Abstract
Background: Most of the reports showed that videolaryngoscopy has better outcomes than direct laryngoscopy for nasotracheal intubation. The FKScope® comprises a semirigid and malleable stylet with a terminal camera and has been used to facilitate orotracheal intubation. However, its efficacy and safety for nasotracheal intubation remain unknown. This study compared FKScope® with Macintosh direct laryngoscopy for nasotracheal intubation.
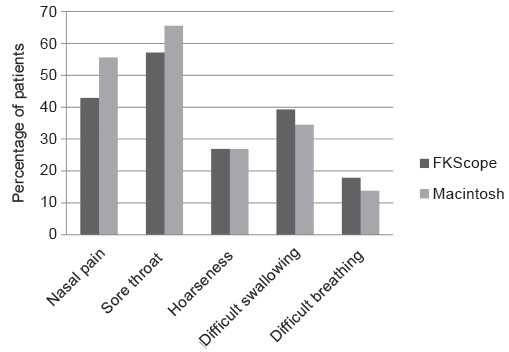
Methods: Sixty-four patients scheduled for oral and maxillofacial surgery requiring nasotracheal intubation were enrolled and randomly assigned to FKScope® (n = 32) or Macintosh group (n = 32). The primary outcome was time to successful intubation during the first attempt. Secondary outcomes included modified nasal intubation difficulty scale (MNIDS) scores; percentage of glottic opening (POGO); immediate postintubation side effects such as mucosal bleeding, dental injury, and lip lacerations; and postoperative side effects including nasal pain, sore throat, hoarseness, dysphagia, and dyspnea.
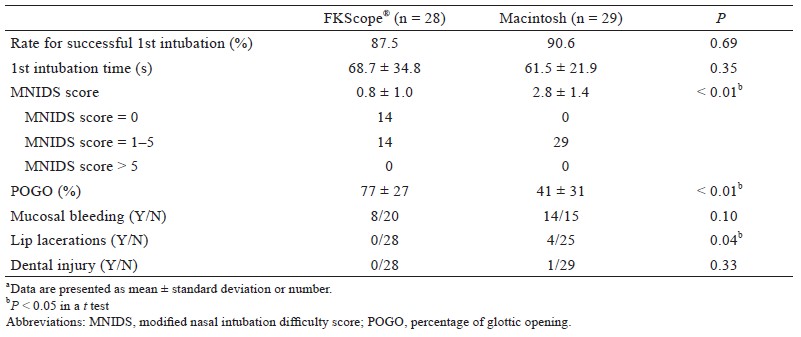
Results: The rates of successful first-attempt intubation were 87.5% and 90.6% in the FKScope® and Macintosh group, respectively (P = 0.69). Mean (± standard deviation) total intubation time was 68.7 ± 34.8 s in the FKScope® group compared with 61.5 ± 21.9 s in the Macintosh group (P = 0.35), despite a higher POGO for the FKScope® group (77 ± 27 vs. 41 ± 31, P < 0.01). The MNIDS scores of the FKScope® group were significantly lower (0.8 ± 1.0 vs. 2.8 ± 1.4, P < 0.01). The groups did not differ significantly regarding most postoperative side effects, although the FKScope® group had fewer lip lacerations (P = 0.04).
Conclusions: The use of FKScope® improves the view of the glottic opening and is safe for nasotracheal intubation with normal airways. However, secretions and blood can obstruct the camera, and therefore, to select the patient carefully is necessary.
