regional anesthesia or nerve block or peripheral nerve block or spinal anesthesia or epidural anesthesia and SARS-CoV-2 or COVID-19 or MERS or SARS-CoV-1 or influenza” were used, and all articles published in English language, regardless of design, whose summaries included information related to personal protective equipment (PPE), preoperative evaluation, risk and benefits of RA techniques in the context of coronavirus, particularly SARS-CoV-2 infection, were included.
PPE
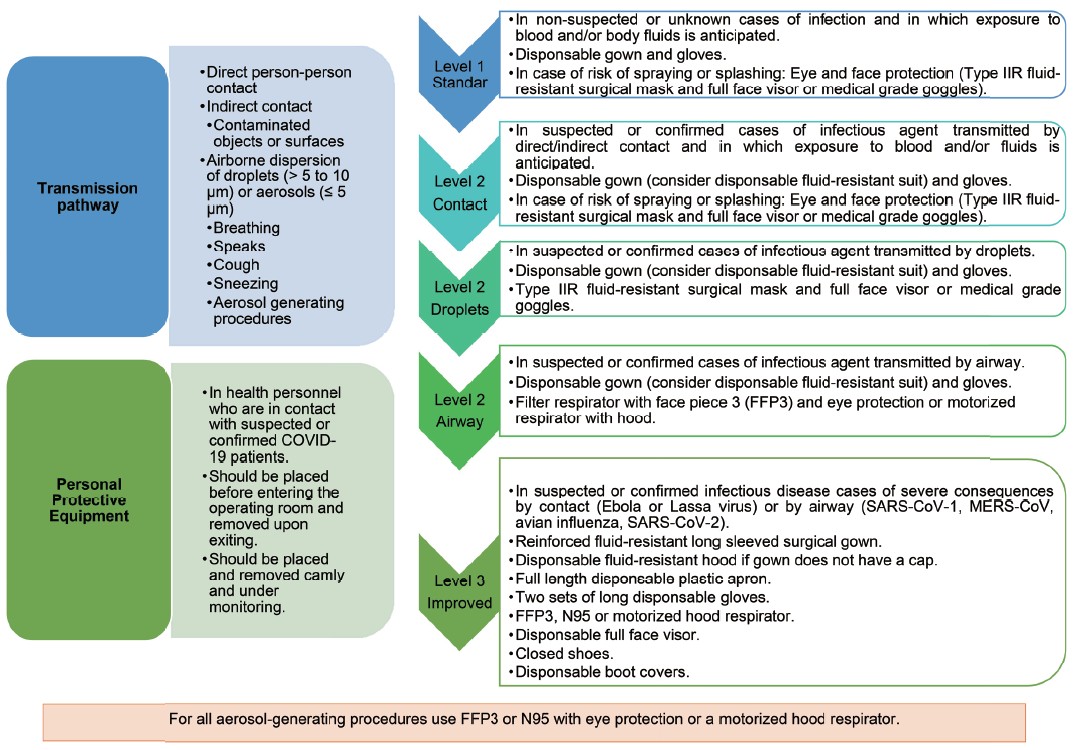
Given the main routes of transmission of SARSCoV-2,7-12 the use of PPE is recommended for healthcare personnel who are in contact with patients with suspected or confirmed SARS-CoV-2 infection.
The administration of RA is not considered an aerosol-generating procedure per se, and at a minimum, the use of droplet protection is recommended.13-15 The size of droplets and aerosols, as well as inertia, gravity, temperature, humidity, evaporation, turnover, and airflow in a space determine how far they disperse, how long they remain floating, and probably how much they affect viral viability.10,11,16,17 Therefore, in the course of the pandemic, more specific recommendations have been issued on the level of PPE to use.13,15,18-24 A higher level of protection is necessary particularly in prolonged surgeries (≥ 120 minutes) and in anatomical regions close to the head and neck,23,25 including the upper extremities;26 spinal anesthesia;13,27 with the possibility of failed blockages, the need for ventilation or conversion to GA that warrants aerosol-generating procedures.13,23,28-30
A study by Zhong and colleagues,18 showed a SARS-CoV-2 viral transmission frequency of 11.36% (5 of 44) in anesthesiologists who administered subarachnoid block to 49 COVID-19 patients. It was observed that 4 of the 7 anesthesiologists who used level 1 PPE (57.1%) and only 1 of the 37 anesthesiologists who used level 3 PPE (2.7%) were infected, so the use of level 3 PPE showed a reduction in relative risk (RR) of 95.3% (95% confidence interval [CI], 63.7–99.4).
Under ideal conditions and with adequate availability of material and supplies, it is justified to use the same level of PPE for RA and for GA (Figure 1).20
For the patient, the use of a surgical mask is recommended throughout their hospital stay.
Download full-size image
Abbreviations: COVID-19, coronavirus disease 2019; SARS-CoV-1, severe acute respiratory syndrome coronavirus 1; MERS-CoV, Middle East respiratory syndrome coronavirus.
