Abstract
Coronavirus disease 2019 (COVID-19) has rapidly spread globally ever since the virus was first identified in December 2019 in Wuhan, China. Despite efforts to accelerate the supply of COVID-19 vaccines worldwide, the global pandemic has continued. Polymerase chain reaction (PCR) test is currently considered the gold standard for the diagnosis of COVID-19. However, the rate of false-negative PCR for COVID-19 has been reported to be over 10%. Furthermore, an asymptomatic period can last up to 14 days following the infection. Under these circumstances, standard anesthetic practice, surgery scheduling, and approaches to appropriate management of the operating room to protect both patients and medical personnel against COVID-19 transmission need to be reviewed and appropriately modified. In this review, based on our institutional experiences along with the guidelines reported elsewhere, we propose safer and more effective perioperative management amidst the COVID-19 pandemic.
Keywords
COVID-19 pandemic, infection prevention measures, perioperative management
Introduction
Severe acute respiratory syndrome of coronavirus 2 (SARS-Co-V-2) infection, called coronavirus disease 2019 (COVID-19) pneumonia, was first identified in December 2019 in Wuhan, China1 and subsequently has spread worldwide at a rapid rate. The World Health Organization (WHO) declared COVID-19 a global pandemic on March 11, 2020.2 According to the WHO, as of June 13, 2021, there have been 175,306,598 confirmed cases of COVID-19, including 3,792,777 deaths across the globe.3 At the beginning of April 2020, the Japanese government declared the first state of emergency owing
to an abrupt surge in COVID-19 positivity rate and death cases. Furthermore, the government concurrently requested medical institutions to postpone non-urgent elective surgery to ensure availability of maximum medical resources for COVID-19 patients during the first state of emergency from April to May 2020. Since then, the declaration of the state of emergency has been repeated several times in Japan. The state of emergency in Japan is unlike European or Wuhan-style lockdown. Japan cannot legally enforce hard lockdowns owing to the feature of Japanese law. The state of emergency only allows prefectural leaders to ask residents to stay home. They can also request closures of schools, some child and senior care or community centers, and stores and businesses that are considered nonessential. Accordingly, stay-at-home-order is just a request, but it is not a legal restriction by the Government of Japan. Despite the repeated declarations of a state of emergency, COVID-19 transmission has continued to spread nationwide, and the number of newly infected cases is greater in the next wave than in the previous one. Meanwhile, the Japanese government commenced the COVID-19 vaccination for healthcare providers and elderly population over 65 years in February and June 2021, respectively. Under these circumstances, surgeries previously suspended have recently been initiated under the crucial requirement of protecting both patients and healthcare workers against COVID-19 transmission.
Exposure to respiratory droplets and aerosols increases the risk of COVID-19 transmission.4 Thus, anesthesiologists and other medical staff working in the operating room (OR) are at a higher risk of COVID-19 infection during aerosol-generating procedures, such as mask ventilation, intubation, tracheal suctioning, and extubation.5
In this review, we propose safer anesthetic practices, surgery scheduling, and management of the OR to reduce the risk of COVID-19 transmission based on our institutional experiences (Nippon Koukan Hospital, Ube-Kohsan Central Hospital, and Kawasaki Municipal Hospital). Similar guidelines reported elsewhere have also been included. The characteristics of the three hospitals are described as follows. Nippon Koukan Hospital and Ube-Kohsan Central Hospital are secondary hospitals with 350–400 beds. In contrast, Kawasaki Municipal Hospital is an advanced medical institution with over 700 beds and an emergency and critical care center. Nippon Koukan Hospital and Kawasaki Municipal Hospital are located in Kawasaki City, one of the metropolises located next to Tokyo. The population in Kawasaki is over 1,500,000. Ube-Kohsan Central Hospital is located in Ube City, a rural area in the southwestern part of Yamaguchi Prefecture at the western end of mainland Japan, with a population of approximately 160,000.
Preoperative Management
Screening for COVID-19
Following the Japanese government’s decision to lift the first state of emergency in mid-May 2020, the non-urgent elective surgeries that were postponed at our institutions have been gradually resumed since around June 2021. During the first state of emergency from April to May 2020, clusters of COVID-19 cases at medical institutions and nursing homes were frequently reported nationwide. Because of such situations, the Japanese government started making efforts to supply COVID-19 vaccines nationwide immediately. Consequently, COVID-19 vaccination for healthcare providers and the elderly population aged over 65 years was commenced in February and June 2021, respectively. All citizens aged over 12 years, except healthcare providers and the elderly population, currently receive COVID-19 vaccination. Nearly half of Japanese people have already received the second dose of COVID-19 vaccination.