Keywords
nasotracheal intubation, oral and maxillofacial surgery, video-assist
Introduction
Nasotracheal intubation is widely used in airway management of general anesthesia for oropharyngeal, dental, and maxillofacial surgery either by direct laryngoscopy or videolaryngoscopy. This intubation technique is also indicated for patients with difficult airways, such as those with questionable cervical spine stability (using awake fiberoptic intubation), intraoral mass lesions or structural abnormalities, and limited mouth opening (e.g., trismus).1 When an anesthesiologist performs nasotracheal intubation, narrow nasal passages and deviate nasal septum occasionally impede the advancement of the nasotracheal tube. The rigid tube tip may cause nasal cavity and nasopharyngeal injury. Because of high vascularity of the whole nasal cavity, especially Little’s area, trauma to the nasal cavity can lead to brisk bleeding. Besides, a large tongue or any oral masses that reduce the space of oral cavity will make manipulation of the endotracheal tube more difficult. Nasotracheal intubation may cause certain complications; epistaxis is the most common, and other complications include bacteremia, partial or complete obstruction of the tube, sinusitis, subcutaneous or mediastinal emphysema, inadvertent intracranial placement of the nasotracheal tube, and retropharyngeal perforation.2 Various types of videolaryngoscopes are available, including integrated channel, video stylet, and rigid blade laryngoscopes.3 Compared with direct laryngoscopy, the use of videolaryngoscopy in nasotracheal intubation bring about good outcomes, such as increased glottic visualization and efficiency for both normal and difficult airways.4-6 Studies have shown no significant differences in nasal bleeding for McGrath, GlideScope, and Pentax airway scopes compared with Macintosh laryngoscopes.2,4,7 However, neither video stylet laryngoscopes nor intubation stylets have been used in those studies. The FKScope® comprises a semirigid, malleable stylet with a terminal camera (Figure 1), and it has been used to facilitate orotracheal intubation in Taiwan. However, its efficacy and safety for nasotracheal intubation remain unknown. This study compared FKScope® direct laryngoscopy with Macintosh one for nasotracheal intubation.

Download full-size image
Methods
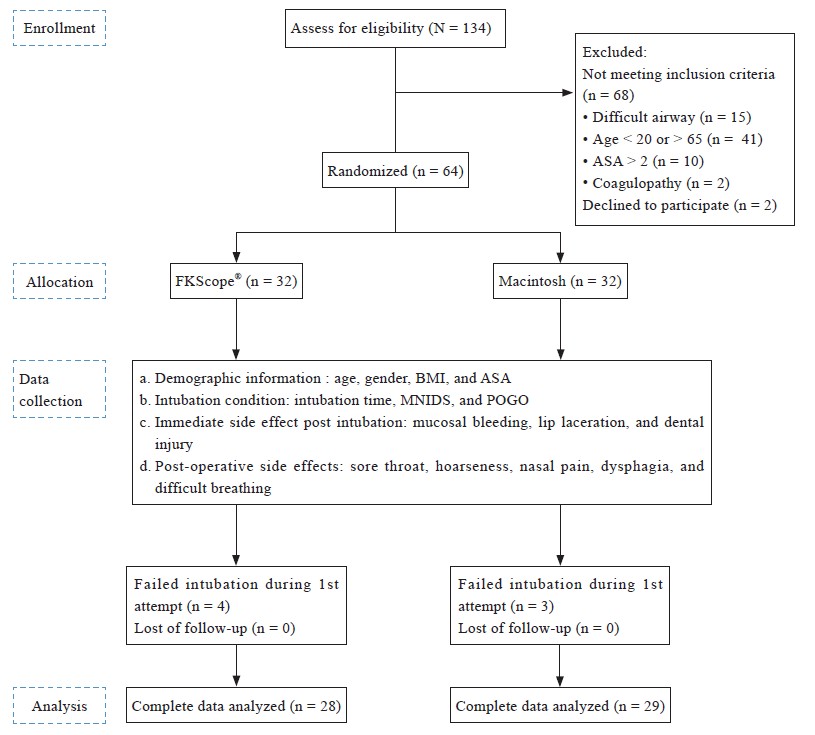
The overall structure of our study is summarized in the CONSORT flow diagram in Figure 2. We enrolled patients who were 20–65 years old, classified as American Society of Anesthesiologists (ASA) 1–2, and were scheduled to undergo elective oral and maxillofacial surgery under general anesthesia with nasotracheal intubation. Exclusion criteria were a suspected difficult airway, such as limited mouth opening (< 2 fingerbreadths); oropharyngeal anomaly and limited cervical spine motion; and contraindications for nasotracheal intubation such as recent nasal surgery, midface instability, basilar skull fracture, and coagulopathy. All nasotracheal intubations were performed only for surgical need. High-risk patients who had contraindications for nasotracheal intubation were excluded during the screening period. Any untoward or adverse event was treated in time and documented. The studied device, FKScope®, is FDA approved and has been used to help orotracheal intubation in several countries. Possible side effects and complications of nasotracheal intubation and further management strategies were explained thoroughly to all patients. Participants were randomized into two groups: FKScope ® and Macintosh direct laryngoscope, each of size 32. Randomization was performed using an online calculator (https://www.graphpad.com/quickcalcs/randomize1.cfm). Written informed consent was obtained from all participants.
