Abstract
Background
Lumbar facet joint (LFJ) pain was reported to occur in 27%–40% of patients with chronic low back pain (LBP). Several therapeutic procedures such as corticosteroid injection (CI) and radiofrequency (RF) ablation have been used. However, there is no clear consensus that one is superior to the other. This study aimed to perform a meta-analysis to compare the effectiveness of CI and RF ablation for LFJ pain.
Methods
This study was conducted by searching for all randomized controlled trials comparing the effect of CI and RF ablation on LFJ pain in Cochrane Central Register of Controlled Trials and PubMed database. We performed inverse-variance weighted meta-analysis of outcomes including pain intensity and functional disability at 3, 6, and 12-month measurement by using RevMan 5.3 (Cochrane, London, England).
Results
CI was associated with a higher pain intensity score when compared to RF ablation at 3 months (3 trials; standardized mean difference [SMD], 1.09; 95% CI, 0.79 to 1.38;
Conclusions
Pooled analysis from limited trials showed a benefit of RF to the improvement of pain intensity and functional disability when we compared RF with CI for the treatment of LFJ pain.
Keywords
corticosteroid injection, denervation, facet joint, low back pain, radiofrequency
Introduction
More than a quarter of patients with chronic lower back pain (LBP) have been reported to have pain originated from lumbar facet joints (LFJs).1 Meanwhile, LFJ pain is mostly caused by degenerative osteoarthritis.2 Some therapeutic procedures have been used for the management of LBP originated from LFJ. Due to its anti-inflammatory effect, LFJ injection with corticosteroid is a beneficial option for treating LBP caused by facet joint osteoarthritis.3 On the other hand, the application of radiofrequency (RF) ablation in patients with LFJ pain has been reported to effectively reduce the pain score and improve the quality of life.4
A few studies have explored the effectiveness of facet interventions for chronic lumbar pain, but there has been no clear consensus of which procedures are more superior. This study aimed to perform a meta-analysis to compare the effectiveness of corticosteroid injection (CI) and RF ablation for the treatment of LFJ pain.
Methods
This study followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.5 All randomized controlled trials (RCTs) comparing the pain intensity of CI with RF ablation for the treatment of LFJ pain were eligible for inclusion. The procedure of RF ablation could be either continuous or pulse RF. All studies investigating issues other than patients with LFJ pain were excluded.
Ethical clearance was obtained before a systematic search of the literature. The searched terms “radiofrequency or denervation,” “steroid or corticosteroid,” “facet joint,” and “trial” were subjected to PubMed and Cochrane Library database on September 10, 2020, and evaluated for their presence in the title, abstract, and medical subject heading. The reference list of each study that we found was also evaluated and screened to identify any other relevant studies.
Screening of titles and abstracts was conducted independently by two authors before obtaining full papers for final inclusion. Data extraction included author, the year of publication, the age of population, the number of patients, intervention, pain intensity score, functional disability score, and adverse events. Any relevant data reported in graphical form using ImageJ (ImageJ v1.52k January 2019: http://wsr.imagej.net/distros/win/ij152-win-java8.zip) were extracted if there was no further information from corresponding authors.
Two independent authors performed methodological quality evaluation using the Cochrane Collaboration Risk of Bias Tool and the Grades of Recommendation Assessment, Development and Evaluation (GRADE) approach.6,7 Pain intensity was assessed by either visual analogue scale or numerical rating scale and was pooled as a primary outcome. Pain intensity measurement was categorized into three periods (3, 6, and 12 months). The secondary outcome was the functional disability measured via Oswestry Disability Index. The analysis was conducted by using standardized mean difference (SMD) for pain intensity, whereas mean difference (MD) was used for functional disability. Fixed-effects method was implemented by using Review Manager (RevMan v5.3 2014; Cochrane, London, England). When the heterogeneity was greater than 50%, the I2 statistic, random-effects model analysis was applied. Sensitivity analysis was performed by not only removing data that were retrieved using ImageJ but also removing high risk of bias study.