The mortality rate of COVID-19 for the elderly > 80 years was 28.3% as of July 15, 2020, in Japan.6 Accordingly, screening for COVID-19 has been strengthened for all patients requiring hospitalization and surgery across the nation since around June 2020. At the beginning of June 2020, after the first state of emergency, as preoperative screening for COVID-19, we commenced preoperative questionnaires regarding respiratory infections, such as fever, dry cough, sputum, and sore throat, and the computed tomography (CT) of the chest in all surgical patients to rule out active pneumonia at our institutions.
COVID-19 can be transmitted to other individuals during an asymptomatic period of up to 14 days after infection.7 Currently, the standard polymerase chain reaction (PCR) test is regarded as the gold standard for COVID-19 diagnosis. Considering the asymptomatic period of COVID-19, the PCR test should be considered preoperative screening. However, the standard PCR test is a complicated and time-consuming procedure that requires enormous human resources. Thus, more simplified isothermal amplification technologies, such as loop-mediated amplification (LAMP), nicking enzyme-assisted reaction (NEAR), and transcription-reverse transcription concerted reaction (TRC) that can diagnose COVID-19 within 30 minutes to 1 hour are desirable in clinical settings.8 For example, Nippon Koukan Hospital, Kawasaki Municipal Hospital, and Ube-Kohsan Central Hospital employed NEAR, LAMP, and TRC techniques, respectively for preoperative screening of COVID-19. At Nippon Koukan Hospital in Kawasaki, one of the metropolises in Japan, in addition to negative findings in the chest CT scan and respiratory symptoms, the confirmation of a negative NEAR test has also been a mandatory requirement for hospitalization and surgery since the summer of 2020 as the status of COVID-19 infection has been critical, and the crisis has not been settled down in Kawasaki area yet. Meanwhile, at Ube-Kohsan Central Hospital in Ube, a rural area, where the infection status of COVID-19 has been much milder than in metropolises such as Tokyo and Kawasaki, in addition to the chest CT scan and questionnaires regarding respiratory symptoms, the TRC test is also routinely undertaken as a preoperative screening; however, this test is performed only when the rate of newly infected individuals exceeds 15/100,000 in Ube area during the preceding week. Accordingly, to conserve the limited medical resources, reconsideration of the PCR test for COVID-19 as the routine preoperative screening can be suggested, depending on the prevalence of infection in each region. Because of these simplified and less time-consuming techniques, prompt COVID-19 diagnosis is available immediately before hospitalization and surgery at our institutions. Concurrently, considering that there may be a possibility of a shortage of resources such as the test reagents when positivity drastically increases nationwide, various tests for diagnosis of COVID-19 should be available at each institution. The COVID-19 rapid antigen test is much more simplified and can deliver results in a much shorter time (within 10 minutes) for symptomatic individuals. However, this test cannot be used for asymptomatic individuals since its sensitivity heavily depends on the viral load.9
The false-negative rate of the PCR test for COVID-19 has been reported to be 13%.10 The chest CT scan can rule out COVID-19 with a high negative prediction (approximately 90%).11 Therefore, in addition to the PCR results, confirmation of negative findings of active pneumonia in the chest CT scan as well as the absence of symptoms related to respiratory infection (fever > 37.4°C, dry cough, sputum, and sore throat) should also be regarded as a preoperative screening. Considering the possibilities of the false negative results of PCR test and the asymptomatic period, such multimodal preoperative screenings are considered crucial to prevent in-hospital transmission although the chest CT scan might be an excessive examination. Furthermore, we must repeat tests in highly suspected patients with negative results. However, it may be noted that such multimodal screenings cannot detect all COVID-19 positive individuals.