Download full-size image
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index; MNIDS, modified nasal intubation difficulty score; POGO, percentage of glottic opening.
No participant received any premedication. Each patient was fitted with a standard monitor in the operation room before induction of anesthesia. Baseline hemodynamic data recorded included heart rate, blood pressure (noninvasive), and oxygen saturation (SpO2). General anesthesia was induced with intravenous fentanyl (1.5–2.0 μg/kg), propofol (2.0–2.5 mg/kg), and either rocuronium (1.00 mg/kg) or cisatracurium (0.02 mg/kg). Mask ventilation using 100% oxygen was provided to all patients; while it was being performed, both groups received Lignospan® (lidocaine 2% with epinephrine 1:100,000) nasal packing. Because we used simple preinduction clinical tests based on airflow to estimate the relative patency of the nostrils may not be helpful,8 we tested each nostril by using cotton swab infiltrated with Lignospan® during nasal packing. Patients were intubated by one of the three anesthesiologists who were also researchers in this study; each of them had clinical experience of more than 3 years and had previously performed at least 10 successful intubations by using both devices. The sizes of endotracheal tube that we used were 7.0 mm (inner diameter) for male patients and 6.5 mm for female patients. In the FKScope® group, the endotracheal tube was loaded onto the video stylet.
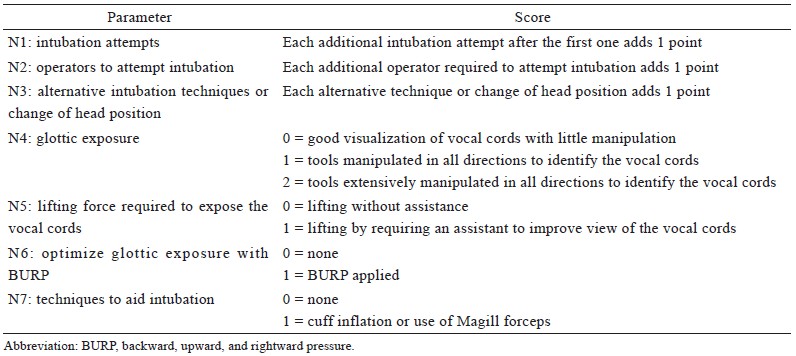
The primary outcome was time to successful intubation during the first attempt. Intubation time was defined as the time from face mask removal from a patient’s face to the appearance of three consecutive capnography waveforms. Intubation failure was defined as either an intubation time exceeding 150 seconds or SpO2 decreasing below 95%,4 in which case a different intubation method was performed. The rate of successful first intubation was calculated for each group; patients who were successfully intubated on the first attempt were retained for further analysis. Secondary outcomes included the percentage of glottic opening (POGO); modified nasal intubation difficulty scale (MNIDS) score (Table 1);9-11 immediate side effects including mucosal bleeding, lip laceration, and dental injury; and postoperative side effects including sore throat, hoarseness, nasal pain, dysphagia, and difficulty breathing. MNIDS scores were categorized as easy (0), minor difficulty (0–5) and major difficulty (> 5). The oral and nasal cavities were aspirated using a suction catheter to evaluate mucosal bleeding. After surgery, patients were asked about sore throat, hoarseness, nasal pain, dysphagia, and difficulty breathing in the postanesthesia care unit (PACU) by using a questionnaire.
Download full-size image
Sample-Size Calculation and Statistical Analysis
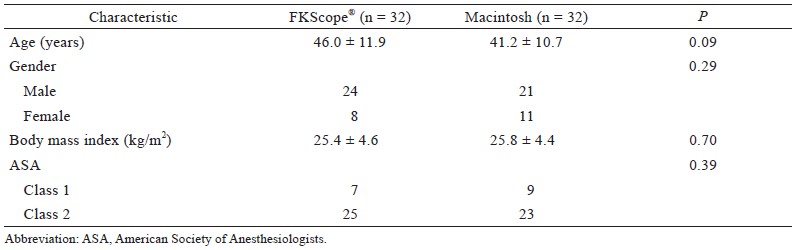
According to the criteria of Sim and Lewis12 for determining a pilot study’s sample size, an appropriate pilot size is likely to be at least n = 55; furthermore, considering a 10% dropout rate, at least 61 patients should be enrolled. We planned to enroll 64 patients. Data analysis was performed using SPSS version 20.0 (IBM, Armonk, NY, USA). The baseline data of the participants are presented as means and standard deviations (SDs) (Table 2). Categorical data were analyzed using either a chi-square test or Fisher’s exact test as appropriate. Continuous data were compared using independent-sample t tests. All tests were two-sided and performed at the 0.05 level of significance.
