Abstract
Background
Laparoscopic cholecystectomy is a commonly performed surgical procedure. Most anesthesiologists advocate tracheal intubation. Laparoscopic cholecystectomy is becoming a day care surgery, hence many anaesthesiologists have started using laryngeal masks to decrease airway manipulation seen with conventional laryngoscopy and endotracheal intubation and avoid hemodynamic pressor responses and postoperative sore throat. The Supreme laryngeal mask airway (LMA) is an innovative, sterile, single use, supraglottic airway management device which provides access to and functional separation of the respiratory and digestive tracts. In this study, there are two objectives—(1) primary objective: to assess the adequacy of ventilation when using LMA-SupremeTM (LMA-S) and endotracheal tube (ETT), and (2) secondary objective: the first is to give the time for achieving effective airway and number of attempts for securing airway. The second is to assess haemodynamic parameters (heart rate and blood pressure). The last is to show the incidence of gastric distension, regurgitation and postoperative sore throat.
Methods
A total of 132 American Society of Anesthesiologists (ASA) I–II patients were randomly assigned to LMA-S and ETT for intraoperative ventilation. After induction of general anaesthesia, the device was inserted, correct placement was checked, and parameters were recorded. SPSS version 20.0 software (IBM Corp., Armonk, NY, USA) was used for statistical analysis. A
Results
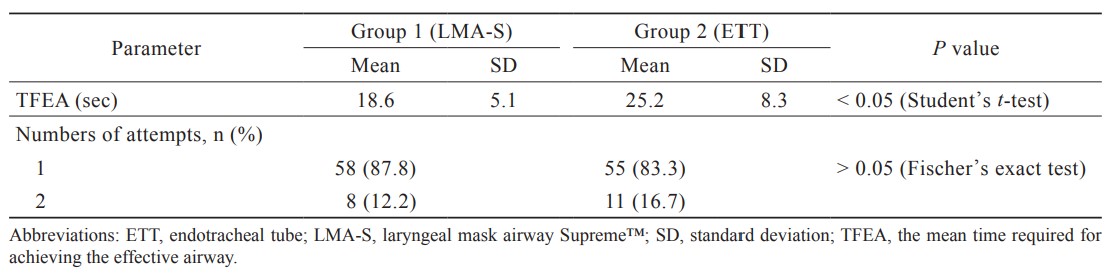
Ventilatory parameters such as inspiratory and expiratory leak volumes, and peak airway pressure values were comparable between the groups throughout the entire time interval. The number of attempts for successful insertion were comparable, but the mean time required for achieving effective airway was significantly longer in ETT than LMA-S (25.2 ± 8.3 sec vs. 18.6 ± 5.1 sec, respectively [
Conclusions
Positive pressure ventilation with a correctly placed LMA-S allows adequate pulmonary ventilation, without the untoward hemodynamic and postoperative adverse effects of endotracheal intubation, in laparoscopic cholecystectomy surgery.
Keywords
anesthesia, endotracheal tube, laparoscopic cholecystectomy, laryngeal mask airway Supreme
Introduction
After the laryngeal mask was evaluated in laparoscopic cholecystectomy for the first time in 1996, very few clinical studies have been done on the topic.1-4
The advantages of laryngeal mask airway (LMA) are the avoidance of complications associated with tracheal intubation, and the ease and quickness of placement of the airway device itself, which leads to a reduced requirement for neuromuscular blockade and a lower incidence of postoperative sore throat, dysphonia, and dysphagia.5,6 However, there are also some disadvantages such as pulmonary aspiration of gastric contents, the inability to provide accurate ventilation during laparoscopy in the context of increased intra-abdominal pressure (IAP), and high peak airway pressure (PAP).7
One of the most widely studied supraglottic airway devices is the classical LMA (LMA-C), and in recent years, ProsealTM (LMA-P), LMA SupremeTM (LMA-S), i-gelTM, and the Guardian CPVTM have been put into practice. With constant improvements, these devices could be reasonably safe in the use of laparoscopy, but many anesthesiologists remain unconvinced about the supraglottic airway in these procedures. This forms the basis of this study.
This study aims to compare LMA-S and endotracheal tube (ETT) in healthy adult patients undergoing laparoscopic cholecystectomy under general anesthesia. The objectives in the study are listed as follows:
(1) Primary: To assess the adequacy of ventilation when using LMA-S or ETT by measuring:
• Quality of glottic airway seal—difference between inspired tidal volume and expired tidal volume
• Oxygen saturation (SpO2)
• End tidal carbon dioxide (EtCO2)
• PAP
(2) Secondary:
• Ease of insertion: Time required for achieving effective airway and the number of attempts for securing airway
• Hemodynamic responses (heart rate, systolic, diastolic, and mean arterial blood pressure) was recorded before induction, at the time of insertion, 1 and 5 minutes after insertion of device, on pneumoperitoneum inflation and deflation, and on extubation.
• Complications: Incidences of gastric distension, aspiration, and postoperative sore throat were noted.
Methods
Ethics committee approval (889-14-SN) was obtained (P.D. Hinduja National Hospital & M.R.C., India), and trial was registered with CTRI number CTRI/2017/11/010452.
Study Population
(1) Sample size: 132 patients.
(2) Inclusion criteria: 132 American Society of Anesthesiologists (ASA) status I and II adults of either sex, aged 20–65 years, weighted 40–80 kg, scheduled for elective laparoscopic cholecystectomy, under general anesthesia, who had given consent to participate was recruited.
(3) Exclusion criteria:
• Obesity (body mass index [BMI] > 30 kg/m2)
• Increased risk of aspiration (e.g., gastro-esophageal reflux disease, hiatus hernia, and pregnant patients)
Patients with anticipated difficult airway (e.g., reduced mouth opening, oropharyngeal pathology, and restricted neck mobility).
Study Design
The study is prospective, randomized, doubleblind, and comparative.
Time Frame
The period is from March 15 to June 16.
Study Intervention
Interventions were done by qualified anesthesiologists. Informed consent was obtained. Patients were randomized by opening an opaque envelope inside the operation theatre containing the computer-generated random assignment into two groups (group 1: LMA-S and group 2: endotracheal intubation). After insertion of the device, the face of the patient (including the device) was covered by a sheet of cloth. The principal investigator monitored the readings.
Anesthesia
Standard anesthetic procedures were followed, monitors were attached, and baseline parameters were noted. Premedication with intravenous midazolam 1 mg (5 minutes prior to induction) and fentanyl citrate (1 µg/kg) was given. After 3 minutes preoxygenation, anesthesia was induced with propofol 2 mg/kg. Intravenous atracurium 0.5 mg/kg was given, and after paralysis, the airway was inserted. In group 1, LMA-S (size 3 for weight 30–50 kg, size 4 for weight 50–70 kg, and size 5 for weight 70–100 kg) was used. In group 2, endotracheal intubation (7 mm internal diameter in females and 8 mm internal diameter in males) was performed. The cuffs of both devices were inflated with air by using the aneroid manometer to an intracuff pressure of 60 cm H2O (LMA-S) and 25 cm of H2O (ETT) and maintained at that value throughout the procedure.
Time for achieving effective airway was defined as the time from the picking-up of the airway device to the correct placement of it, which was seen with one effective end-tidal capnography waveform.
(1) Correct placement of the devices was confirmed by:
• Adequate chest movement on manual ventilation
• Square wave capnography
• Expired tidal volume of more than 6 mL/kg
• For LMA-S, no audible leak from the drain tube with PAP less than 20 cm H2O. A leak below 20 cm H2O was regarded as significant and suggested a malposition.
(2) Criteria for crossover between study groups:
• Failure to place the airway device with three
attempts
• Respiratory obstruction
• Persistent audible oropharyngeal leak
• Insufficient ventilation (EtCO2 > 40 mmHg
before insufflation)
• Gastric distension interfering with surgical field
• Maximum expired tidal volume < 6 mL/kg
After the placement of the device, a number 14 gastric tube was inserted. Anesthesia was maintained with air, oxygen (FiO2 0.5), and sevoflurane (MAC 1) on the volume control ventilation mode at 6–8 mL/kg tidal volume, with no positive end-expiratory pressure. Respiratory rate was maintained to keep ETCO2 from 25 to 35 mmHg. Additional fentanyl (up to 2 mcg/kg) and atracurium boluses (0.5 mg) were given as and when required. IAP was maintained at 11–15 mmHg.
Standard 0.05 mg/kg of neostigmine and 0.6 mg of atropine was used for reversal. The airway device was removed when the patient was awake, breathing spontaneously, and responding to verbal commands.
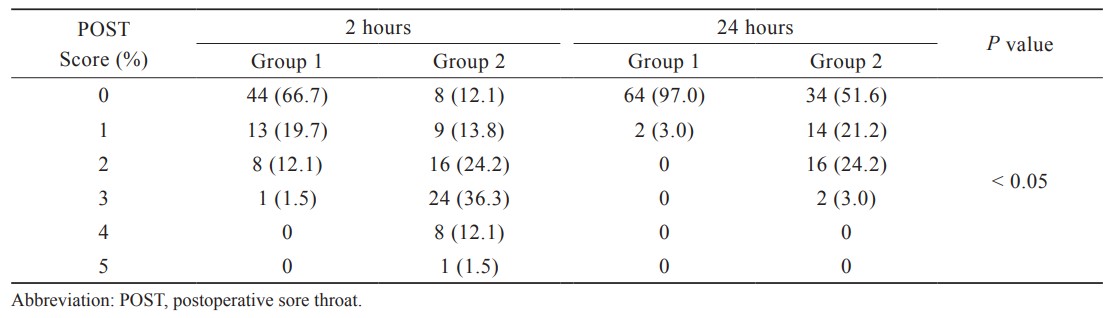
Postoperative sore throat was graded by the patient from 0 to 5 after 2 hours in the recovery room and again after 24 hours.
Study Duration
This study was conducted in the operating room, and the patients were followed up for 24 hours to check the degree of sore throat.
Sample Size
Sample size was calculated with the help of difference in mean method based on the article by Kahla and Alhusainy8—“Tidal volume expired pre-carboperitoneum” at 90% confidence interval (α error) and at 80% power of study.
As per their study, LMA-S had standard deviation (SD) of 65.7(σ1), and ETT had SD of 49.3(σ2)
Formula:
N1 = 65; N2 = 65; N ≈ 132; σ1, σ2 = SD; μ1, μ2 = mean; Z1–α/2 = 1.645; Z1–β = 0.842. Based on these conditions, the sample size was 132, which is 66 in each group.
After data collection, data entry was done in MS Excel 2010. Data analysis was done with the help of SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA). Quantitative data were presented with the help of mean and SD. Comparison was done with unpaired
Results
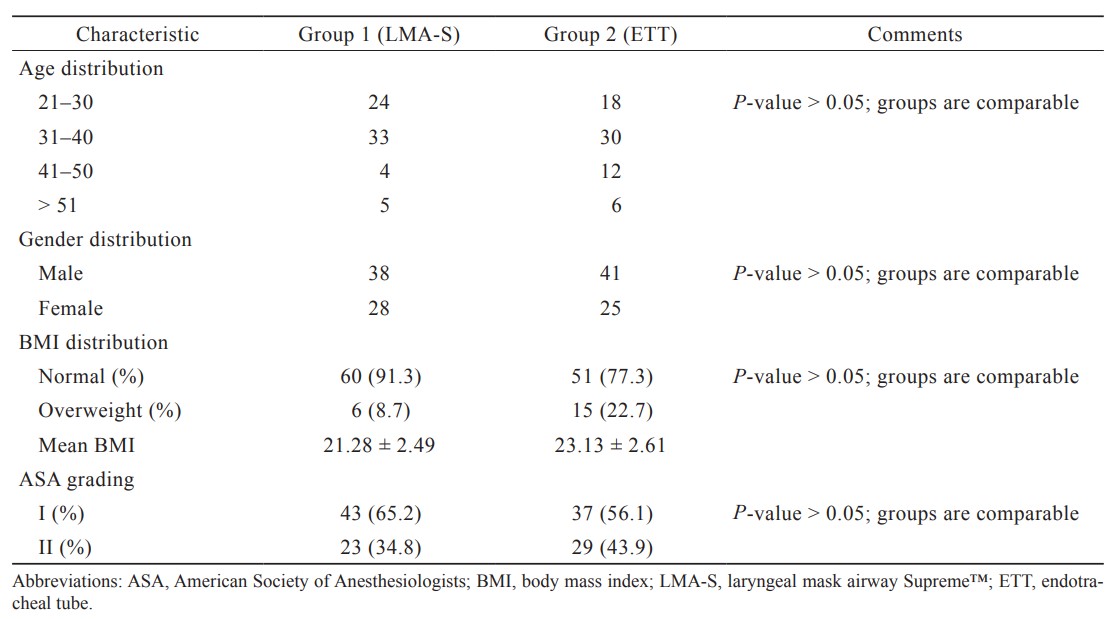
The mean age in the groups were 35.14 ± 9.35 (group 1) and 36.37 ± 10.97 (group 2), as shown in Table 1. The gender distribution, BMI, and the ASA grades distribution were also comparable and statistically not significant (
Download full-size image
As shown in Table 2, the mean time required for achieving the effective airway (TFEA) with the LMA-S was significantly lesser than that with the ETT. This is a very important finding of this study. However, when the number of attempts to insert the device was taken into account, there is not statistically significant difference.
The SpO2 of the two groups was compared, and there was no statistically significant difference between the two groups during the entire observed period.
Download full-size image
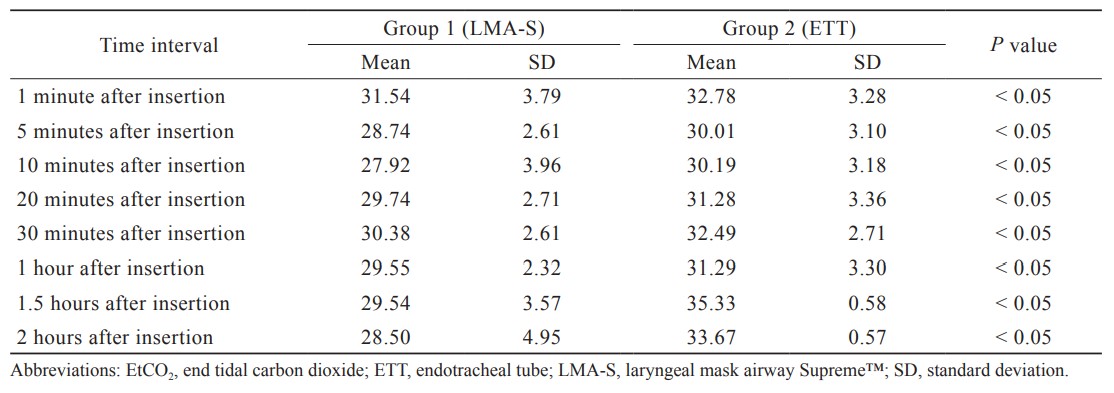
Table 3 shows the comparison of EtCO2 (mmHg) between groups. At all the time points, EtCO2 values were significantly lower in group LMA-S than group ETT.
Download full-size image
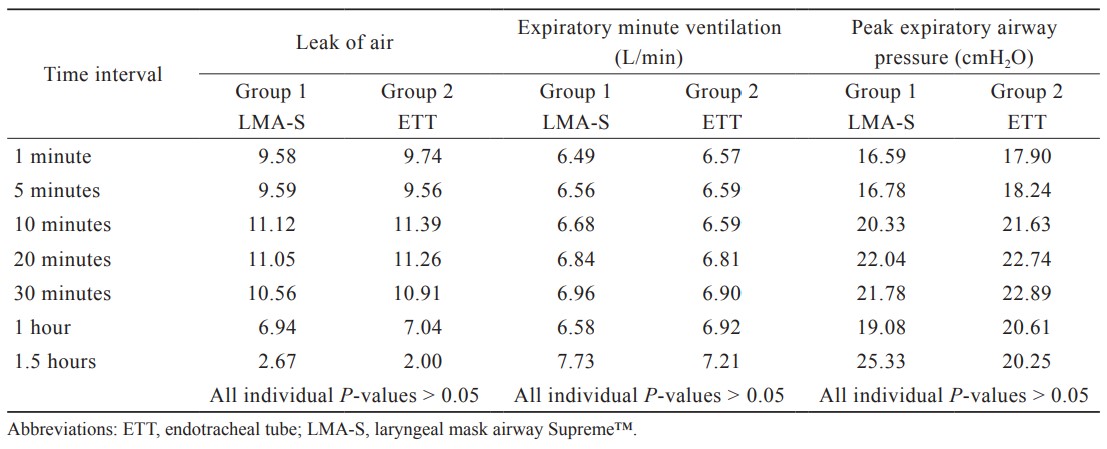
The leak of air between inspiratory tidal volume and the expiratory tidal volume, the expired minute ventilation and the peak expiratory airway pressure for each device were compared between the groups and the results are presented in Table 4, and there was no significant difference between the groups at all the time points.
Download full-size image
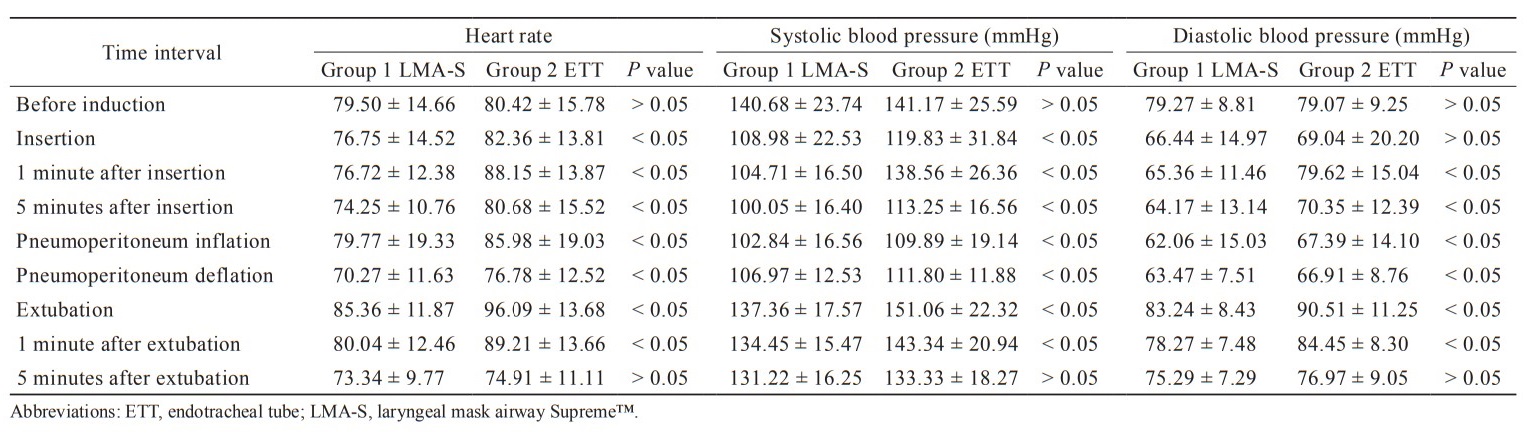
In Table 5, heart rate is significantly lower in group LMA-S for the entire time intervals starting from the time of insertion to 1 minute after extubation than group ETT.
Download full-size image
Systolic blood pressure (SBP) (mmHg) is significantly lower in group LMA-S for the entire time intervals from the time of insertion to 1 minute after extubation than group ETT. Diastolic blood pressure (DBP) (mmHg) is significantly lower in group LMA-S for the entire time intervals from 1 minute after insertion to 1 minute after extubation than group ETT.
There was no significant difference in the IAP between the groups. It was observed that there were no cases of gastric distension or regurgitation in both groups.
In Table 6, the postoperative sore throat scoring at 2-hour and 24-hour interval was significantly lower in group LMA-S than group ETT.
Download full-size image
Discussion
As shown in the results, the demographic parameters (age, gender, BMI, and ASA grading) were comparable between both groups. Maltby et al.9 and Natalini et al.10 have compared LMA and ETT in obese patients. In our study, there were no obese patients but only few overweight patients
Ease of Insertion
In our study, there was no failure of securing the airway. Both 12% of the LMA-S group and 17% of the ETT group needed the second attempt at securing the airway. Patel et al.11 and Saraswat et al.12 had succeeded in the first attempt in all their patients. In another study conducted by Anand et al.,13 LMA-S demonstrated a very good success rate at the first insertion.
In the study conducted by Beleña et al.,2 there was also a very high success rate of the first insertion (96 %). Additionally, in the study conducted by Yao et al.,14 airway insertion was performed on caesarean section patients, and the success rates of LMA and the ETT groups were comparable.
Pournajafian et al.15 showed a success rate of 80.6% which was quite similar to the 88% in our study. However, Kahla and Alhusainy8 had identified much lower success rate as 48%. The overall acquired results of success rate was 88%, correlating well with the findings of 86%–100% in the review article written by Wong et al.16
The mean TFEA was shorter with the LMA-S, which is similar to the results in the studies done by Kahla and Alhusainy8 and Jarineshin et al.17 However, Wong et al.16 stated that the “time for insertion” lacked an accurate definition.
Adequacy of Ventilation
At all the time intervals, SpO2 was adequate, and the mean EtCO2 was maintained between 25–35 mmHg, and values were significantly lower in group LMA-S than group ETT for the entire time intervals from 1 minute after insertion to 2 hours after insertion but were not clinically significant. Beleña et al.2 also reported similar adequacy of ventilation parameters in patients undergoing elective laparoscopic cholecystectomy.
Ventilatory parameters (Table 4) were similar in both groups. There was no problem in maintaining the ventilatory parameters during the entire period of the operative procedure. This is similar to the findings noted in the studies conducted by Kahla and Alhusainy8 and Barreira et al18. In summary, the LMA-S provides effective ventilation and lasts throughout the procedure.
Hemodynamic Parameters
Between the two groups, heart rate, SBP, DBP, and mean arterial pressure were significantly lower in group LMA-S than group ETT for all the time intervals from 1 minute after insertion to 1 minute after extubation (Table 5). The changes of the cardiovascular responses in our study correlated to the studies of Kahla and Alhusainy,8 Jarineshin et al.,17 Barreira et al.,18 and Singam et al.19 Shribman et al.20 concluded that stimulation of the supraglottic region by laryngoscopy and intubation is the major cause of the increased release of catecholamines that may be concerned about patients with high cardiac risk.
Complications
There was no gastric distension in both groups on enquiry with the surgeons, and these findings were similar to the report of Kahla and Alhusainy.8 There were no cases of regurgitation noted in our study, which was similar to the studies conducted by Yao et al.,14 Anand et al.,13 and Saraswat et al.12
There were no cases of pulmonary aspiration in our study. This is consistent with the findings of Bernardini and Natalini,21 Beleña et al.,5 and Barreira et al.18 The occurrence of postoperative sore throat was less in the LMA-S group. This is similar to the results of the studies conducted by Beleña et al.,5 Singam et al.,19 and Pournajafian et al.,15 but unlike those by Yao et al.14 and by Anand et al.13.
Overall, the meta-analysis by Yu et al.1 showed that patients undergoing general anesthesia with LMA were less likely to develop hoarseness, coughing, and laryngospasm.
The present study has a couple of limitations. Firstly, the time of insertion and the number of attempts to insert the device were not blinded. The study is not sufficiently powered to discriminate between the two groups regarding complications and postoperative problems which may be rare in occurrence.
Conclusions
To conclude, when compared with ETTs, the LMA-S device provides the advantage of the ease of insertion, negligible rate of failure of device insertion, satisfactory ventilatory dynamics throughout the operative procedure, stable hemodynamic parameters, and a favourable profile with regards to postoperative discomfort for the surgery of laparoscopic cholecystectomy.
References
| 1 |
Yu SH, Beirne OR.
Laryngeal mask airways have a lower risk of airway complications compared with endotracheal intubation: a systematic review.
J Oral Maxillofac Surg. 2010;68(10):2359-2376.
|
| 2 |
Beleña JM, Núñez M, Anta D, et al.
Comparison of laryngeal mask airway Supreme and laryngeal mask airway Proseal with respect to oropharyngeal leak pressure during laparoscopic cholecystectomy: a randomised controlled trial.
Eur J Anaesthesiol. 2013;30(3):119-123.
|
| 3 |
Aydogmus MT, Turk HSY, Oba S, Unsal O, Sinikoglu SN.
Can SupremeTM laryngeal mask airway be an alternative to endotracheal intubation in laparoscopic surgery?
Braz J Anesthesiol. 2014;64(1):66-70.
|
| 4 |
Sharma B, Sehgal R, Sahai C, Sood J.
PLMA vs.
J Anaesthesiol Clin Pharmacol. 2010;26(4):451-457.
|
| 5 |
Beleña JM, Gracia JL, Ayala JL, et al.
The laryngeal mask airway Supreme for positive pressure ventilation during laparoscopic cholecystectomy.
J Clin Anesth. 2011;23(6):456-460.
|
| 6 |
Hoşten T, Yıldız TŞ, Kuş A, Solak M, Toker K.
Comparison of Supreme laryngeal mask airway and ProSeal laryngeal mask airway during cholecystectomy.
Balkan Med J. 2012;29(3):314-319.
|
| 7 |
Cha SM, Park S, Kang H, et al.
Gastric distension with SLIPA versus LMA ProSeal during laparoscopic cholecystectomy: a randomized trial.
Surg Laparosc Endosc Percutan Tech. 2014;24(3):216-220.
|
| 8 |
Kahla AH, Alhusainy AM.
Comparison of laryngeal mask airway Supreme and endotracheal tube in adult patients undergoing laparoscopic surgery.
Ain Shams J Anesth. 2009;2(2):73-85.
|
| 9 |
Maltby JR, Beriault MT, Watson NC, Liepert D, Fick GH.
The LMA-ProSeal is an effective alternative to tracheal intubation for laparoscopic cholecystectomy.
Can J Anaesth. 2002;49(8):857-862.
|
| 10 |
Natalini G, Franceschetti ME, Pantelidi MT, Rosano A, Lanza G, Bernardini A.
Comparison of the standard laryngeal mask airway and the ProSeal laryngeal mask airway in obese patients.
Br J Anaesth. 2003;90(3):323-326.
|
| 11 |
Patel MG, Swadia V, Bansal G.
Prospective randomized comparative study of use of PLMA and ET tube for airway management in children under general anaesthesia.
Indian J Anaesth. 2010;54(2):109-115.
|
| 12 |
Saraswat N, Kumar A, Mishra A, Gupta A, Saurabh G, Srivastava U.
The comparison of Proseal laryngeal mask airway and endotracheal tube in patients undergoing laparoscopic surgeries under general anaesthesia.
Indian J Anaesth. 2011;55(2):129-134.
|
| 13 |
Anand LK, Goel N, Singh M, Kapoor D.
Comparison of the Supreme and the ProSeal laryngeal mask airway in patients undergoing laparoscopic cholecystectomy: a randomized controlled trial.
Acta Anaesthesiol Taiwan. 2016;54(2):44-50.
|
| 14 |
Yao WY, Li SY, Yuan YJ, et al.
Comparison of Supreme laryngeal mask airway versus endotracheal intubation for airway management during general anesthesia for cesarean section: a randomized controlled trial.
BMC Anesthesiol. 2019;19(1):123.
|
| 15 |
Pournajafian A, Alimian M, Rokhtabnak F, Ghodraty M, Mojri M.
Success rate of airway devices insertion: laryngeal mask airway versus supraglottic gel device.
Anesth Pain Med. 2015;5(2):e22068.
|
| 16 |
Wong DT, Yang JJ, Jagannathan N.
Brief review: the LMA SupremeTM supraglottic airway.
Can J Anaesth. 2012;59(5):483-493.
|
| 17 |
Jarineshin H, Kashani S, Vatankhah M, Baghaee AA, Sattari S, Fekrat F.
Better hemodynamic profile of laryngeal mask airway insertion compared to laryngoscopy and tracheal intubation.
Iran Red Crescent Med J. 2015;17(8):e28615.
|
| 18 |
Barreira SR, Souza CM, Fabrizia F, Azevedo ABG, Lelis TG, Lutke C.
Prospective, randomized clinical trial of laryngeal mask airway Supreme(®) used in patients undergoing general anesthesia.
Braz J Anesthesiol. 2013;63(6):456-460.
|
| 19 |
Singam AP, Jaiswal AA, Chaudhari AR.
Comparison of laryngeal mask airway supremeTM versus endotracheal intubation in positive pressure ventilation with muscle relaxant for intraoperative and postoperative conditions.
Int J Res Med Sci. 2018;6(1):129-134.
|
| 20 |
Shribman AJ, Smith G, Achola KJ.
Cardiovascular and catecholamine responses to laryngoscopy with and without tracheal intubation.
Br J Anaesth. 1987;59(3):295-299.
|
| 21 |
Bernardini A, Natalini G.
Risk of pulmonary aspiration with laryngeal mask airway and tracheal tube: analysis on 65 712 procedures with positive pressure ventilation.
Anaesthesia. 2009;64(12):1289-1294.
|