Benefits of RA
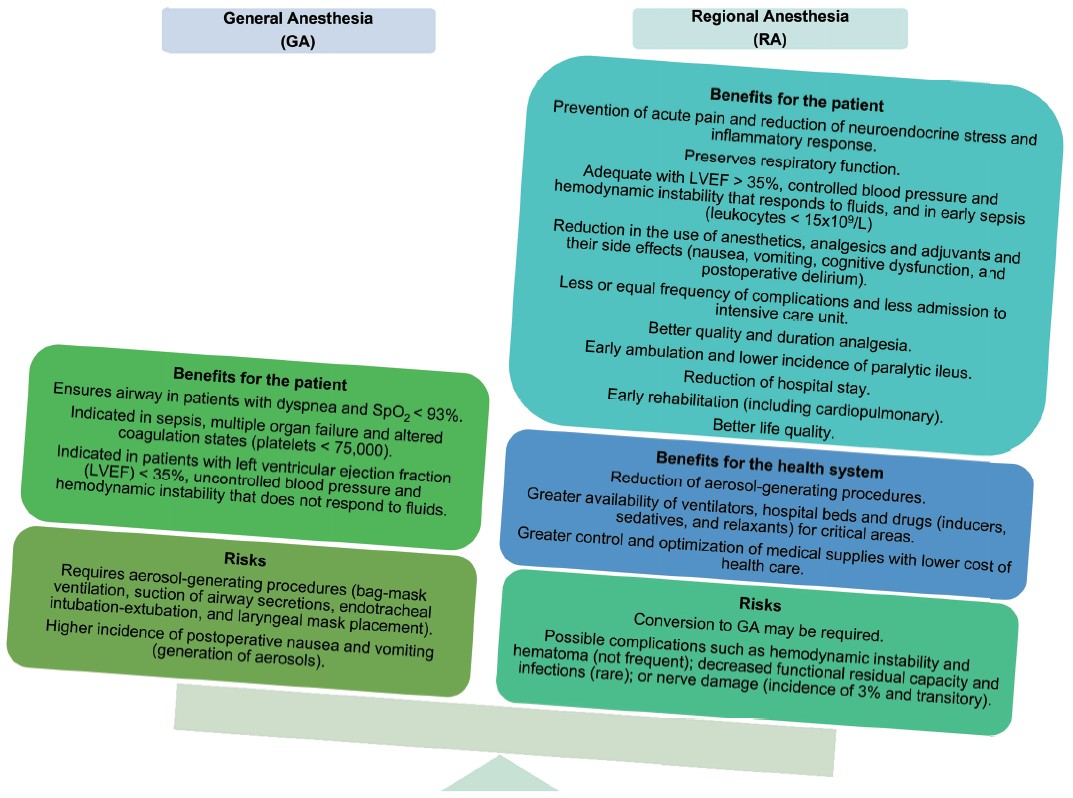
RA is currently considered a safe strategy and part of comprehensive perioperative care, since when compared with GA, it has been associated with multiple benefits.15,31-34 In addition, a lower frequency of pulmonary complications, acute renal failure, thromboembolic events, blood transfusions,35 pneumonia (RR, 0.45; 95% CI, 0.26–0.79) and mortality (zero mortality 30 days after surgery: RR, 0.71; 95% CI, 0.53–0.94), as well as a similar prevalence of cardiac complications (myocardial infarction: RR, 1.17; 95% CI, 0.57–2.37)36 or gastrointestinal complications, intensive care unit admissions, and nerve damage35 than when performing GA. When a neuraxial block is used as a complement to GA compared to GA alone, neither the risk of myocardial infarction (RR, 0.69; 95% CI, 0.44–1.09) or mortality (RR, 1.07; 95% CI, 0.76–1.51) is modified, although the risk of pneumonia is reduced (RR, 0.69; 95% CI, 0.49–0.98).15,32,36-43
GA has also been associated with a higher incidence of nausea and vomiting in the postoperative period;15,32 therefore, if the clinical, respiratory,43 and coagulation status40,44,45 is adequate, neuraxial or peripheral blocks may be optimal for performing limb, abdominal, gynecological, and even urological surgeries safely.29,32,38,46-48 Additionally, through indirect and direct mechanisms, neuraxial anesthesia influences platelet function with antithrombotic effects,49 so it could be useful for the management of surgical patients with COVID-19 in whom a state of hypercoagulability with risk of venous thromboembolism has been reported.
RA techniques can constitute an alternative to reduce the use of the aerosol-generating procedures that are usually used during GA.50 The risk is mainly for the anesthesiologist, who is in direct contact and at a closer distance to the patient;51 in fact, endotracheal intubation is considered an independent risk factor for the acquisition of SARS-CoV infection, with a higher risk (odds ratio [OR], 8.8; 95% CI, 5.3–14.4) of transmission to health personnel.52
RA also reduces health care costs compared to GA,25,53-55 which in a health crisis such as the COVID-19 pandemic is momentous.
Finally, RA should be carried out with the greatest possible precision, minimum risk of failure, and anticipation of all possible scenarios, since timely attention to each situation is key to maintaining anesthetic and surgical safety (Figure 2).18,56,57
Download full-size image
Preoperative Evaluation and Selection of Anesthetic Technique
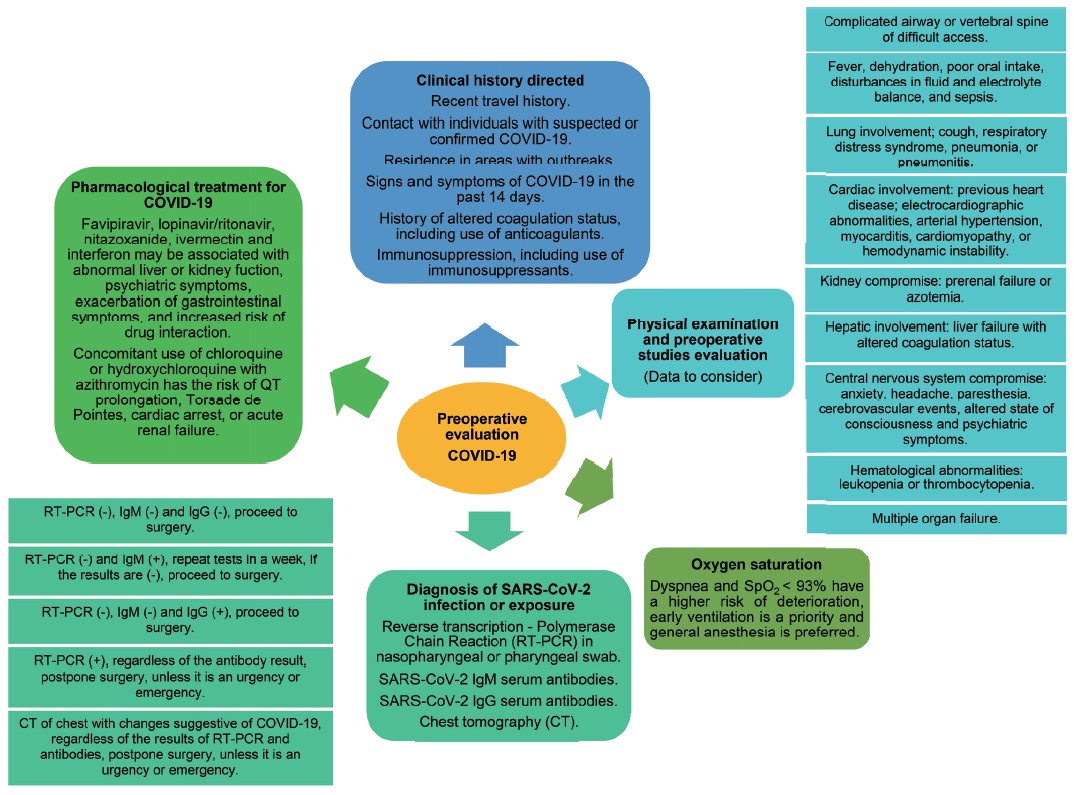
The preoperative evaluation has changed in the context of the COVID-19 pandemic, so far without optimal methods being available.41,54 In addition to routine preoperative evaluation, a patient-oriented history, clinical, laboratory, and radiologic evaluation should be performed with suspected or confirmed COVID-19.41,46 Reverse transcription polymerase chain reaction (RT-PCR) for the detection of SARSCoV-2 RNA and chest tomography are the tests most frequently requested before surgical intervention.54 Some authors have suggested performing RT-PCR only in suspected cases,32 while others suggest it for all patients,58 preferably 24–72 hours before surgery.23,59 The Centers for Disease Control and Prevention have suggested performing RT-PCR or antigenic tests in individuals with signs and symptoms of COVID-19, asymptomatic individuals with suspected or confirmed exposure to SARS-CoV-2, asymptomatic individuals without exposure to the virus for early identifi cation in special situations (which could be applied to patients who will undergo surgery), in individuals in whom it is desired to confi rm that the infection has been resolved and finally, as part of the public health surveillance programs.60