Download full-size image
Results
The data of 64 patients were analyzed, each treatment group has 32 patients , and no significant differences between groups were found (Table 2). In the FKScope® group, failed intubation was recorded in 4 patients. Among these intubation failures, 3 of 4 patients was due to nasopharyngeal bleeding that obstructed the camera, and 1 of them was due to a narrow nostril. Successful second-attempt intubations were performed with a Macintosh laryngoscope for 1 patient and GlideScope for 2 patients with nasopharyngeal bleeding. For the patient with a narrow nostril, the other nostril was intubated with a Macintosh laryngoscope. In the Macintosh laryngoscope group, 3 failed intubations were reported, 2 of them failed because of a high anterior larynx; and was successfully intubated during the second attempt by using a GlideScope. The other failed intubation was due to retropharyngeal laceration during the first intubation, and intubation through the other nostril during the secondary attempt was successful. The rates of successful first-attempt intubation were 87.5% (28/32) and 90.6% (29/32) in the FKScope® and Macintosh groups, respectively (P = 0.69). The mean (± SD) total intubation time was 68.7 ± 34.8 s in the FKScope® group and 61.5 ± 21.9 s in the Macintosh group (P = 0.35; Table 3), despite a higher POGO in the FKScope ® group (Table 3; FKScope®, 77 ± 27; Macintosh, 41 ± 31; P < 0.01). Mean MNIDS scores were also significantly lower in the FKScope® group (FKScope®, 0.8 ± 1.0; Macintosh, 2.8 ± 1.4; P < 0.01). No significant differences were observed in postoperative side effects, including sore throat, hoarseness, nasal pain, dysphagia, and dyspnea as assessed by reviewing the patient questionnaires in the PACU (Figure 3). However, postintubation lip lacerations were significantly less common in the FKScope® group. (Table 3, P = 0.04).
Download full-size image
Download full-size image
Discussion
In this study, we examined the efficacy and safety of the FKScope® for nasotracheal intubation. To test the efficacy, we compared intubation time of using FKScope® laryngoscopy with intubation time of using Macintosh laryngoscopy, which is a conventional method of nasotracheal intubation. Our results indicate that using FKScope® required more time than Macintosh laryngoscopy for intubation in normal airways although the difference was not significant, and this result contradicts most previous studies.4-7 However, videolaryngoscopes with a rigid blade (e.g., GlideScope, Artrap, or McGrath) instead of a video stylet were used in those studies. The use of videolaryngoscopes with a video stylet for nasotracheal intubation has been studied previously. Lee et al.9 concluded that the Trachway technique for nasotracheal intubation is quicker and easier compared with fiberoptic intubation in patients with restricted mouth opening, but the data were limited when compared with those of Macintosh laryngoscopy. In the present study, one possible reason for the longer intubation time in the FKScope® group was the increased amount of time required for the video stylet to advance the nasopharynx. We passed the endotracheal tube along with the FKScope® through the nasal cavity carefully under direct vision to avoid injuring the turbinate and to minimize damage to the nasopharyngeal mucosa, but the mucosal bleeding rate did not differ significantly between the two groups. More failed intubations occurred with the FKScope® than with the Macintosh laryngoscope mostly because of nasopharyngeal bleeding despite nasal preparation with topical vasoconstrictors. Mucosal bleeding obscures the view of the FKScope®. Epistaxis from the nasal mucosa is the most frequent complication of nasotracheal intubation, with an incidence of 18%–77%.13-15 Oropharyngeal blood or secretions rarely obstruct the laryngeal view during direct laryngoscopy unless massive bleeding occurs, whereas a single drop of blood or a secretion smear on the camera lens of a videolaryngoscope may completely obscure the view.16 Therefore, patient selection is an important consideration when using the FKScope® as a nasotracheal intubation tool. In addition, previous findings have demonstrated that the use of videolaryngoscopy improved glottic views for nasotracheal intubation2,5,6,7. These previous findings are compatible with our result, as we found significantly higher POGOs in the FKScope® group. The video stylet improves visualization of the vocal cords without requiring the alignment of the oral, pharyngeal, and laryngeal axes. Compared with Macintosh laryngoscopy, the use of FKScope® might overcome the challenges of large tongue, anterior larynx, and floppy epiglottis. In addition, we found one retropharyngeal laceration—a complication that has rarely been reported in nasotracheal intubation17,18—in the Macintosh group. In this group, advancement of the nasotracheal tube into the nasopharyngeal space was performed blindly, making direct observation of the direction of the tube during this stage difficult. By contrast, the FKScope® contains a camera at the end of the stylet, which can help guide a stylet-loaded endotracheal tube into the nasopharynx under direct observation.