Triage for Surgical Patients
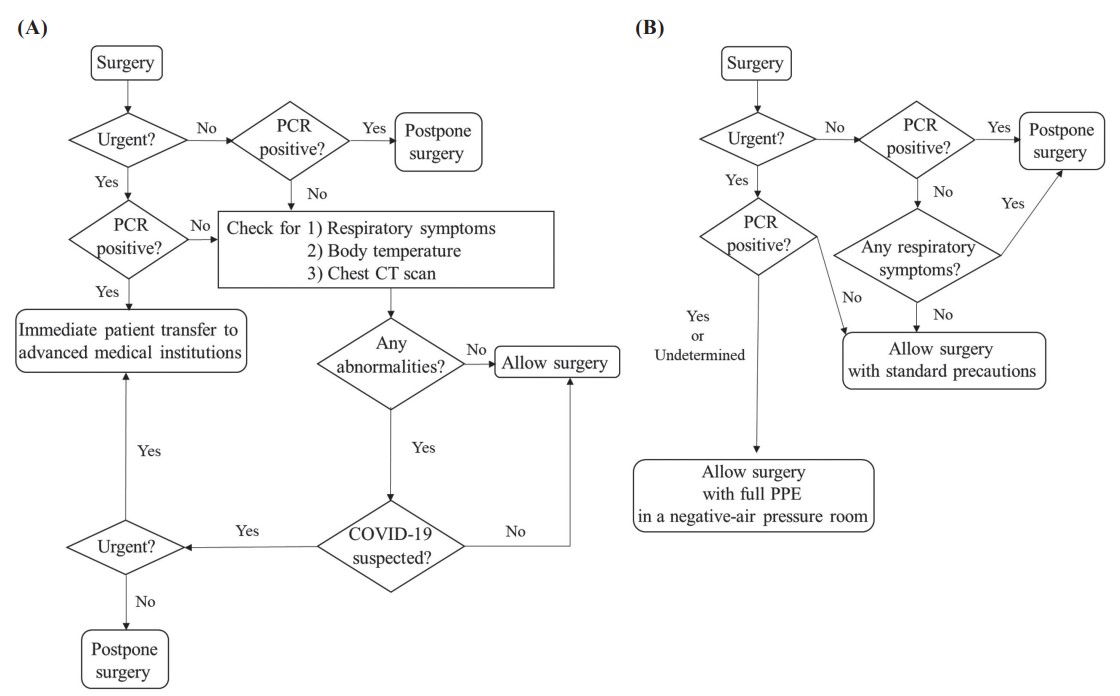
A previous study reported a mortality rate of 23.8%, and critical pulmonary complications occurred in 51.2% of patients with COVID-19 at the time of surgery.12 Therefore, for COVID-19 positive patients, irrespective of respiratory symptoms, non-urgent elective surgeries should be postponed. However, urgent surgery should be performed immediately, notwithstanding COVID-19 infection. Nippon Koukan Hospital and Ube-Kohsan Central Hospital have COVID-19 dedicated wards. However, these two secondary hospitals have neither adequate medical staff nor equipped facilities, such as the OR with negative-air-pressure rooms and the fully equipped intensive care unit, for performing surgeries on COVID-19 positive patients. It is desirable to have negative-air pressure rooms, a larger area, and adequate medical staff in the OR for appropriate management of patients with COVID-19 undergoing surgery.7,13-16 For example, it is advisable to establish dedicated donning and doffing rooms for personal protective equipment (PPE) with separated entry and exit areas in the OR to prevent infection among the OR staff.13 In addition, it is advantageous to have adequate medical staff to allow enough time for the OR staff to don and doff PPE under the supervision of an observer.13 In case of urgent surgeries of patients with COVID-19 infection, such secondary hospitals should immediately transfer the infectious patients to advanced medical institutions which are sufficiently equipped for perioperative management of COVID-19 positive patients, such as Kawasaki Municipal Hospital. Accordingly, it is crucial to ensure close communication with a few advanced medical institutions that are well equipped to accommodate COVID-19 positive patients requiring urgent surgery in each region. Depending on the local situation, each hospital should establish a strategy to offer patients optimal care with infection prevention measures during the era of COVID-19.17 A and B represent the examples of the flowchart of the triage for surgical patients during the COVID-19 pandemic at the two secondary hospitals (Nippon Koukan Hospital and Ube-Kohsan Central Hospital) and an advanced medical institution (Kawasaki Municipal Hospital), respectively (Figure 1).
Download full-size image
(A) and (B) represent the flowchart of the triage for surgical patients at the two secondary hospitals (Nippon Koukan Hospital and Ube-Kohsan Central Hospital) and an advanced medical institution (Kawasaki Municipal Hospital), respectively.