Regarding chest tomography, most guidelines suggest its performance in all cases upon surgical admission, since it can show relevant changes and pulmonary targets even in false negative patients on RT-PCR.61,62 The estimated false negative rate oropharyngeal exudate based on chest tomography for the diagnosis of COVID-19 has been reported from 17.0%63 to 60.5%64. However, not only the sensitivity and specificity of chest computed tomography should be taken into account, but the consequences associated with radiation exposure.65
Serological tests can be used to complement the results of RT-PCR for the diagnosis of COVID-19, as long as they have been validated.23
Precautions, when selecting and using RA techniques in patients with suspected or diagnosed COVID-19, are the same as for the negative patient; and local anesthetics should be adjusted especially in states of acidosis.15,23
The severity of COVID-19 and the clinical status of the patient should be carefully evaluated before selecting a specific anesthetic technique, particularly in those conditions that could increase the risk of complications,40,44,66-68 or repres contraindications for neuraxial procedures.43,69
Evidence on the safety of neuraxial anesthesia in febrile or infected patients70,71 has shown a very low incidence of complications (including viral or bacterial spread to the central nervous system) from pre-existing or severe infections72 in patients with immunosuppression,56 so there is no strict contraindication in these cases.69 Even though the neurotrophic potential of SARS-CoV-2 has been proposed,71,73 the procedure can be carried out safely as long as it is well founded and carried out with adequate protection and asepsis measures, avoiding cerebrospinal fluid leakage.73,74
In the patients with COVID-19, the treatment they are receiving should also be evaluated,43,75,76 given potential adverse effects due to drug interactions.43,75
In the case of emergency surgeries, it is recommended that the selection of the anesthetic technique be made based on the levels of oxygen saturation (SpO2).43
In all cases of patients with suspected or confirmed COVID-19, whenever possible, RA should be considered as the first choice.13 It is important to anticipate and avoid the conversion of a regional technique into GA, which implies communication with the surgeon, mastery of regional anesthetic techniques, and knowledge of surgical pathology, as well as consideration of the physical and emotional characteristics of the patient (Figure 3).
Download full-size image
The anesthesiologist, prior to surgery and as far as possible, must explain to the patient the anesthetic procedure selected according to clinical conditions, risks, and benefi ts, resolve their questions, and obtain their consent and/or that of their relatives or legal representatives in writing. The patient’s understanding of the anesthetic and surgical process will facilitate their cooperation, reducing the need for moderate to deep sedation, and thus reducing the amount of aerosols that could increase the risk of transmission.47
RA
General Recommendations
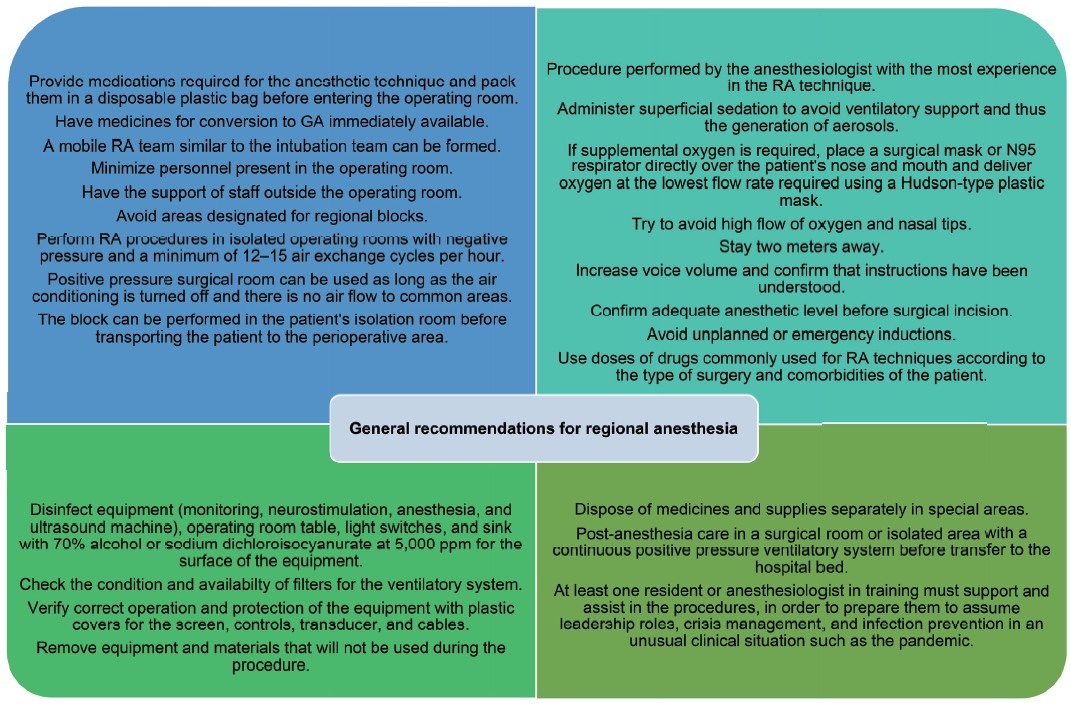
Figure 4 shows a series of general recommendations that should be taken into account before, during, and after the performance of RA procedures.12,13,17,18,20,24,25,30,32,43,57,77-82
Download full-size image
Abbreviations: GA, general anesthesia; RA, regional anesthesia.
Recommendations in Neuraxial Anesthesia
Different gauges and types of needles must be provided for neuraxial blockade even in patients with difficult access to the spinal column.