We used the MNIDS to assess the intubation difficulty and its predictive factors. A total score of 0 indicated intubation under ideal conditions with no difficulty. A total score of 1–5 indicated minor difficulty, and an MNIDS score higher than 5 indicated major difficulty. Fourteen patients in the FKScope® group were categorized as having no difficulty, whereas none in the Macintosh group were categorized as such, resulting in a significantly lower mean MNIDS score for the FKScope® group. Several previous studies have reported greater ease of intubation with videolaryngoscopy by using different assessment methods.5,19-22 Furthermore, most nasal intubations in the Macintosh group were assisted by Magill forceps, which were often used to facilitate intubation in the case of misalignment. However, sore throat is a common complication of nasotracheal intubation resulting from direct pharyngeal trauma caused by Magill forceps.23 Moreover, the use of Magill forceps is not always available when intubation is difficult. Direct laryngoscopy is performed to visualize the vocal cords through the originally curved oral airway space by aligning the oral, pharyngeal, and laryngeal axes in the head’s sniffing position. Although we excluded patients who had possibly difficult airways, a higher Cormack grade could cause unanticipated difficulties in laryngoscopy, in which case the BURP (backward, upward, and rightward pressure) maneuver might be applied to optimize glottic exposure. These reasons might explain why the MNIDS score was higher in the Macintosh group.
The incidence of anesthesia-related dental damage varies widely in the literature.24,25 Dental injury during the perianesthesic period was recorded in 132 cases (1:4537), and half of these injuries occurred during laryngoscopy and tracheal intubation.25 By contrast, a prospective study of 536 patients who underwent direct laryngoscopy for intubation reported a much higher rate (25%) of dental injury.26 However, comparisons between video stylet and direct laryngoscopy concerning dental injury have been limited. In the present study, the incidences of dental injury were 0/28 and 1/29 in the FKScope® and Macintosh groups, respectively. The lack of a significant difference between the groups was probably because of the small sample size. With respect to other types of injury, 4 lip lacerations were recorded in the Macintosh group, and none was recorded in the FKScope® group. A prospective observational study that enrolled 534 patients undergoing general surgery requiring tracheal intubation through classic direct laryngoscopy showed that soft tissue trauma after intubation was observed in 278 (52.1%) patients.27 Tongue injury was the most common type of soft tissue trauma (36.3%), followed by injury to the lower lip (22.3%), upper lip (7.1%), and oral mucosa (2.1%). However, these previous studies have not compared tissue injury between videolaryngoscopy and direct laryngoscopy. In our study, the difference in tissue injuries was significant between the two groups.
The FKScope® is a videolaryngoscope that uses a video stylet. Similar devices include the Trachway intubating stylet (Biotronic Instrument Enterprise Ltd., Taichung, Taiwan) and the VideoStylet (MEDLUME CO. LTD., Taipei, Taiwan). Video stylet-type devices, which have been widely used for tracheal intubation,28-30 contain a rigid or semirigid stylet with a terminal camera; therefore, cephalad movement of the video stylet handle might exert compressive force on the nasal crura. Hence, the manipulation of a stylet tube within the nasal cavity might cause iatrogenic injury during nasal intubation. Although safety issues regarding nasal trauma are another concern, the FKScope® did not cause more mucosal bleeding episodes than the Macintosh laryngoscope did in our study. Moreover, we used a questionnaire to evaluate patients’ postoperative complications, including nasal pain, sore throat, hoarseness, dysphagia, and dyspnea, and found no significant differences between the two groups. Thus, our results indicate that the FKScope® is safe for use in nasotracheal intubation.