Intraoperative Management
Anesthetic Practice for COVID-19 Negative Patients
At Nippon Koukan Hospital in Kawasaki City, where COVID-19 infection status has been critical since the summer of 2020, only patients confirmed COVID-19 negative without any signs of active pneumonia on chest CT scans and any respiratory symptoms are permitted to undergo surgery in the OR. However, considering the possibility of a false-negative and the asymptomatic period of up to 14 days after infection, anesthetic practice has been modified to protect anesthesiologists and medical staff against aerosol exposure as much as possible. By referring to the protocol for intubation technique for COVID-19 suspected patients as demonstrated by Dr. Vanessa Moll of the University of Zurich18 and previous reviews,7,13,19 we established our protocols for anesthetic management as follows. The use of supraglottic airway devices should be avoided to minimize air leakage from the upper airway. Regional anesthesia without general anesthesia requiring tracheal intubation is chosen when possible. Anesthesiologists wear goggles to protect their eyes in addition to surgical masks and caps during anesthetic induction. To avoid the dissemination of aerosols caused by mask ventilation, anesthetic induction is performed with rapid sequence induction (RSI) whenever it is possible. Preoxygenation with 100% oxygen is performed under a see-through disposable plastic cover. If the RSI technique is inappropriate owing to compromised oxygen reserve, mask ventilation is performed under the plastic cover by applying a two-handed technique to minimize air leakage from the facemask. Tracheal intubation is also performed under the plastic cover by using a video laryngoscope. During the extubation procedure, the see-through plastic cover is also fully placed on the patient’s head. The plastic covers are changed for each procedure. After extubation, oxygen supply via the nasal prong is commenced. After the patients’ respiratory condition is confirmed stable, a surgical mask is placed on the patient’s face, and the plastic cover is then removed. During the procedures of intubation and extubation, the air conditioning system is turned off in each OR to suppress airflow.
Anesthetic Practice and Scheduling Surgery for COVID-19 Positive Patients
At Kawasaki Municipal Hospital, confirmed or highly suspected COVID-19 positive patients are allowed to undergo only urgent surgeries in the OR. In addition to standard precautions for COVID-19 negative patients described above, critical measures for intraoperative management of COVID-19 positive patients in the OR are as follows. First, surgery must be performed in a negative-air-pressure OR.14,15,20 We set the assigned OR to negative air pressure before the patient’s arrival, and the entrance of the negative-air-pressure room is altered to manual mode to avoid inadvertent door opening. It is also necessary to prepare all the devices and tools for surgery and anesthesia in the assigned OR before the patient’s arrival to prevent infection among the medical staff.14 Patients can enter the OR while wearing a surgical mask and must be authenticated inside the assigned OR. While the patient is in the OR, any unauthorized staff is strictly prohibited from accessing the room. Second, all the involved medical staff must strictly don full PPE, such as an N95 mask, eye guard, long sleeve plastic apron, and double gloves throughout the surgery.15,21 Regional anesthesia is chosen over general anesthesia whenever it is possible because it significantly reduces the need for aerosol-generating procedures.22-25 Under regional anesthesia with spontaneous breathing, the patient must wear a surgical mask throughout the surgery. When general anesthesia is required, tracheal intubation is performed by using the RSI technique to avoid exposure to aerosols. The patient must continue to wear a surgical mask until anesthesia induction. Tracheal suction is performed by using a closed suction device or avoided if possible. After extubation, the tracheal tube is immediately discarded and placed in a sealed bag. The involved staff must doff the PPE inside the OR after the patient is discharged from the OR to prevent the medical staff from getting infected.
The patient should not be extubated if there is any health-related concern, especially regarding the respiratory status at the end of surgery. While the intubated patient is transferred, the breathing circuit filter should be attached to the tracheal tube directly, so the patient’s airway does not get exposed to the open air while the respiratory circuit is getting disconnected.14 After the patient is discharged from the OR, the OR is disinfected for 20 minutes by using xenon irradiation. Following disinfection, negative air pressure may be released. During the unavailability of xenon, the room must be ventilated under negative pressure for at least 1 hour.