Results
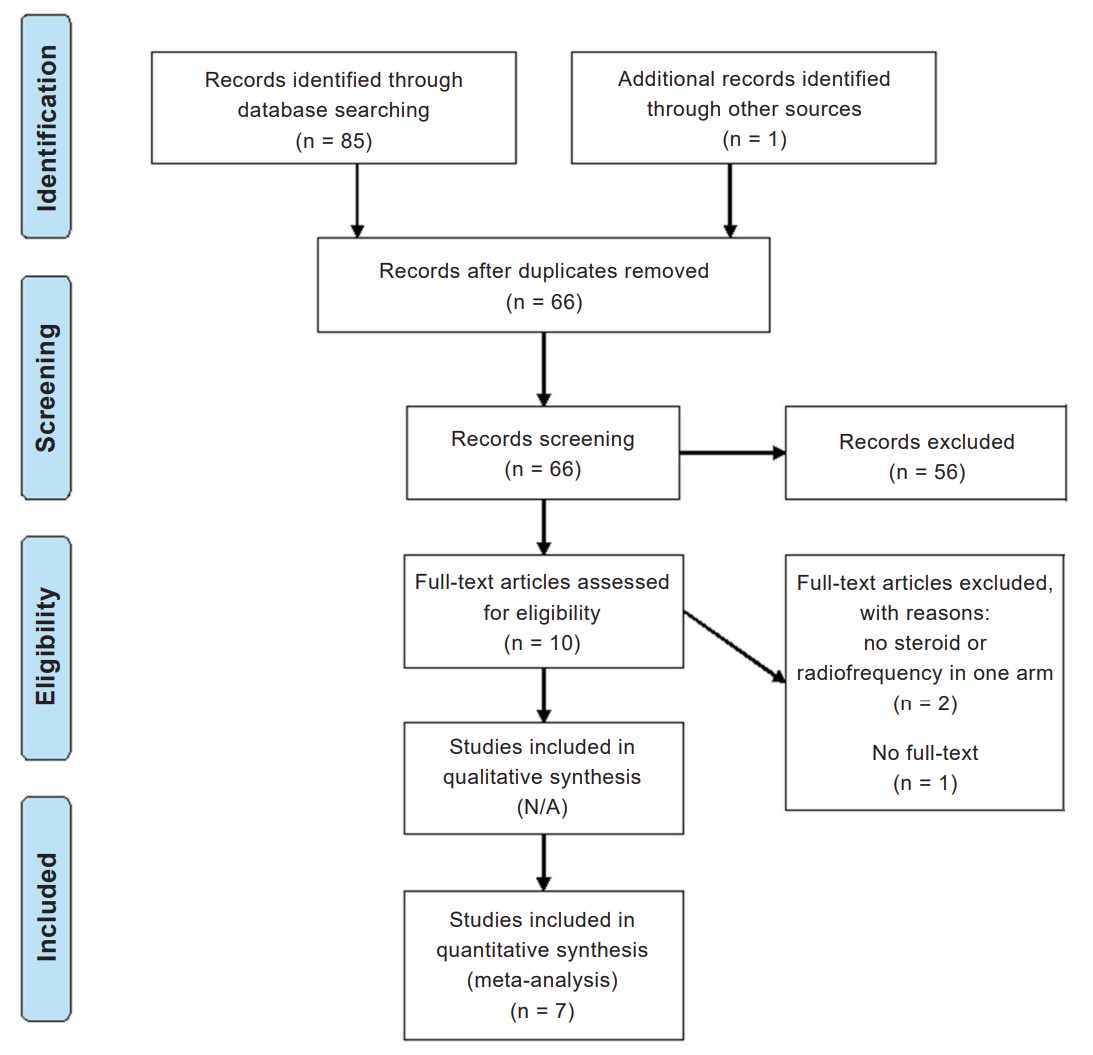
Systematic search of literature revealed 58 records in PubMed, 27 in the Cochrane Library database, and 1 from other sources, among which 20 were duplicates (Figure 1). Ten studies were then retrieved for full text review. However, 3 studies were excluded because two of them did not use steroid or RF in one arm, and the other one was unavailable in full text. In total, 7 studies were finally included in our analysis.8-14
Download full-size image
Abbreviation: PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
The characteristics of the 7 included studies8-14 are presented in Table 1. All studies used a combination of corticosteroid and local anesthetic agents for CI groups. The corticosteroid agents were methylprednisolone in 4 trials, betamethasone in 2 trials, and dexamethasone in 1 trial. Pulsed RF was performed in 4 trials, whereas continuous RF was performed in 3 trials. Three trials did not identify adverse event. In one study, two subjects experienced an increase of LBP in the follow-up period.8
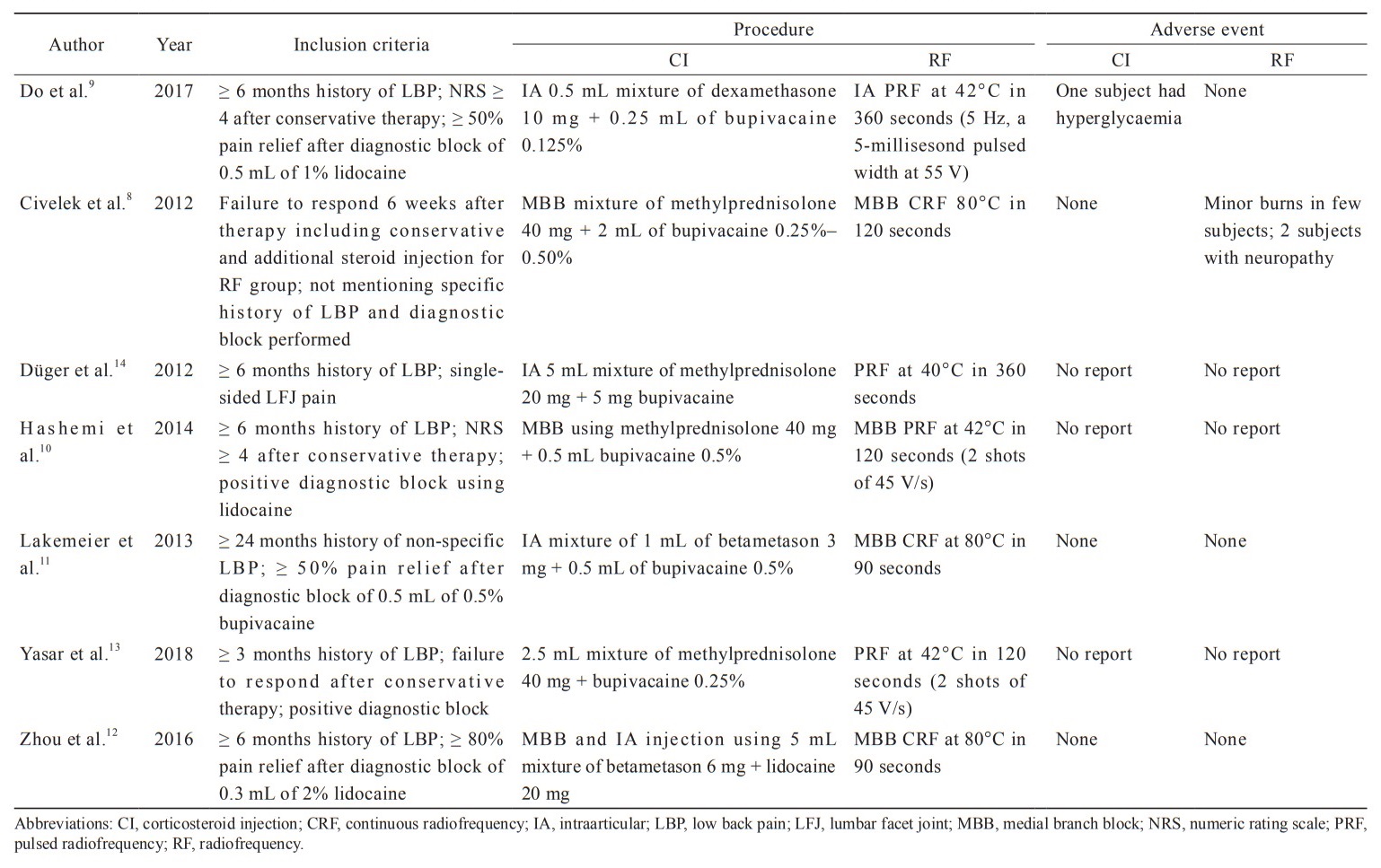
Download full-size image
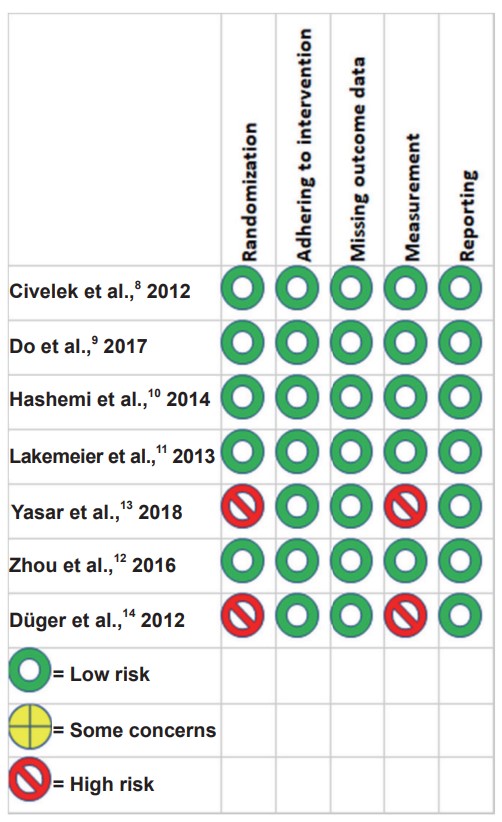
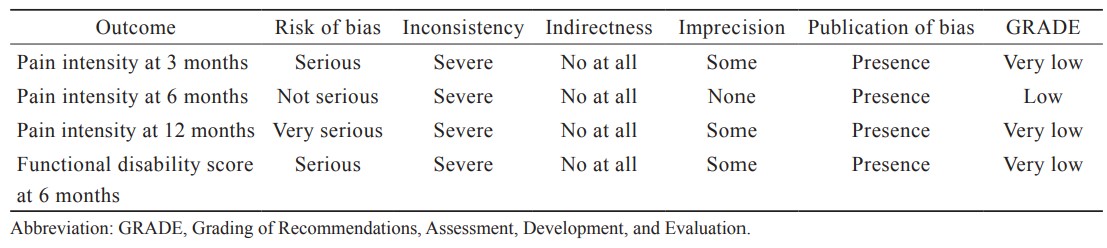
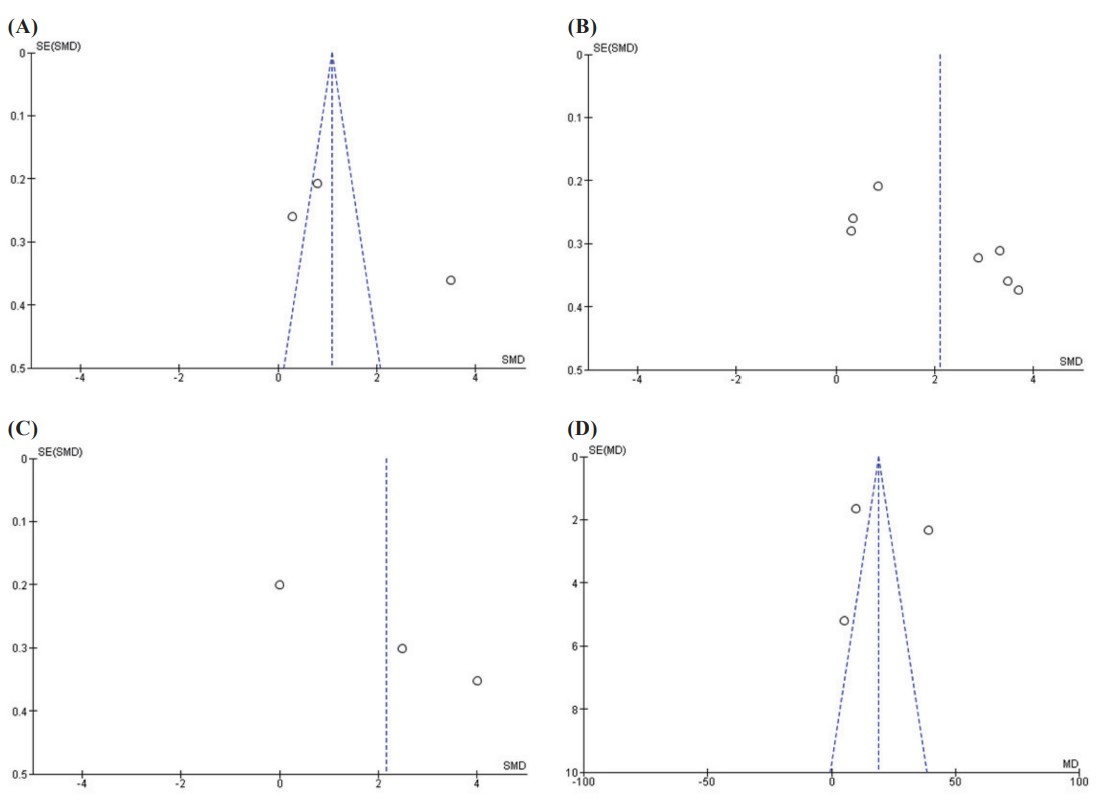
The risk of bisa across the domains is presented in Figure 2.8-14 The method of randomizations, adherence to interventions, missing outcome data, measurement, and reporting were considered adequate in 5 studies. Two studies were considered high risk of bias because they did not mention randomization and blinding-to-assessor process.13,14 The quality of evidence