The utilization of appropriate tools for intubation can improve the management of difficult airways. In patients with an anticipated difficult airway, videolaryngoscopy significantly improved laryngeal exposure, thus facilitating endotracheal intubation.31 Based on our findings, we would select a videolaryngoscope over a Macintosh laryngoscope as an intubation tool for anticipated difficult airways in clinical practice to ensure the safety of our patients. Furthermore, limited mouth opening is a characteristic of the airway that is difficult for direct laryngoscopy. By contrast, the FKScope ®, which lacks a blade, might be useful for intubation in such patients. Therefore, only patients with normal airways were enrolled in this study to avoid allocation bias. Further studies that include patients with anticipated difficult airway are required to test the role of the FKScope® in nasotracheal intubation.
Our study has several limitations. First, the sample size was small. Second, the anesthesiologists were not blinded to the study groups. Third, we did not perform more objective airway assessments (e.g., Mallampati score or thyromental distance) to exclude patients with difficult airways. Fourth, although three of the anesthesiologists have extensive experience with nasotracheal intubation, personal differences in technique might have caused some bias.
In conclusion, FKScope® provides a better view of the glottic opening than Macintosh direct laryngoscopy does and is used easily and safely for nasotracheal intubation for normal airways. However, secretions and blood may obscure the camera view. Therefore, patient selection must be considered carefully when using the FKScope®.
References
| 1 |
Healy DW, Maties O, Hovord D, Kheterpal S.
A systematic
review of the role of videolaryngoscopy in successful
orotracheal intubation.
BMC Anesthesiol. 2012;12:32.
|
| 2 |
Prasanna D, Bhat S.
Nasotracheal intubation: an overview.
J Maxillofac Oral Surg. 2014;13(4):366-372.
|
| 3 |
Kwak HJ, Lee SY, Lee SY, Cho SH, Kim HS, Kim JY.
Mc-Grath video laryngoscopy facilitates routine nasotracheal intubation in patients undergoing oral and maxillofacial surgery: a comparison with Macintosh laryngoscopy.
J Oral Maxillofac Surg. 2016;74(2):256-261.
|
| 4 |
Tseng KY, Lu IC, Shen YC, Lin CH, Chen PN, Cheng KI.
A comparison of the video laryngoscopes with Macintosh laryngoscope for nasotracheal intubation.
Asian J of Anesthesiol.
2017;55(1):17-21.
|
| 5 |
St Mont G, Biesler I, Pförtner R, Mohr C, Groeben H.
Easy and difficult nasal intubation—a randomised comparison of Macintosh vs Airtraq® laryngoscopes.
Anaesthesia. 2012;67(2):132-138.
|
| 6 |
Chae YJ, Kim DH, Park EJ, Oh J, Yi IK.
A comparison
of McGrath MAC, Pentax AWS, and Macintosh direct
laryngoscopes for nasotracheal intubation: a randomized
controlled trial.
Ther Clin Risk Manag. 2019;15:1121-
1128.
|
| 7 |
Kang R, Jeong JS, Ko JS, et al.
Neutral position facilitates
nasotracheal intubation with a glideScope video
laryngoscope: a randomized controlled trial.
J Clin Med.
2020;9(3):671.
|
| 8 |
Smith JE, Reid AP.
Identifying the more patent nostril
before nasotracheal intubation.
Anaesthesia.
2001;56(3):258-262.
|
| 9 |
Lee MC, Tseng KY, Shen YC, et al.
Nasotracheal intubation
in patients with limited mouth opening: a comparison
between fibreoptic intubation and the Trachway®.
Anaesthesia. 2016;71(1): 31-38.
|
| 10 |
Ovassapian A, Yelich SJ, Dykes MH, Brunner EE.
Fiberoptic
nasotracheal intubation—incidence and causes of
failure.
Anesth Analg. 1983;62(7):692-695.
|
| 11 |
Ono K, Goto T, Nakai D, Ueki S, Takenaka S, Moriya T.
Incidence and predictors of difficult nasotracheal intubation
with airway scope.
J Anesth. 2014;28(5):650-654.
|
| 12 |
Sim J, Lewis M.
The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency.
J Clin Epidemiol. 2012;65(3):301-
308.
|
| 13 |
Elwood T, Stillions DM, Woo DW, Bradford HM, Ramamoorthy C.
Nasotracheal Intubation: a randomized
trial of two methods.
Anesthesiology. 2002;96(1):51-53.
|
| 14 |
Hall CEJ, Shutt LE.
Nasotracheal intubation for head
and neck surgery.
Anaesthesia. 2003;58(3):249-256.
|
| 15 |
Enk D, Palmes AM, Aken HV, Westphal M.
Nasotracheal
intubation: a simple and effective technique to reduce
nasopharyngeal trauma and tube contamination.
Anesth
Analg. 2002;95(5):1432-1436.
|
| 16 |
Rothfield KP, Russo SG.
Videolaryngoscopy: should
it replace direct laryngoscopy? a pro-con debate.
J
Clin Anesth. 2012;24(7):593-597.
|
| 17 |
Krebs MJ, Sakai T.
Retropharyngeal dissection during
nasotracheal intubation: a rare complication and its management.
J Clin Anesth. 2008;20(3):218-221.
|
| 18 |
Tintinalli JE, Claffey J.
Complications of nasotracheal
intubation.
Ann Emerg Med. 1981;10(3):142-144.
|
| 19 |
Puchner W, Drabauer L, Kern K, et al.
Indirect versus
direct laryngoscopy for routine nasotracheal intubation.
J Clin Anesth. 2011;23(4):280-285.
|
| 20 |
Jones PM, Armstrong KP, Armstrong PM, et al.
A comparison
of glidescope videolaryngoscopy to direct laryngoscopy
for nasotracheal intubation.
Anaesthesia. 2010;65(6):569-572.
|
| 21 |
Lili X, Zhiyong H, Jianjun S.
A comparison of the Glide-
Scope with the Macintosh laryngoscope for nasotracheal
intubation in patients with ankylosing spondylitis.
J
Neurosurg Anesthesiol. 2014;26(1):27-31.
|
| 22 |
Suzuki A, Onodera Y, Mitamura SM, et al.
Comparison
of the Pentax-AWS airway scope with the Macintosh
laryngoscope for nasotracheal intubation: a randomized,
prospective study.
J Clin Anesth. 2012;24(7):561-565.
|
| 23 |
Yeom JH, Oh MK, Shin WJ, Ahn DW, Jeon WJ, Cho SY.
Randomized comparison of the effectiveness of nasal
intubation using a GlideScope video laryngoscope with
Magill forceps versus vascular forceps in patients with a
normal airway.
Can J Anaesth. 2017;64(12):1176-1181.
|
| 24 |
Warner ME, Benenfeld SM, Warner MA, Schroeder
DR, Maxson PM.
Perianesthetic dental injuries: frequency,
outcomes, and risk factors.
Anesthesiology.
1999;90(5):1302-1305.
|
| 25 |
Mourão J, Neto J, Luís C, et al.
Dental injury after conventional
direct laryngoscopy: a prospective observational
study.
Anaesthesia. 2013;68(10):1059-1065.
|
| 26 |
Mourão J, Moreira J, Barbosa J, Carvalho J, Tavares J.
Soft
tissue injuries after direct laryngoscopy.
J clin Anesth.
2015;27(8):668-671.
|
| 27 |
Hsu HT, Lin CH, Tseng KY, et al.
Trachway in assistance
of nasotracheal intubation with a preformed nasotracheal
tube in patients undergoing oral maxillofacial surgery.
Br
J Anaesth. 2014;113(4):720-721.
|
| 28 |
Yang M, Kim JA, Ahn HJ, Choi JW, Kim DK, Cho EA.
Double-lumen tube tracheal intubation using a rigid video-
stylet: a randomized controlled comparison with the
Macintosh laryngoscope.
Br J Anaesth. 2013;111(6):990-
995.
|
| 29 |
Tseng KY, Chau SW, Su MP, Shih CK, Lu IC, Cheng KI.
A comparison of Trachway intubating stylet and Airway
Scope for tracheal intubation by novice operators: a manikin
study.
Kaohsiung J Med Sci. 2012;28(8);448-451.
|
| 30 |
Chang PY, Hu PY, Lin YC, et al.
Trachway video intubating
stylet allows for optimization of electromyographic
endotracheal tube placement for monitored thyroidectomy.
Gland Surg. 2017;6(5):464-468.
|
| 31 |
Stroumpoulis K, Pagoulatou A, Violari M, et al.
Videolaryngoscopy
in the management of the difficult airway: a
comparison with the Macintosh blade.
Eur J Anaesthesiol.
200926(3):218-222.
|