Despite vasodilation, capillary leakage, and hypotension associated with the inflammatory response to SARS-CoV-2 infection, hemodynamic status can be preserved, although there is the possibility of sustained hypotension during neuraxial blocks, which must be anticipated in order to avoid hypoperfusion of target organs and the presence of nausea or vomiting.83,84
The management of post-puncture headache should begin with conservative and pharmacological treatment according to the clinical situation. If the headache persists, the placement of a blood patch is not recommended given the lack of evidence of its benefit, and the blood deposit in the epidural space that could contain SARS-CoV-2 with the possibility of infection of the central nervous system.13
Recommendations in Obstetric Practice
Epidural analgesia is recommended in patients with COVID-19 due to the hyperventilation and forced exhalation during vocalization and expression of pain associated with labor, with the consequent production of aerosols.
Women in labor should be cared for in the available delivery room closest to the obstetric operating room or directly in an operating room.
An elective caesarean section can be performed with neuraxial block unless there are contraindications. In case of an emergency cesarean section, an epidural block with the use of bicarbonate is recommended to reduce the installation time of the block (3.5 min) compared to a subarachnoid block. Rapid sequence induction is recommended if the catheter is not in place.85
It is known that SARS CoV-2 interacts with the renin-angiotensin-aldosterone system through the angiotensin-converting enzyme 2, which functions as a viral receptor, so the circulatory system could be sensitized and associated with increased hypotension secondary to the administration of spinal anesthesia. In a series of 17 obstetric patients undergoing cesarean section and positive for SARS-CoV-2 infection, excessive hypotension (systolic pressure < 80% of baseline) without target organ damage was reported after administration of epidural block in 12 of 14 patients (85%) compared with none of the 3 patients who received GA, which is why routine preventive use of phenylephrine is recommended after the establishment of epidural block.83
It is recommended to maintain analgesia in labor with automated methods (continuous infusion pumps or patient-controlled analgesia) in order to reduce the traffic of anesthetic personnel in the room. To date, there is no evidence that contraindicates the use of non-steroidal anti-inflammatory drugs for the management of postpartum pain in patients with COVID-19, so they can be utilized.85 Although antiemetics should be administered to prevent postoperative vomiting, the use of dexamethasone should be carefully evaluated,85 given the limited evidence available to date on the impact of the use of steroids for prophylaxis of nausea and vomiting in the context of SARS-CoV-2 infection.
Recommendations in Peripheral RA (Peripheral Nerve Block)
There must be adequate communication with the surgical team, evaluating the innervation zones according to the surgical approach and the approximate duration of surgery, in order to carry out the safest and most effective block for the patient and the procedure.25
Intraoperative conversion of a peripheral block to GA is not recommended, although its concomitant administration can be planned. The American Society of Regional Anesthesia and Pain Medicine does not recommend routine use of peripheral nerve blocks in anesthetized adult patients, as it is believed that the awake state of the patient allows for the detection of systemic local anesthetic systemic toxicity (LAST) or of impending peripheral nerve injury. However, when comparing the relatively low incidence of long-term neurological injury (0.04%) and LAST (0.1%)86,87 with the highly contagious nature of COVID-19 and its high mortality rate in susceptible individuals,67 the block can be performed followed by a planned and scheduled endotracheal intubation or, although less advisable, to have a secured airway and subsequently perform peripheral regional techniques,34 to obtain mixed anesthesia.
Ultrasound guidance may not reduce the risk of nerve injury, but it has shown a 65% reduction in the incidence of LAST,67,88 so all procedures should be guided by ultrasound and neurostimulation, and if available, can be used together.34
Sedation is optional and it is recommended that it be superficial with midazolam 0.01–0.03 mg/kg and/or fentanyl 0.25–1.00 μg/kg, at the discretion of the anesthesiologist in charge89 or with dexmedetomidine of 0.1–0.4 μg/kg/h, given its minimal effects on respiration.15,19,90
For peripheral nerve blocks, it is preferable to use short or intermediate-acting local anesthetics to avoid a stay in the post-anesthesia recovery unit. The duration of the block should be adequate for the surgical procedure; therefore, the use of local anesthetic mixtures of short/intermediate and long action or the placement of a perineural catheter can be considered,24 always monitoring for the presence of LAST.25
Given the need for prolonged blockade time, it is necessary to evaluate the theoretical risk-benefit of the routine use of adjuvants such as dexamethasone due to potential immunosuppression, or clonidine or dexmedetomidine due to infrequent side effects such as sedation, bradycardia, or hypotension.25,26
Due to the risk of thrombocytopenia and bleeding disorders in patients with COVID-19, coagulation tests and platelet count should be performed postoperatively in all patients undergoing deep blockages or perineural catheter placement in interscalene approaches, supra and infraclavicular, lumbar plexus block, or sciatic nerve block in transgluteal, anterior, and parasacral approaches.24
During brachial plexus blocks, special attention should be paid to patients with compromised respiration, since blocks above the clavicle carry an inherent risk of both phrenic nerve palsy and pneumothorax, which translates into a risk of up to a 25% decrease in vital capacity and forced expiratory volume. To prevent pneumothorax in the supraclavicular and infraclavicular approaches an ultrasound-guided peripheral nerve block should be performed and the needle tip should always be visualized.24
For the prevention of hemidiaphragmatic paresis, it has been proposed to reduce the volume or concentration of the local anesthetic, however, it has not been possible to reduce the risk to below 20% without increasing the block failure rate. Therefore, to avoid ventilatory compromise, the use of alternative techniques that do not affect diaphragmatic mobility, such as suprascapular nerve block, with or without axillary nerve block or infraclavicular block, is preferred15,26,91 or even with no blockage, especially interscalene blockade. Other alternatives are upper trunk block, infraclavicular brachial plexus block, extrafasial injection, and interfascial injection below the C6 level.24
The combination of some blocks may represent a valid alternative for upper extremity surgery involving dermatomes C5–T1. Open reduction and internal fixation or shoulder arthroplasty (hemiarthroplasty or reverse prosthesis) under interscalene block and supraclavicular block using 30 mL of a 1:1 mixture of 2% mepivacaine and 0.5% levobupivacaine to complete both blocks, in addition to receiving superficial sedation, resulting in adequate surgical anesthesia, has been reported.89 Alternatively, the selective blockade of the trunks (from C5 to T1 individually) guided by ultrasound not including the area of innervation of the intercostobrachial nerve (T2), with a total volume of 25 mL with a mixture of 2% lidocaine with epinephrine 1:200,000 and 0.5% levobupivacaine, resulting in sensory and motor block of the entire limb in 15–20 minutes without affection of the innervation of the diaphragm, also has been reported.90
On the other hand, interfascial plane blocks in any location have become the primary option (whenever possible) for the anesthetic management of patients with suspected COVID-19 infection.92
Performing a minimally invasive peripheral technique, such as erector spinae muscle plane block, as part of multimodal pain management can also be considered a safe and effective procedure for postoperative pain.32
The combination of neuraxial anesthesia and peripheral femoral block without any type of sedation, in the management of elderly patients with femoral neck fracture, achieving surgical results and adequate postoperative pain control without increased postoperative morbidity, has been reported.42
If it is necessary to prolong a block, infiltration of the surgical site, use of rescue blocks25, or the use of tumescence anesthesia is feasible.23
Sphenopalatine ganglion block at the nasal level is a treatment described for post-puncture headache, which involves the insertion of long cotton swabs into the nasal cavity to continuously deposit local anesthetic. It should not be performed routinely, as it is unknown whether it could generate aerosols.27,29,57
The decision to leave a perineural catheter, which may require repeated contact with the patient, must be evaluated in each individual case. Kilicaslan et al.79 reported the use of continuous femoral and popliteal sciatic block with 6 minutes to perform both blocks. To evaluate the success of both blocks, analgesia in the innervation areas was meticulously corroborated, so surgery began 20 minutes after performing the blocks. No complications were reported during surgery or postoperatively, so in the hands of experienced operators, peripheral nerve blocks are the first option for surgeries during the pandemic.
The use of continuous peripheral nerve blocks for all patients with COVID-19 in whom more than one surgical procedure is planned or who have significant prolonged postoperative pain has been recommended.30 Performing the blocks in the patient’s isolation room, using standard monitors and minimal sedation with intravenous midazolam and fentanyl, as that allows for the evaluation of the block’s adequacy, and then proceeding to the operating room, has been suggested. This practice ensures that the block works properly for surgery and minimizes time spent in the operating room for both the patient and the anesthesiologist. In addition, with a functional continuous nerve block, debridements or other small procedures that are commonly performed in the operating room can be performed at the bedside. Finally, the improved analgesia in patients with continuous nerve blocks allows for them to be discharged from the surgical service and returned to isolation more quickly than with the use of single-dose nerve blocks.
Conclusions
RA techniques have been used in pandemics caused by previous respiratory infections, such as those caused by the SARS-CoV, MERS, and influenza AH1N1 viruses. However, the experience obtained has not generated sufficient evidence to make solid recommendations on the indications and contraindications for the use of RA, which can be extrapolated to the care of patients with SARS-CoV-2 infection. Currently, there is no single optimal anesthetic management technique for COVID-19 patients, as there are arguments both for and against the use of GA and RA. Given the benefits reported during the COVID-19 pandemic with the use of RA techniques by experienced anesthesiologists, both for the patient and for healthcare personnel, it has recently been suggested that RA should be considered as the first choice. It is extremely important to consider different clinical scenarios, as well as to make a coordinated effort to generate more precise and homogeneous management guidelines based on the evidence obtained every day during the care of patients with COVID-19.
Conflict of Interest
The authors have no conflict of interest to declare.
Funding
This work was not funded.
Acknowledgments
We thank Douglas C Nance (Professor-Associated C Researcher TC, Universidad de la Sierra Sur, Instituto de Investigación sobre la Salud Pública, Miahuatlán de Porfirio Díaz, Oaxaca, Mexico; a native speaker of English) for technical English assess.
We thank Carla Elizabeth Contreras-Rincon (Anesthesiology Service, Hospital Angeles Pedregal, Mexico City, Mexico) for their support in the search for information on RA in obstetrics.
References
| 1 |
Zhu N, Zhang D, Wang W, et al.
A novel coronavirus
from patients with pneumonia in China, 2019.
N Engl J
Med. 2020;382(8):727-733.
|
| 2 |
Chan JFW, Lau SKP, To KKW, Cheng VCC, Woo PCY, Yuen KY.
Middle East respiratory syndrome coronavirus: another zoonotic betacoronavirus causing SARSlike disease.
Clin Microbiol Rev. 2015;28(2):465-522.
|
| 3 |
Cheng VCC, Lau SKP, Woo PCY, Yuen KY.
Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection.
Clin Microbiol Rev.
2007;20(4):660-694.
|
| 4 |
To KKW, Tsang OTY, Leung WS, et al.
Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARSCoV-2: an observational cohort study.
Lancet Infect Dis. 2020;20(5):565-574.
|
| 5 |
Peng PWH, Ho PL, Hota SS.
Outbreak of a new coronavirus:
what anaesthetists should know.
Br J Anaesth.
2020;124(5):497-501.
|
| 6 |
Li Q, Guan X, Wu P, et al.
Early transmission dynamics in
Wuhan, China, of novel coronavirus-infected pneumonia.
N Engl J Med. 2020;382(13):1199-1207.
|
| 7 |
Chan JFW, Yuan S, Kok KH, et al.
A familial cluster of
pneumonia associated with the 2019 novel coronavirus
indicating person-to-person transmission: a study
of a family cluster.
Lancet. 2020;395(10223):514-523.
|
| 8 |
Zhang R, Li Y, Zhang AL, Wang Y, Molina MJ.
Identifying
airborne transmission as the dominant route for
the spread of COVID-19.
Proc Natl Acad Sci U S A.
2020;117(26):14857-14863.
|
| 9 |
Kutter JS, Spronken MI, Fraaij PL, Fouchier RA, Herfst S.
Transmission routes of respiratory viruses among humans.
Curr Opin Virol. 2018;28:142-151.
|
| 10 |
Prather KA, Wang CC, Schooley RT.
Reducing transmission
of SARS-CoV-2.
Science. 2020;368(6498):1422-1424.
|
| 11 |
Asadi S, Bouvier N, Wexler AS, Ristenpart WD.
The coronavirus
pandemic and aerosols: does COVID-19 transmit
via expiratory particles?
Aerosol Sci Technol. 54(6):635-638.
|
| 12 |
van Doremalen N, Bushmaker T, Morris DH, et al.
Aerosol
and surface stability of SARS-CoV-2 as compared with
SARS-CoV-1.
N Engl J Med. 2020;382(16):1564-1567.
|
| 13 |
Uppal V, Sondekoppam RV, Landau R, El-Boghdadly K, Narouze S, Kalagara HKP.
Neuraxial anaesthesia and
peripheral nerve blocks during the COVID-19 pandemic:
a literature review and practice recommendations.
Anaesthesia.
2020;75(10):1350-1363.
|
| 14 |
Mejía-Terrazas GE, López-Muñoz E.
Implications of
COVID-19 (SARS-CoV-2) for the anesthesiological
practice.
Medwave. 2020;20(6):e7950.
|
| 15 |
Lie SA, Wong SW, Wong LT, Wong TGL, Chong SY.
Practical
considerations for performing regional anesthesia:
lessons learned from the COVID-19 pandemic.
Can J
Anaesth. 2020;67(7):885-892.
|
| 16 |
Tellier R, Li Y, Cowling BJ, Tang JW.
Recognition of
aerosol transmission of infectious agents: a commentary.
BMC Infect Dis. 2019;19(1):101.
|
| 17 |
Nicas M, Nazaroff WW, Hubbard A.
Toward understanding
the risk of secondary airborne infection: emission of respirable pathogens.
J Occup Environ Hyg.
2005;2(3):143-154.
|
| 18 |
Zhong Q, Liu YY, Luo Q, et al.
Spinal anaesthesia for
patients with coronavirus disease 2019 and possible
transmission rates in anaesthetists: retrospective, single-centre, observational cohort study.
Br J Anaesth.
2020;124(6):670-675.
|
| 19 |
Lie SA, Wong SW, Wong LT, Wong TGL, Chong SY.
In reply:
Regional anesthesia during the COVID-19 pandemic:
a time to reconsider practices? (Letters #1 and #2).
Can J
Anaesth. 2020;67(9):1286-1287.
|
| 20 |
Erbabacan E, Özdilek A, Beyoğlu ÇA, Altındaş F.
Perioperative
anaesthetic management of confirmed or suspected
COVID-19 patients.
Turk J Anaesthesiol Reanim.
2020;48(3):180-187.
|
| 21 |
Public Health England.
COVID-19: guidance for maintaining
services within health and care settings: infection
prevention and control recommendations (version 1.2).
GOV. UK. Accesed July 30, 2021.
|
| 22 |
Health Protection Scotland.
Appendix 16—best practice—
aide memoire for levels of personal protective equipment (ppe) for healthcare workers when providing patient care.
National Services Scotland.
National Services Scotland. Published February 11, 2019.
Accessed August 22, 2020.
|
| 23 |
Kaye K, Paprottka F, Escudero R, et al.
Elective, non-urgent
procedures and aesthetic surgery in the wake of
SARS-COVID-19: considerations regarding safety, feasibility and impact on clinical management.
Aesthetic Plast
Surg. 2020;44(3):1014-1042.
|
| 24 |
Mendes ÂB, Penedos C, Rodrigues LV, Varandas J, Lages N, Machado H.
The role of locoregional anesthesia in the covid-19 pandemic.
Acta Médica Portuguesa. 2020;33(7-8):522-527.
|
| 25 |
Macfarlane AJR, Harrop-Griffiths W, Pawa A.
Regional anaesthesia and COVID-19: first choice at last?
Br J Anaesth.
2020;125(3):243-247.
|
| 26 |
Herman JA, Urits I, Kaye AD, Urman RD, Viswanath O.
COVID-19: recommendations for regional anesthesia.
J Clin Anesth. 2020;65:109885.
|
| 27 |
Du Y, Wang L, Wu G, Lei X, Li W, Lv J.
Anesthesia and protection in an emergency cesarean section for pregnant woman infected with a novel coronavirus: case report and literature review.
J Anesth. 2020;34(4):613-618.
|
| 28 |
Uppal V, Sondekoppam RV, Lobo CA, Kolli S, Kalagara HK.
Practice recommendations on neuraxial anesthesia
and peripheral nerve blocks during the COVID-19
Pandemic. A joint statement by the American Society of
Regional Anesthesia and Pain Medicine (ASRA) and European
Society of Regional Anesthesia and Pain Therapy
(ESRA).
ASRA/ESRA. Published March 31, 2020. Accessed
September 11, 2020.
|
| 29 |
Lima RME, Reis L de A, Thyrso de Lara FS, et al.
Recommendations for local-regional anesthesia
during the COVID-19 pandemic.
Braz J Anesthesiol.
2020;70(2):159-164.
|
| 30 |
Finneran JJ, Said ET, Curran BP, Gabriel RA.
The use of
continuous perineural catheters and other practices to
optimize regional anesthesia in COVID-19 patients.
Can
J Anaesth. 2020;67(11):1665-1666.
|
| 31 |
Bugada D, Ghisi D, Mariano ER.
Continuous regional anesthesia:
a review of perioperative outcome benefits.
Minerva
Anestesiol. 2017;83(10):1089-1100.
|
| 32 |
Fiorelli S, Menna C, Piccioni F, et al.
The cutting edge of
thoracic anesthesia during the coronavirus disease 2019
(COVID-19) outbreak.
J Cardiothorac Vasc Anesth.
2020;34(12):3203-3210.
|
| 33 |
Au Yong PSA, Chan DXH.
Opioid reduction strategies are
important for laparotomies during the covid-19 outbreak.
Reg Anesth Pain Med. 2021;46(2):188.
|
| 34 |
Aliste J, Altermatt F, Atton R, et al.
Recomendaciones
para la ejecución de anestesia regional no obstétrica en
perioperatorio de pacientes COVID-19.
Rev chil anest.
2020.
|
| 35 |
Memtsoudis SG, Cozowicz C, Bekeris J, et al.
Anaesthetic
care of patients undergoing primary hip and knee arthroplasty:
consensus recommendations from the International
Consensus on Anaesthesia-Related Outcomes after
Surgery group (ICAROS) based on a systematic review
and meta-analysis.
Br J Anaesth. 2019;123(3):269-287.
|
| 36 |
Guay J, Choi P, Suresh S, Albert N, Kopp S, Pace NL.
Neuraxial blockade for the prevention of postoperative
mortality and major morbidity: an overview of Cochrane
systematic reviews.
Cochrane Database Syst
Rev. 2014;2014(1):CD010108.
|
| 37 |
Varandas JS, Dias R, Mendes AB, Lages N, Machado H.
New indication for an old anesthetic technique: could we consider now rapid sequence spinal anesthesia in a COVID-19 time?
Reg Anesth Pain Med. 2021;46(2):191.
|
| 38 |
Hotta K.
Regional anesthesia in the time of COVID-19:
a minireview.
J Anesth. 2021;35(3):341-344.
|
| 39 |
Lei S, Jiang F, Su W, et al.
Clinical characteristics and
outcomes of patients undergoing surgeries during the incubation
period of COVID-19 infection.
EClinicalMedicine.
2020;21:100331.
|
| 40 |
Lirk P, Hollmann MW.
Outcome after regional anesthesia:
weighing risks and benefits.
Minerva Anestesiol.
2014;80(5):610-618.
|
| 41 |
Chhabra HS, Bagaraia V, Keny S, et al.
COVID-19: current
knowledge and best practices for orthopaedic surgeons.
Indian J Orthop. 2020;54:411-425.
|
| 42 |
Catellani F, Coscione A, D’Ambrosi R, Usai L, Roscitano
C, Fiorentino G.
Treatment of proximal femoral fragility
fractures in patients with COVID-19 during the SARSCoV-
2 outbreak in Northern Italy.
J Bone Joint Surg Am.
2020;102(12):e58.
|
| 43 |
Ashokka B, Chakraborty A, Subramanian BJ, Karmakar
MK, Chan V.
Reconfiguring the scope and practice
of regional anesthesia in a pandemic: the COVID-19
perspective.
Reg Anesth Pain Med. 2020;45(7):536-543.
|
| 44 |
Mendes AB, Penedos C, Vaz Rodrigues L, Varandas JS,
Lages N, Machado H.
Coagulation concerns in patients
with COVID-19 proposed for regional anesthesia.
Reg
Anesth Pain Med. 2021;46(5):457.
|
| 45 |
Bauer ME, Toledano RD, Houle T, et al.
Lumbar
neuraxial procedures in thrombocytopenic patients
across populations: a systematic review and meta-analysis.
J Clin Anesth. 2020;61:109666.
|
| 46 |
Singleton MN, Soffin EM.
Daring discourse: are we ready
to recommend neuraxial anesthesia and peripheral nerve
blocks during the COVID-19 pandemic? A pro-con.
Reg
Anesth Pain Med. 2020;45(10):831-834.
|
| 47 |
Romanzi A, Galletti M, Macchi L, et al.
Awake laparotomy:
is locoregional anesthesia a functional option for major
abdominal surgeries in the COVID-19 era?
Eur Rev
Med Pharmacol Sci. 2020;24(9):5162-5166.
|
| 48 |
Ti LK, Ang LS, Foong TW, Ng BSW
What we do when a
COVID-19 patient needs an operation: operating room
preparation and guidance.
Can J Anaesth. 2020;67(6):756-
758.
|
| 49 |
Kettner SC, Willschke H, Marhofer P.
Does regional anaesthesia really improve outcome?
Br J Anaesth.
2011;107(Suppl 1):i90-i95.
|
| 50 |
Park MH, Kim HR, Choi DH, Sung JH, Kim JH.
Emergency
cesarean section in an epidemic of the middle east
respiratory syndrome: a case report.
Korean J Anesthesiol.
2016;69(3):287-291.
|
| 51 |
Mistry T, Singh SK.
COVID-19 pandemic: regional anesthesia
should be the new norm!
Reg Anesth Pain Med.
2021;46(2):186-187.
|
| 52 |
Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J.
Aerosol generating procedures and risk of transmission of
acute respiratory infections to healthcare workers: a systematic
review.
PLoS One. 2012;7(4):e35797.
|
| 53 |
Hutton M, Brull R, Macfarlane AJR.
Regional anaesthesia
and outcomes.
BJA Educ. 2018;18(2):52-56.
|
| 54 |
Gökce Mİ, Yin S, Sönmez MG, et al.
How does the
COVID-19 pandemic affect the preoperative evaluation
and anesthesia applied for urinary stones? EULIS eCOREIAU
multicenter collaborative cohort study.
Urolithiasis.
2020;48(4):345-351.
|
| 55 |
Morris MT, Morris J, Wallace C, et al.
An analysis
of the cost-effectiveness of spinal versus general
anesthesia for lumbar spine surgery in various hospital
settings.
Global Spine J. 2019;9(4):368-374.
|
| 56 |
Gimeno AM, Errando CL.
Neuraxial regional anaesthesia
in patients with active infection and sepsis: a clinical narrative
review.
Turk J Anaesthesiol Reanim. 2018;46(1):8-
14.
|
| 57 |
Smiley R.
Spinal anaesthesia and COVID-19 transmission
to anaesthetists. Comment on Br J Anaesth 2020; 124:
670-5.
Br J Anaesth. 2020;125(2):e247-e248.
|
| 58 |
Givi B, Schiff BA, Chinn SB, et al.
Safety recommendations
for evaluation and surgery of the head and neck
during the COVID-19 pandemic.
JAMA Otolaryngol
Head Neck Surg. 2020;146(6):579-584.
|
| 59 |
Dexter F, Elhakim M, Loftus RW, Seering MS, Epstein
RH.
Strategies for daily operating room management of
ambulatory surgery centers following resolution of the
acute phase of the COVID-19 pandemic.
J Clin Anesth.
2020;64:109854.
|
| 60 |
Centers for Disease Control and Prevention (CDC).
Healthcare workers: overview of testing for SARS-CoV-2
(COVID-19).
CDC. Updated September 18, 2020. Accessed
September 19, 2020.
|
| 61 |
Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J.
Chest
CT for typical coronavirus disease 2019 (COVID-19) pneumonia: relationship to negative RT-PCR testing.
Radiology. 2020;296(2):E41-E45.
|
| 62 |
Liu Z, Zhang Y, Wang X, et al.
Recommendations for surgery
during the novel coronavirus (COVID-19) epidemic.
Indian J Surg. 2020;82:124-128.
|
| 63 |
Long C, Xu H, Shen Q, et al.
Diagnosis of the coronavirus
disease (COVID-19): rRT-PCR or CT?
Eur J Radiol.
2020;126:108961.
|
| 64 |
Li Y, Yao L, Li J, et al.
Stability issues of RT-PCR testing
of SARS-CoV-2 for hospitalized patients clinically diagnosed
with COVID-19.
J Med Virol. 2020;92(7):903-908.
|
| 65 |
Kim H, Hong H, Yoon SH.
Diagnostic performance of
CT and reverse transcriptase polymerase chain reaction
for coronavirus disease 2019: a meta-analysis.
Radiology.
2020;296(3):E145-E155.
|
| 66 |
Jiang F, Deng L, Zhang L, Cai Y, Cheung CW, Xia Z.
Review
of the clinical characteristics of coronavirus disease
2019 (COVID-19).
J Gen Intern Med. 2020;35(5):1545-
1549.
|
| 67 |
Soberón JR, Urdaneta F.
Regional anesthesia during
the COVID-19 pandemic: a time to reconsider practices?
(Letter #1).
Can J Anaesth. 2020;67(9):1282-1283.
|
| 68 |
Horlocker TT, Wedel DJ.
Infectious complications of
regional anesthesia.
Best Pract Res Clin Anaesthesiol.
2008;22(3):451-475.
|
| 69 |
Stundner O, Memtsoudis SG.
Regional anesthesia and
analgesia in critically ill patients: a systematic review.
Reg Anesth Pain Med. 2012;37(5):537-544.
|
| 70 |
Wedel DJ, Horlocker TT.
Regional anesthesia in the
febrile or infected patient.
Reg Anesth Pain Med.
2006;31(4):324-333.
|
| 71 |
Aminnejad R, Salimi A, Saeidi M.
Lidocaine during
intubation and extubation in patients with coronavirus
disease (COVID-19).
Can J Anaesth. 2020;67(6):759.
|
| 72 |
Lee AI, Hoffman MJ, Allen NN, Sullivan JT.
Neuraxial
labor analgesia in an obese parturient with influenza
A H1N1.
Int J Obstet Anesth. 2010;19(2):223-226.
|
| 73 |
Baig AM, Khaleeq A, Ali U, Syeda H.
Evidence of the
COVID-19 virus targeting the CNS: tissue distribution,
host-virus interaction, and proposed neurotropic
mechanisms.
ACS Chem Neurosci. 2020;11(7):995-998.
|
| 74 |
Filatov A, Sharma P, Hindi F, Espinosa PS.
Neurological
complications of coronavirus disease (COVID-19):
encephalopathy.
Cureus. 2020;12(3):e7352.
|
| 75 |
Şimşek Yavuz S, Ünal S.
Antiviral treatment of COVID-19.
Turk J Med Sci. 2020;50(SI-1):611-619.
|
| 76 |
Greenland JR, Michelow MD, Wang L, London MJ.
COVID-19 Infection: implications for perioperative and
critical care physicians.
Anesthesiology. 2020;132(6):1346-
1361.
|
| 77 |
Cook TM, El-Boghdadly K, McGuire B, McNarry AF,
Patel A, Higgs A.
Consensus guidelines for managing the
airway in patients with COVID-19: guidelines from the
Difficult Airway Society, the Association of Anaesthetists
the Intensive Care Society, the Faculty of Intensive Care
Medicine and the Royal College of Anaesthetists.
Anaesthesia.
2020;75(6):785-799.
|
| 78 |
Wang E, Mei W, Shang Y, et al.
Chinese Association of
Anesthesiologists Expert Consensus on the use of perioperative
ultrasound in coronavirus disease 2019 patients.
J Cardiothorac Vasc Anesth. 2020;34(7):1727-1732.
|
| 79 |
Kilicaslan A, Kekec AF, Eren AS, Uzun ST.
Peripheral
nerve blocks in a patient with suspected COVID-19
infection.
J Clin Anesth. 2020;65:109853.
|
| 80 |
Binks AC, Parkinson SM, Sabbouh V.
Oxygen: under or
over a surgical facemask for COVID-19 patients?
Anaesthesia.
2020;75(12):1691-1692.
|
| 81 |
Simonds AK, Hanak A, Chatwin M, et al.
Evaluation
of droplet dispersion during non-invasive ventilation,
oxygen therapy, nebuliser treatment and chest physiotherapy
in clinical practice: implications for management
of pandemic influenza and other airborne infections.
Health Technol Assess. 2010;14(46):131-172.
|
| 82 |
Yao W, Wang T, Jiang B, et al.
Emergency tracheal intubation
in 202 patients with COVID-19 in Wuhan, China:
lessons learnt and international expert recommendations.
Br J Anaesth. 2020;125(1):e28-e37.
|
| 83 |
Chen R, Zhang Y, Huang L, Cheng BH, Xia ZY, Meng
QT
Safety and efficacy of different anesthetic regimens
for parturients with COVID-19 undergoing Cesarean
delivery: a case series of 17 patients.
Can J Anaesth.
2020;67(6):655-663.
|
| 84 |
Hanidziar D, Bittner EA.
Hypotension, systemic inflammatory
response syndrome, and COVID-19: a clinical
conundrum.
Anesth Analg. 2020;131(3):e175-e176.
|
| 85 |
Bauer ME, Bernstein K, Dinges E, et al.
Obstetric anesthesia
during the COVID-19 pandemic.
Anesth Analg.
2020;131(1):7-15.
|
| 86 |
Neal JM, Barrington MJ, Brull R, et al.
The second ASRA practice advisory on neurologic complications associated with regional anesthesia and pain medicine: executive summary 2015.
Reg Anesth Pain Med. 2015;40(5):401-
430.
|
| 87 |
Bernards CM, Hadzic A, Suresh S, Neal JM.
Regional
anesthesia in anesthetized or heavily sedated patients.
Reg Anesth Pain Med. 2008;33(5):449-460.
|
| 88 |
Neal JM, Barrington MJ, Fettiplace MR, et al.
The third
American Society of Regional Anesthesia and Pain
Medicine practice advisory on local anesthetic systemic
toxicity: executive summary 2017.
Reg Anesth Pain Med.
2018;43(2):113-123.
|
| 89 |
Tognù A, Barbara E, Pacini I, Bosco M.
Proximal humeral
fracture surgery in the COVID-19 pandemic: advocacy for regional anesthesia.
Reg Anesth Pain Med.
2021;46(4):375-376.
|
| 90 |
Sivakumar RK, Areeruk P, Karmakar MK.
Selective trunk
block (SeTB): a simple alternative to hybrid brachial plexus
block techniques for proximal humeral fracture surgery
during the COVID-19 pandemic.
Reg Anesth Pain
Med. 2021;46(4):376-378.
|
| 91 |
Aliste J, Altermatt FR, Atton R, et al.
Regional anesthesia
during the COVID-19 pandemic: a time to reconsider
practices? (Letter #2).
Can J Anaesth. 2020;67(9):1284-
1285.
|
| 92 |
Altiparmak B, Korkmaz Toker M, Uysal AI, Gümüş
Demi Rbi Lek S.
Regional anesthesia in patients with
suspected COVID-19 infection.
Reg Anesth Pain Med.
2021;46(1):91-92.
|