for each outcome is presented in Table 2. We downgraded two levels from the risk of bias and inconsistency for all outcomes but pain intensity at 6-month period because of the serious risk of bias and substantial heterogeneity. Publication bias was detected in all outcomes as shown in Figure 3.
Download full-size image
Download full-size image
Download full-size image
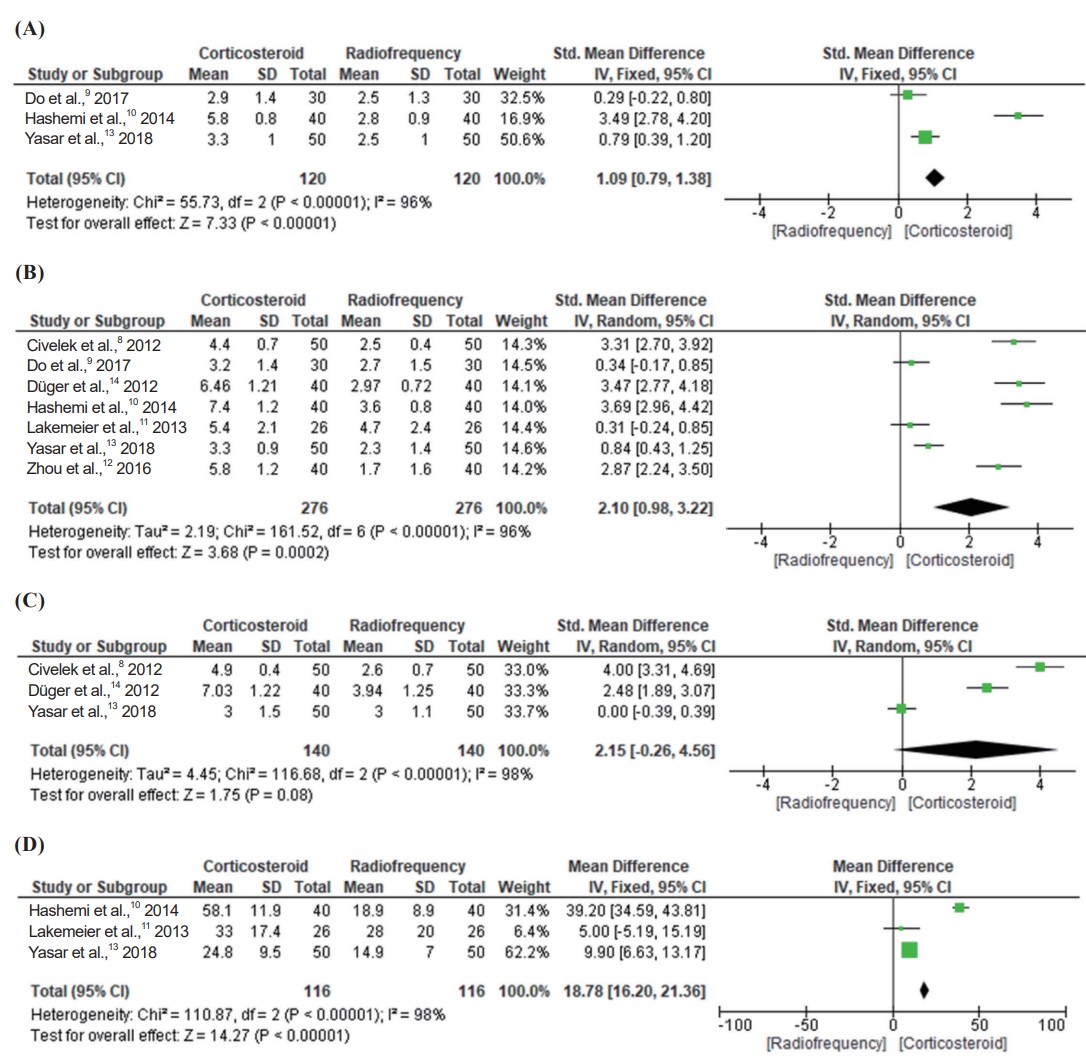
(A) Pain intensity at 3 months. (B) Pain intensity at 6 months. (C) Pain intensity at 12 months. (D) Functional disability at 6 months.
Seven studies involving 552 patients reported pain intensity score (Figure 4). Treatment with CI was associated with higher pain intensity score than RF ablation (3 trials; SMD, 1.09; 95% CI, 0.79 to 1.38;
Download full-size image