The medical staff with full PPE in the isolated OR must be mentally and physically exhausted; therefore, only expert practitioners should be involved to avoid undesirable events and ensure smooth execution of procedures.26
Planned surgery should not be considered during the period in which the patients may be infectious: at least 10 days for mildly to moderately ill patients and 15–20 days for severely ill patients until the symptoms subside totally.27 Elective surgery should not be scheduled within 7 weeks after the diagnosis of COVID-19 infection.27
Postoperative Management
COVID-19 Negative Patients
As a normal practice in Japan, medical institutions allow no visitors to enter the ward to minimize the risk of COVID-19 transmission in hospitalized patients. However, the possibility of a patient’s contact with the medical staff during an asymptomatic period cannot be ruled out. To prevent the surge of COVID-19 cases in the ward, medical staff need to do as follows. First, the patient’s health condition should be monitored and followed-up in detail during hospitalization. In case of any clinical symptoms such as fever, dry cough, and difficulty in breathing, further medical tests should be performed immediately. Early diagnosis and treatment of COVID-19 and immediate quarantine are crucial in postsurgical patients. Second, medical staff should regularly check their health conditions as well. Third, medical staff should always wear a surgical mask in a hospital and maintain hand hygiene when donning and doffing gloves for each medical procedure.20,21 The Centers for Disease Control and Prevention (CDC) recommend using alcohol-based hand rub with 60%–95% alcohol for hand hygiene in healthcare settings.28
COVID-19 Positive Patients
In addition to the strategies toward managing COVID-19 negative patients as described above, zoning is mandatory for positive patients. At Kawasaki Municipal Hospital, the dedicated ward for positive patients is strictly isolated from the general wards. Accordingly, the postoperative care of positive patients is strictly restricted to the COVID-19 dedicated ward. Shifting positive patients is conducted by minimum staff, stringently separated from other patients and medical staff. Once confirmed to be positive in the general ward, the patient is immediately transferred to the COVID-19 dedicated ward. Patients previously diagnosed as positive are allowed to enter a general ward after being tested negative twice by the LAMP test.
Concerns for Vaccination and Surgery Scheduling
The COVID-19 vaccine may cause some systemic events, such as fever and chills, within 1–2 days after vaccination. In most cases, these symptoms persist for a short duration, and all symptoms resolve within a week. Though side effects are uncommon after the first dose, approximately 15% of cases experience them after the second dose.29 Considering the possibility of the side effects caused by the vaccines, the Royal College of Surgeons of England has proposed recommendations toward scheduling vaccination and surgery as follows.29 First, an urgent surgery should be performed, irrespective of the vaccination status. Second, for non-urgent elective surgery, the date of surgery should be separated from that of vaccination by a few days (at most one week) to ensure that any symptom such as fever, chills, and general fatigue can be appropriately attributed to the consequences of either vaccination or the surgery itself. Furthermore, CDC have announced that people can be considered fully vaccinated 2 weeks after their second dose in a 2-dose series, such as the Pfizer or Moderna vaccines.30 Accordingly, it can be recommended that non-urgent elective surgeries take place at least 2 weeks after the second dose of vaccination.
Conclusions
Amidst the global COVID-19 pandemic, OR management needs to be appropriately modified to minimize the risk of virus transmission. Multimodal preoperative screenings for COVID-19 are crucial to prevent in-hospital transmission. Considering the possibility of a false-negative PCR test and an asymptomatic period, anesthesiologists should take appropriate measures to avoid exposure to aerosols during the anesthetic procedure even if the patient is COVID-19 negative. In COVID-19 positive patients, only urgent surgeries can be allowed under the supervision of expert practitioners with full-PPE in the OR that can be set to negative air pressure.
Regarding the scheduling of surgeries after vaccination, urgent surgeries should immediately be performed, irrespective of vaccination status. However, non-urgent elective surgeries should be planned at least 2 weeks after the second dose vaccination, considering the acquired immune effect and the adverse events after vaccination.
Conflict of Interest
The authors declare no conflict of interest.
Funding
None.
References
| 1 |
Wang D, Hu B, Hu C, et al.
Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China.
JAMA. 2020;323(11):1061-1069.
|
| 2 | |
| 3 |
WHO coronavirus (COVID-19) dashboard.
World Health Organization.
https://covid19.who.int/.. Accessed June 14, 2021.
|
| 4 |
Chan JFW, Yuan S, Kok KH, et al.
A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster.
Lancet. 2020;395(10223):514-523.
|
| 5 |
Hirota K.
Air contamination with SARS-CoV-2 in the operating room.
J Anesth. 2021;35(3):333-336.
|
| 6 |
Situation of COVID-19 in Japan.
Japan Health, Labour and Welfare Ministry.
https://www.mhlw.go.jp/content/10906000/000649533.pdf.. Accessed June 15, 2021.
|
| 7 |
Erbabacan E, Özdilek A, Beyoğlu ÇA, Altındaş F.
Perioperative anaesthetic management of confirmed or suspected COVID-19 patients.
Turk J Anaesthesiol Reanim. 2020;48(3):180-187.
|
| 8 |
James AS, Alawneh JI.
COVID-19 infection diagnosis: potential impact of isothermal amplification technology to reduce community transmission of SARS-CoV-2.
Diagnostics (Basel). 2020;10(6):399.
|
| 9 |
Hanson KE, Altayar O, Caliendo AM, et al.
The infectious diseases society of America guidelines on the diagnosis of COVID-19: antigen testing.
Clin Infect Dis. 2021;ciab557.
|
| 10 |
Arevalo-Rodriguez I, Buitrago-Garcia D, Simancas-Racines D, et al.
False-negative results of initial RT-PCR assays for COVID-19: a systematic review.
PLoS One. 2020;15(12):e0242958.
|
| 11 |
Suehiro K.
Preoperative assessment for scheduling surgery during the coronavirus disease pandemic.
J Anesth. 2021;35(3):378-383.
|
| 12 |
COVIDSurg Collaborative.
Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study.
Lancet. 2020;396(10243):27-38.
|
| 13 |
Malhotra N, Bajwa SJS, Joshi M, Mehdiratta L, Trikha A.
COVID operation theatre—advisory and position statement of Indian Society of Anaesthesiologists (ISA National).
Indian J Anaesth. 2020;64(5):355-362.
|
| 14 |
Chow TT, Yang XY.
Ventilation performance in operating theatres against airborne infection: review of research activities and practical guidance.
J Hosp Infect. 2004;56(2):85-92.
|
| 15 |
Ti LK, Ang LS, Foong TW, Ng BSW.
What we do when a COVID-19 patient needs an operation: operating room preparation and guidance.
Can J Anaesth. 2020;67(6):756-758.
|
| 16 |
Obara S.
Anesthesiologist behavior and anesthesia machine use in the operating room during the COVID-19 pandemic: awareness and changes to cope with the risk of infection transmission.
J Anesth. 2021;35(3):351-355.
|
| 17 |
Wong J, Goh QY, Tan Z, et al.
Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore.
Can J Anaesth. 2020;67(6):732-745.
|
| 18 |
InterAnest.
Intubation of suspected COVID-19 patients (English).
https://www.youtube.com/watch?v=iIGAmdyZr4Y&t=60s.. Published March 22, 2020. Accessed June 17, 2021.
|
| 19 |
Al Harbi MK, Abdulmomen A, Qurashi FA, Kattan M, Ahmad AE, Eldawlatly A.
Airway management and COVID-19 patient—Saudi Anesthesia Society guidelines.
Saudi J Anaesth. 2020;14(3):387-389.
|
| 20 |
Bowdle A, Jelacic S, Shishido S, Munoz-Price LS.
Infection prevention precautions for routine anesthesia care during the SARS-CoV-2 pandemic.
Anesth Analg. 2020;131(5):1342-1354.
|
| 21 |
Rush University System for Health.
Personal protective equipment for COVID-19 care.
https://www.youtube.com/watch?v=84CydmuHXD8.. Published March 22, 2020. Accessed June 19, 2021.
|
| 22 |
Murata H, Vanegas C, Ogami-Takamura K.
Ultrasound-guided regional anesthesia in COVID-19 and future pandemics: infection control.
Curr Opin Anaesthesiol. 2021;34(5):648-653.
|
| 23 |
Hotta K.
Regional anesthesia in the time of COVID-19: a minireview.
J Anesth. 2021;35(3):341-344.
|
| 24 |
Heijnen T, Vandebergh V, Vandepitte C, Buck R.
Regional anesthesia in coronavirus disease 2019 pandemic.
Curr Opin Anaesthesiol. 2021;34(5):609-615.
|
| 25 |
Uppal V, Sondekoppam RV, Landau R, El-Boghdadly K, Narouze S, