Abstract
Background
Transversus abdominis plane (TAP) block has been demonstrated to be an effective module of multimodal analgesic treatments for infra-umbilical surgeries with limited duration of action. Various adjuvants have been studied to increase the efficacy of this technique. Herein, we evaluated the analgesic efficacy of dexmedetomidine with ropivacaine in TAP block for unilateral infra-umbilical surgeries under spinal anesthesia.
Methods
The study was conducted on 60 adult patients with the age of 18–65 years, who were planned for unilateral infra-umbilical surgeries under spinal anesthesia. These patients are randomly divided into 2 groups (30 each). In group A, 20 mL of 0.25% ropivacaine with 1 mL of normal saline, and in group B, 20 mL of 0.25% ropivacaine with 0.5 µg/kg (1 mL) dexmedetomidine was given in ultrasound-guided TAP block. Duration, quality of analgesia, and total analgesic consumption were noted. Statistical analysis was performed with SPSS software version 21.0 (IBM Corp., Armonk, NY, USA) by using Student’s
Results
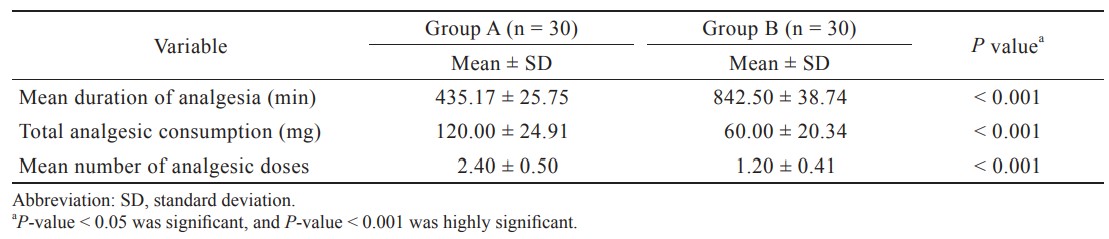
The mean duration of analgesia was significantly longer in group B than group A (842.50 ± 38.74 min and 435.17 ± 25.75 min, respectively). Verbal numerical rating scale was persistently low in both groups, except at the 7th hour and 20th hour in group A and the 12th hour in group B. Total analgesic consumption and number of analgesics doses during 24 hours after surgery were also lower in group B.
Conclusions
The addition of dexmedetomidine as adjuvant to 0.25% ropivacaine for TAP block significantly increases the duration and quality of analgesia without any significant adverse effects.
Keywords
dexmedetomidine, ropivacaine, transversus abdominis plane block
Introduction
Postoperative pain following unilateral infra-umbilical surgeries like inguinal herniorrhaphy and appendicectomy is usually moderate to severe and can cause significant morbidity ranging from patient discomfort, prolonged immobilization, thromboembolic complications, and pulmonary problems to extend hospital stay. Numerous analgesics (e.g., opioids and nonsteroidal anti-inflammatory drugs) have been tried to provide satisfactory analgesia despite their demerits. Recently, the use of peripheral nerve blocks has been encouraged to ease the above problems with better postoperative analgesia.
The transversus abdominis plane (TAP) block, first defined by Rafi1 in 2001, is an innovative, relatively straightforward, and rapidly expanding regional anesthesia technique, that anesthetizes the parietal peritoneum, muscles, and skin of abdominal wall, including lower thoracolumbar nerve roots (T7–L3). It includes the local anesthetic injection into a fascial plane between the internal oblique muscle and transversus abdominis muscle. Currently, the ultrasound-guided (USG) technique is recommended over the landmark technique to ensure precise placement of block needle as well as real time deposition of
local anesthetics (LA), thereby increasing the safety and quality of TAP block.2
Among all LA available, ropivacaine is mostly preferred in regional blocks because of its prolonged duration, less motor blockade, and better safety profile.3 Traditionally, single injections of LA result in good analgesia postoperatively, but their duration of sensory block may not be long enough to reduce the postoperative use of opioids. Therefore, the prolongation of the duration of TAP block by using various adjuvants, such as opioids, tramadol, ketamine, dexamethasone, and clonidine, has garnered significant interest.4-7
Dexmedetomidine is a selective alpha 2 (α2) adrenergic agonist with both analgesic and sedative properties. Dexmedetomidine is the pharmacologically active dextro isomer of medetomidine that causes analgesia and sedation without any respiratory complication.8,9 Due to its unique mechanism of action, it differs from those currently used agents like clonidine. Although the efficacy of dexmedetomidine as an adjuvant is proven in other nerve blocks, the data supporting its use in TAP block are still scarce. Hence, we planned to evaluate the analgesic efficacy of dexmedetomidine as an adjuvant to ropivacaine in TAP block for unilateral infra-umbilical surgeries in terms of duration and quality of analgesia along with total analgesic consumption during 24 hours.
Methods
This prospective, randomized clinical trial was conducted over the period of 18 months in agreement with the principles of Declaration of Helsinki 2013 and as per the guidelines of Indian Council of Medical Research for biomedical research in human subjects. After we obtained the approval from the institutional ethical committee and registered the trial with the Clinical Trial Registry of India (CTRI/2019/04/025381), 60 adult patients of either sex, aged 18–65 years, of American Society of Anesthesiologists (ASA) I or II status, scheduled for various elective unilateral infra-umbilical surgeries like inguinal herniorrhaphy and appendicectomy under spinal anesthesia were enrolled in the study. The exclusion criteria involved patient’s refusal, any contraindication to regional block, history of allergy to the studied drugs, psychiatric disorders, chronic opioid use, infection at block site, body mass index (BMI) > 30 kg/m2, and diabetes mellitus. All the patients were randomly divided into two groups of 30 patients by computer generated randomization table. Group A received 20 mL of 0.25% ropivacaine with 1 mL of normal saline, and group B received 20 mL of 0.25% ropivacaine with dexmedetomidine 0.5 µg/kg (1 mL) through USG TAP block.
On the day before surgery, thorough preoperative assessment of the patients was done by an anesthesiologist, and they were explained about the verbal numerical rating scale (VNRS) for pain intensity along with risks and benefits associated with the procedure. A written informed consent was obtained from all the patients prior to surgery. Each patient received premedication of tablet, alprazolam 0.25 mg and tablet, and ranitidine 150 mg orally at night before surgery. All patients were kept fasting as per standard guidelines before surgery.
After the arrival of the patients in the operative room, standard monitors like ECG, pulse oximeter, and noninvasive blood pressure were attached, and baseline parameters were recorded. Preloading was done with intravenous (i.v.) infusion of crystalloid solution after securing i.v. access. Spinal anesthesia was given in sitting position at L3–L4 level by using 3 mL of 0.5% heavy bupivacaine under all aseptic precautions. The surgery was allowed after achieving T6 level of block, and vitals were monitored throughout the surgery. Hypotension, defined as the fall in mean arterial pressure of > 20% of baseline values, was treated with fluid bolus, and if hypotension remained uncorrected in patients, i.v. mephentermine 3 mg bolus was given. Bradycardia, defined as pulse rate of ≤ 50/min, was treated with an i.v. atropine 0.6 mg. At the end of the surgical procedure, we used all aseptic precautions and performed USGTAP block on patients in supine position on the side of surgery by posterior approach which covered anterior and lateral abdominal wall at the infra-umbilical area between costal margin and iliac crest supplied by T7–12 segmental thoracolumbar nerves. After the sterilization of skin, a linear high frequency probe (5–10 MHz) of ultrasound machine (Esaote My Lab) was sheathed and placed in mid axillary line to scan the abdominal muscle. The ultrasound transducer probe was moved more posteriorly to view the transversus abdominis fascial plane. With an adequate ultrasound image, 23G Quincke spinal needle (Becton Dickinson [BD], Franklin Lakes, NJ, USA) attached to 10 cm extension line for drug infusion was inserted medially by the plane approach and directed towards the TAP. After we assured the correct position of the needle between the internal oblique and transversus abdominis muscles, the study drugs were injected as per group allocation. The correct placement of the injection was confirmed by the separation of the fascial plane, and the formation of a well-defined, hypoechoic, and elliptical shape between both muscles on ultrasound image.
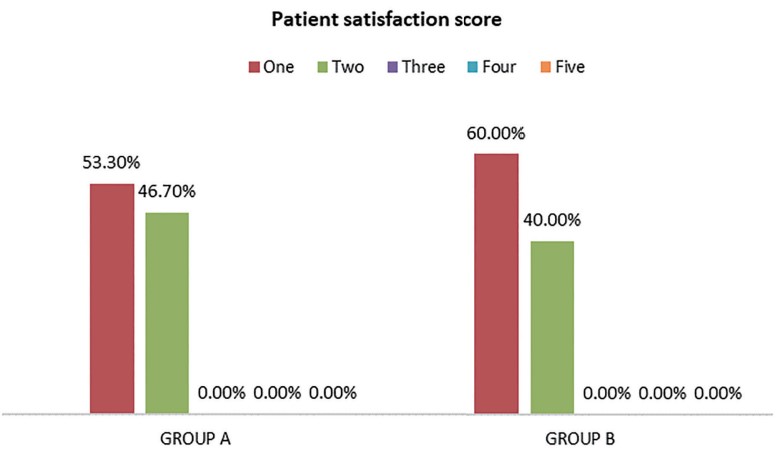
Postoperatively, all patients were observed for vital parameters and quality of analgesia at every hour for the first 8 hours, then at 12, 16, 20, and 24 hours. Quality of analgesia was assessed by using four-point VNRS as 0 = no pain, 1–3 = mild pain, 4–7 = moderate pain, and 8–10 = severe pain. Rescue analgesia was given to the patient, who showed VNRS > 3, in the form of injection tramadol 50 mg i.v. If the patient still had VNRS > 3, second rescue analgesic drug injection of diclofenac 75 mg i.v. was given. The total of analgesic consumption and the number of rescue doses given during the first 24 hours after surgery were recorded. Duration of analgesia as the primary outcome of this study was noted and defined as the time from the completion of injection to the request of first rescue analgesia. Patient satisfaction score was measured with a five-point numerical scale (1 = very satisfied, 2 = satisfied, 3 = undecided, 4 = dissatisfied, 5 = very dissatisfied) at the end of 24 hours after surgrey. Any adverse effects, such as nausea and vomiting, hypotension, sedation, and block related complication, were noted and managed accordingly. The sedation score was recorded on the modified Ramsay Sedation Score (RSS).10
Statistical Analysis
Based on previous literature, to detect the minimum mean difference of the 4-hour duration of analgesia (primary outcome) between the two groups, we used 80% power along with 5% probability of type one error to calculate a sample size of 26 patients in each group. We had enrolled 60 patients (30 in each group) to cover any drop out. After completion of the study, all the data were compiled and analyzed by using IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY, USA). Data were presented as mean ± SD, absolute numbers, or percentage. Student’s
Results
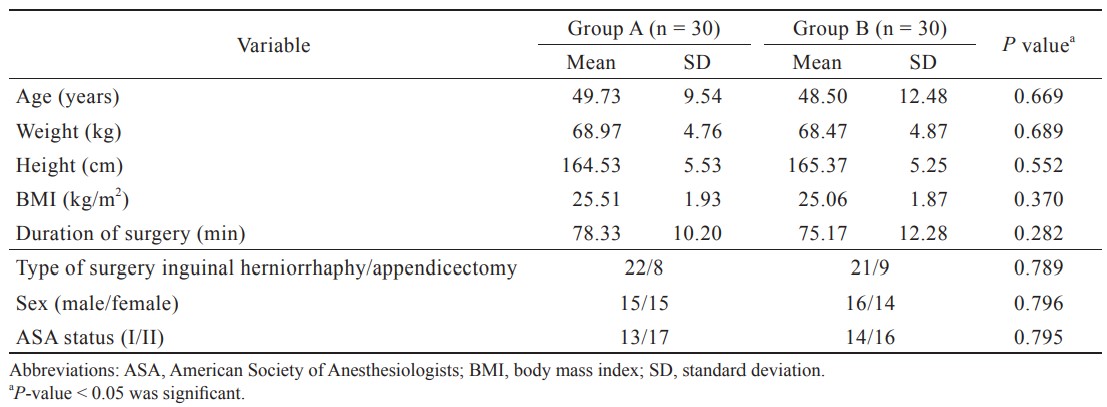
Regarding demographic parameters including age, sex, weight, BMI, ASA I–II status, and type and duration of surgery, both groups were comparable without any statistically significant difference (Table 1). Hemodynamic parameters were comparable in both groups intraoperatively and postoperatively. The duration of analgesia or the time to first rescue analgesia was significantly longer in group B than group A with mean duration of 842.50 ± 38.74 minutes and 435.17 ± 25.75 minutes, respectively (
Postoperatively, total analgesic consumption during 24 hours in the form of injection tramadol was significantly more in group A than group B (Table 2). Moreover, patients in group A required increased mean number of rescue analgesic doses (2.40 ± 0.50) than group B (1.20 ± 0.41) during 24 hours after surgrey (
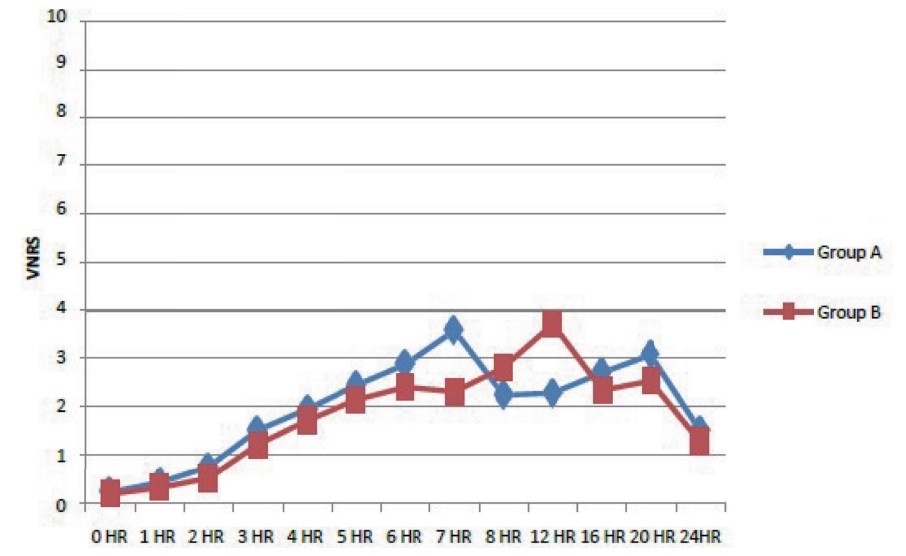
Download full-size image
Abbreviation: HR, hour.
Download full-size image
Download full-size image
Download full-size image
Discussion
USG TAP block which was first described by Hebbard et al.2 has increased the safety, accuracy, and success rate of this regional technique. TAP blocks have been labelled as an active element of multimodal analgesic regimens for various abdominal surgeries, including appendectomy, cholecystectomy, inguinal hernia repair, cesarean section, total abdominal hysterectomy, open prostatectomy, and renal transplant surgery.11-14 Different studies were carried out to demonstrate the analgesic efficacy and safety of dexmedetomidine in neuraxial and peripheral blocks. At spinal level by inhibiting release of substance P at the dorsal root neurons and at supraspinal level by activating α2-adrenoreceptors in locus coeruleus, it acts as a good analgesic.15,16 The local vasoconstrictive effects of dexmedetomidine may prolong the duration of analgesia by reducing the systemic absorption of the LA from the action site.17 Dexmedetomidine has been shown to be safe and effective adjuvant for different peripheral nerve blocks like brachial plexus block, femoral block, and pectoral nerve block,18,19 but the data regarding analgesic efficacy of dexmedetomidine (0.5 µg/kg) with 0.25% ropivacaine in TAP block are very sparse. Hence, we decided to study the efficacy of dexmedetomidine with ropivacaine for TAP block.
The various studies conducted had used different doses and concentration of ropivacaine (0.250%, 0.375%, and 0.500%) for TAP block.20 The exact dose and volume of ropivacaine for TAP block have not been described in previous studies. In all the previous studies, dexmedetomidine was used in doses of 0.25–2.00 µg/kg for peripheral blocks and obtained different results. Because the higher doses were associated with more side effects and the use of lower doses was not effective enough in prolonging the anesthesia,21 we used medium dose range, i.e., 0.5 µg/kg of dexmedetomidine as adjuvant to 20 mL of 0.25% ropivacaine for TAP block.
The present study found that the addition of 0.5 µg/kg dexmedetomidine to 20 mL of 0.25% ropivacaine for TAP block had prolonged the duration of analgesia with better quality of analgesia in view of low VNRS pain score and less total analgesic consumption during 24 hours after surgery in patients undergoing infra-umbilical surgeries. VNRS scores remained persistently lower than 3 for the initial 6 hours in group A and 12 hours in group B, which correlates well with the duration of analgesia.
These results were in concordance with the study done by Ramya Parameswari and Udayakumar,22 who used 0.5 ug/kg with 0.25% bupivacaine for TAP block after cesarean section and found the time to first rescue analgesia was 14.25 hours in dexmedetomidine group and 7.73 hours in the group of bupivacaine alone. Total opioid requirement during 24 hours after surgery was also less in dexmedetomidine group. Another study done by Qian et al.23 had similar finding, where they used 0.5 ug/kg-1 dexmedetomidine as an additive to 20 mL of 0.3% ropivacaine (RD group) for TAP block on 70 patients for cesarean section and found longer duration of analgesia in RD group than ropivacaine alone (R group), i.e., 11.60 ± 2.11 hours vs. 7.10 ± 1.21 hours, respectively. Postoperative visual analog scale (VAS) pain scores were also significantly lower in the RD group at 6 and 8 hours after surgery than the R group.
Another study24 reported that patients undergoing lower abdominal surgeries had shown reduced postoperative pain score (VAS score) up to 12 hours after TAP block with dexmedetomidine as compared with ropivacaine alone. Similarly, Xu et al.25 also found that TAP block after emergency abdominal surgery with RD reduced the postoperative pain score up to 12 hours prolonged the time to the first use of patient-controlled analgesia (PCA) and reduced the overall use of PCA when compared with the use of ropivacaine alone. However, Ding et al.26 reported that adding dexmedetomidine did not significantly improve the quality or duration of TAP block. Different does and concentrations of ropivacaine and dexmedetomidine and the analgesics used after surgery may explain these differences in the results.
Hypotension bradycardia and sedation are considered to be the most prominent adverse effects of α2-agonists. Therefore, hemodynamic parameters, including heart rate, blood pressure, oxygen saturation, and respiratory rate, were monitored during both intra- and postoperative period in our study which were found comparable in both groups. These results are similar to the study conducted by Andurkar and Suryavanshi27 where 0.5 µg/kg dexmedetomidine was added to 0.25% bupivacaine in TAP block for lower segment caesarean sections, and no statistically significant difference with respect to the hemodynamics (HR, MAP, SpO2) in both groups was found. In the present study, none of our patients had bradycardia, hypotension, sedation, nausea, vomiting, or respiratory depression, and this may be due to the lower dose of dexmedetomidine (0.5 µg/kg). Similarly, other studies using a similar dose of dexmedetomidine found no adverse effects in patients receiving dexmedetomidine.23
Limitations of Study
The present study had certain limitations. Firstly, whether the action of dexmedetomidine was related to systemic absorption or pure local effect was not fully elucidated. Further research is necessary to determine the plasma levels of dexmedetomidine. Secondly, in literature, TAP block has been performed with stimuplex needle as it has a blunt end, but in our study, we used Quincke spinal needle because of cost constraints, and we performed USG TAP block carefully without any complication. Thirdly, the onset time of TAP block was uncertain in our study as the patients were still under the effect of spinal anesthesia at the time of block placement. Fourth, larger series need to be done with different dosage of dexmedetomidine to find the optimal dose that most effectively prolongs postoperative analgesia.
Conclusions
From the current study, we conclude that the addition of dexmedetomidine (0.5 µg/kg) as an adjuvant to 0.25% ropivacaine in TAP block significantly prolonged the duration of postoperative analgesia along with better quality of analgesia in terms of low VNRS scores and reduced analgesic consumption during 24 hours after surgery with no significant side effects.
References
| 1 |
Rafi AN.
Abdominal field block: a new approach via the lumbar triangle.
Anaesthesia. 2001;56(10):1024-1026.
|
| 2 |
Hebbard P, Fujiwara Y, Shibata Y, Royse C.
Ultrasound-guided transversus abdominis plane (TAP) block.
Anaesth Intensive Care. 2007;35(4):616-617.
|
| 3 |
Kuthiala G, Chaudhary G.
Ropivacaine: a review of its pharmacology and clinical use.
Indian J Anaesth. 2011;55(2):104-110.
|
| 4 |
Singh R, Kumar N, Jain A, Joy S.
Addition of clonidine to bupivacaine in transversus abdominis plane block prolongs postoperative analgesia after cesarean section.
J Anaesthesiol Clin Pharmacol. 2016;32(4):501-504.
|
| 5 |
Kiran S, Bala R, Kumar K.
Comparison of analgesic efficacy of dexamethasone versus tramadol as adjuvant to ropivacaine for oblique subcostal transversus abdominis plane block in open cholecystectomy.
Indian J Pain. 2019;33(3):141-146.
|
| 6 |
Karasu D, Yilmaz C, Ozgunay SE, Yalcin D, Ozkaya G.
Ultrasound-guided transversus abdominis plane block for postoperative analgesia in laparoscopic cholecystectomy: a retrospective study.
North Clin Istanb. 2020;8(1):88-94.
|
| 7 |
John R, Ranjan RV, Ramachandran TR, George SK.
Analgesic efficacy of transverse abdominal plane block after elective cesarean delivery—bupivacaine with fentanyl versus bupivacaine alone: a randomized, double-blind controlled clinical trial.
Anesth Essays Res. 2017;11(1):181-184.
|
| 8 |
Afshani N.
Clinical application of dexmedetomidine.
South Afr J Anaesth Analg. 2010;16(3):50-56.
|
| 9 |
Naaz S, Ozair E.
Dexmedetomidine in current anaesthesia practice—a review.
J Clin Diagn Res. 2014;8(10):GE01-GE04.
|
| 10 |
Kaur S, Gupta KK, Singh A, Sunita, Baghla N.
Arousal from sedation in lower abdominal surgeries under spinal anesthesia: comparison between dexmedetomidine and clonidine.
Anesth Essays Res. 2016;10(1):98-103.
|
| 11 |
Shin HJ, Kim ST, Yim KH, Lee HS, Sim JH, Shin YD.
Preemptive analgesic efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing gynecologic surgery via a transverse lower abdominal skin incision.
Korean J Anesthesiol. 2011;61(5):413-418.
|
| 12 |
O’Donnell BD, McDonnell JG, McShane AJ.
The transversus abdominis plane (TAP) block in open retropubic prostatectomy.
Reg Anesth Pain Med. 2006;31(1):91.
|
| 13 |
Niraj G, Searle A, Mathews M, et al.
Analgesic efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing open appendicectomy.
Br J Anaesth. 2009;103(4):601-605.
|
| 14 |
Mukhtar K, Singh S.
Transversus abdominis plane block for laparoscopic surgery.
Br J Anaesth. 2009;102(1):143-144.
|
| 15 |
Marhofer D, Kettner SC, Marhofer P, Pils S, Weber M, Zeitlinger M.
Dexmedetomidine as an adjuvant to ropivacaine prolongs peripheral nerve block: a volunteer study.
Br J Anaesth. 2013;110(3):438-442.
|
| 16 |
Al-Metwalli RR, Mowafi HA, Ismail SA, et al.
Effect of intra-articular dexmedetomidine on postoperative analgesia after arthroscopic knee surgery.
Br J Anaesth. 2008;101(3):395-399.
|
| 17 |
Kosugi T, Mizuta K, Fujita T, Nakashima M, Kumamoto E.
High concentrations of dexmedetomidine inhibit compound action potentials in frog sciatic nerves without alpha(2) adrenoceptor activation.
Br J Pharmacol. 2010;160(7):1662-1676.
|
| 18 |
El-Boghdadly K, Brull R, Sehmbi H, Abdallah FW.
Perineural dexmedetomidine is more effective than clonidine when added to local anesthetic for supraclavicular brachial plexus block: a systematic review and meta-analysis.
Anesth Analg. 2017;124(6):2008-2020.
|
| 19 |
Abdulatif M, Fawzy M, Nassar H, Hasanin A, Ollaek M, Mohamed H.
The effects of perineural dexmedetomidine on the pharmacodynamic profile of femoral nerve block: a dose-finding randomised, controlled, double-blind study.
Anaesthesia. 2016;71(10):1177-1185.
|
| 20 |
Abdul Jalil RM, Yahya N, Sulaiman O, et al.
Comparing the effectiveness of ropivacaine 0.
Acta Anaesthesiol Taiwan. 2014;52(2):49-53.
|
| 21 |
Zeng Y, Wen Y, Yang J, Sun H.
Comparing post-operative analgesic effects of varying doses of dexmedetomidine as an adjuvant to ropivacaine for ultrasound-guided dual transversus abdominis plane block following laparotomy for gynecologic malignancies.
Exp Ther Med. 2020;20(2):860-867.
|
| 22 |
Ramya Parameswari A, Udayakumar P.
Comparison of efficacy of bupivacaine with dexmedetomidine versus bupivacaine alone for transversus abdominis plane block for post-operative analgesia in patients undergoing elective caesarean section.
J Obstet Gynaecol India. 2018;68(2):98-103.
|
| 23 |
Qian H, Zhang Q, Zhu P, et al.
Ultrasound-guided transversus abdominis plane block using ropivacaine and dexmedetomidine in patients undergoing caesarian sections to relieve post-operative analgesia: a randomized controlled clinical trial.
Exp Ther Med. 2020;20(2):1163-1168.
|
| 24 |
Mishra M, Mishra SP, Singh SP.
Ultrasound-guided transversus abdominis plane block: what are the benefits of adding dexmedetomidine to ropivacaine?
Saudi J Anaesth. 2017;11(1):58-61.
|
| 25 |
Xu L, Hu Z, Shen J, McQuillan PM.
Efficacy of US-guided transversus abdominis plane block and rectus sheath block with ropivacaine and dexmedetomidine in elderly high risk patients.
Minerva Anestesiol. 2018;84(1):18-24.
|
| 26 |
Ding W, Li W, Zeng X, et al.
Effect of adding dexmedetomidine to ropivacaine on ultrasound-guided dual transversus abdominis plane block after gastrectomy.
J Gastrointest Surg. 2017;21(6):936-946.
|
| 27 |
Andurkar US, Suryavanshi MR.
Dexmedetomidine: a wonder drug for tap block in patients undergoing elective caesarean section for postoperative pain relief.
J Evid Based Med Healthc. 2018;5(28):2139-2143.
|