(A) Pain intensity at 3 months. (B) Pain intensity at 6 months. (C) Pain intensity at 12 months. (D) Functional disability at 3 months.
Sensitivity analysis by removing data10 that were retrieved by using ImageJ showed a similar result of pain intensity at 3 months (SMD, 0.60; 95% CI, 0.28 to 0.92;
Three studies including 232 patients reported functional disability score at 6 months. According to the meta-analysis as shown in Figure 4D, the CI group had a higher functional disability score than RF ablation (3 trials; MD, 18.78; 95% CI, 16.20 to 21.36;
Discussion
This meta-analysis showed that RF ablation was associated with lower pain intensity score and lower functional disability score when compared to CI. An earlier Cochrane systematic review including fewer studies reported that RF ablation was more effective than CI with very low-quality of evidence for pain relief at 3–6-month follow-up period.15 Recent pooled analysis done by Chen et al.16 involving patients with not only chronic lumbar but also sacroiliac joint pain also reported similar results.
Some studies17-19 reported that CI combined with a local anesthetic agent might be beneficial to the treatment of chronic LFJ pain. However, recent trial comparing intraarticular (IA) injection with corticosteroid and saline reported that steroid injection has no benefit of prolonging the time to the requirement of further treatments for facet joint pain.20 A study suggested that although the long-term efficacy for facet blocks lack, it might provide prognostic value before RF ablation.21 However, the dose of steroid used in their study was lower than the equipotent doses.
For CI groups, there were two approaches of CI among the studies: IA and medial branch block (MBB). IA blocks are difficult to perform, more painful than MBB, which had lower technical failure rate.22 The needle is positioned at the junction of the superior articular and transverse processes for MBB, whereas the needle for IA is positioned to be within the joint. Lumbar MBB should be performed with a volume < 0.5 mL in order to prevent the spread to adjacent structures, and IA injections should be done with a volume < 1.5 mL in order to prevent aberrant spread and capsular rupture.23
IA injections would be more accurate than MBB because 10%–15% of joints receive aberrant innervations from nerves other than the medial branches.24 Ackerman and Ahmad25 found that 61% of those who received IA blocks achieved a sustained relief of 12 weeks post-procedure compared with 26% of those who received MBB. IA injections may be considered an option of treatment for some individuals (e.g., young people with inflammatory pain, people at risk of RF ablation complications).23
For RF groups, there were two methods performed in the included studies: pulsed and continuous RF. A meta-analysis showed that continuous RF ablation significantly decreased pain score compared with control treatments at the 6 and 12-month follow-up periods.26 However, it would increase the risk of nerve injury. An included trial8 reported burns and neuropathy as adverse events related to continuous RF ablation.
There were several limitations in this study. First, most of the included studies involved small sample sizes. Secondly, there was substantial heterogeneity among the studies. The sensitivity analysis also showed no improvement in heterogeneity, which might be attributed to the variation in procedures and agents among trials.
Conclusions
Pooled analysis from limited trials showed that RF can be beneficial to the improvement of pain intensity and functional disability when compared to CI for the treatment of LFJ pain. More RCTs with proper homogeneous data are required to improve the quality of evidence.
References
| 1 |
Datta S, Lee M, Falco FJE, Bryce DA, Hayek SM.
Systematic assessment of diagnostic accuracy and therapeutic utility of lumbar facet joint interventions.
Pain Physician. 2009;12(2):437-460.
|
| 2 |
Perolat R, Kastler A, Nicot B, et al.
Facet joint syndrome: from diagnosis to interventional management.
Insights Imaging. 2018;9(5):773-789.
|
| 3 |
Kwak DG, Kwak SG, Lee AY, Chang MC.
Outcome of intra-articular lumbar facet joint corticosteroid injection according to the severity of facet joint arthritis.
Exp Ther Med. 2019;18(5):4132-4136.
|
| 4 |
Çetin A, Yektaş A.
Evaluation of the short-and long-term effectiveness of pulsed radiofrequency and conventional radiofrequency performed for medial branch block in patients with lumbar facet joint pain.
Pain Res Manag. 2018;2018:7492753.
|
| 5 |
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group.
Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement.
Open Med. 2009;3(3):e123-e130.
|
| 6 |
Higgins JPT, Sterne JAC, Savović J, et al.
A revised tool for assessing risk of bias in randomized trials.
Cochrane Database Syst Rev. 2016;10(Suppl 1):29-31.
|
| 7 |
Ryan R, Hill S.
How to GRADE the quality of the evidence.
https://cgf.cochrane.org/sites/cgf.cochrane.org/files/public/uploads/uploads/how_to_grade.pdf.. Published December 2016. Accessed July 13, 2019.
|
| 8 |
Civelek E, Cansever T, Kabatas S, et al.
Comparison of effectiveness of facet joint injection and radiofrequency denervation in chronic low back pain.
Turk Neurosurg. 2012;22(2):200-206.
|
| 9 |
Do KH, Ahn SH, Cho YW, Chang MC.
Comparison of intra-articular lumbar facet joint pulsed radiofrequency and intra-articular lumbar facet joint corticosteroid injection for management of lumbar facet joint pain: a randomized controlled trial.
Medicine (Baltimore). 2017;96(13):e6524.
|
| 10 |
Hashemi M, Hashemian M, Mohajerani SA, Sharifi G.
Effect of pulsed radiofrequency in treatment of facet-joint origin back pain in patients with degenerative spondylolisthesis.
Eur Spine J. 2014;23(9):1927-1932.
|
| 11 |
Lakemeier S, Lind M, Schultz W, et al.
A comparison of intraarticular lumbar facet joint steroid injections and lumbar facet joint radiofrequency denervation in the treatment of low back pain: a randomized, controlled, double-blind trial.
Anesth Analg. 2013;117(1):228-235.
|
| 12 |
Zhou Q, Zhou F, Wang L, Liu K.
An investigation on the effect of improved X-rays-guided radiofrequency thermocoagulation denervation on lumbar facet joint syndrome.
Clin Neurol Neurosurg. 2016;148:115-120.
|
| 13 |
Yasar D, Korgun O, Emine D.
Radiofrequency and methylprednisolone in treatment of lower back pain caused by facet joint syndrome: comparison of the outcomes.
Asian J Neurosurg. 2018;13(2):283-287.
|
| 14 |
Düger C, IÖ Kol, Kaygusuz K, Gürsoy S, Mimaroglu C.
Effects of facet joint nerve block addition to radiofrequency in the treatment of low back pain.
Healthmed. 2012;6(6):2052-2056.
|
| 15 |
Maas ET, Ostelo RWJG, Niemisto L, et al.
Radiofrequency denervation for chronic low back pain.
Cochrane Database Syst Rev. 2015;10:CD008572.
|
| 16 |
Chen CH, Weng PW, Wu LC, Chiang YF, Chiang CJ.
Radiofrequency neurotomy in chronic lumbar and sacroiliac joint pain: a meta-analysis.
Medicine (Baltimore). 2019;98(26):e16230.
|
| 17 |
Manchikanti L, Singh V, Falco FJE, Cash KA, Pampati V.
Evaluation of lumbar facet joint nerve blocks in managing chronic low back pain: a randomized, double-blind, controlled trial with a 2-year follow-up.
Int J Med Sci. 2010;7(3):124-135.
|
| 18 |
Celik B, Er U, Simsek S, Altug T, Bavbek M.
Effectiveness of lumbar zygapophysial joint blockage for low back pain.
Turk Neurosurg. 2011;21(4):467-470.
|
| 19 |
Kawu AA, Olawepo A, Salami AOO.
Facet joints infiltration: a viable alternative treatment to physiotherapy in patients with low back pain due to facet joint arthropathy.
Niger J Clin Pract. 2011;14(2):219-222.
|
| 20 |
Kennedy DJ, Fraiser R, Zheng P, et al.
Intra-articular steroids vs saline for lumbar Z-joint pain: a prospective, randomized, double-blind placebo-controlled trial.
Pain Med. 2019;20(2):246-251.
|
| 21 |
Cohen SP, Doshi TL, Constantinescu OC, et al.
Effectiveness of lumbar facet joint blocks and predictive value before radiofrequency denervation: the facet treatment study (FACTS), a randomized, controlled clinical trial [published correction appears in Anesthesiology.
Anesthesiology. 2018;129(3):618]. Anesthesiology. 2018;129(3):517-535.
|
| 22 |
Lynch MC, Taylor JF.
Facet joint injection for low back pain.
J Bone Joint Surg Br. 1986;68(1):138-141.
|
| 23 |
Cohen SP, Bhaskar A, Bhatia A, et al.
Consensus practice guidelines on interventions for lumbar facet joint pain from a multispecialty, international working group.
Reg Anesth Pain Med. 2020;45(6):424-467.
|
| 24 |
Kaplan M, Dreyfuss P, Halbrook B, Bogduk N.
The ability of lumbar medial branch blocks to anesthetize the zygapophysial joint.
Spine (Phila Pa 1976). 1998;23(17):1847-1852.
|
| 25 |
Ackerman WE 3rd, Ahmad M.
Pain relief with intraarticular or medial branch nerve blocks in patients with positive lumbar facet joint SPECT imaging: a 12-week outcome study.
South Med J. 2008;101(9):931-934.
|
| 26 |
Lee CH, Chung CK, Kim CH.
The efficacy of conventional radiofrequency denervation in patients with chronic low back pain originating from the facet joints: a meta-analysis of randomized controlled trials.
Spine J. 2017;17(11):1770-1780.
|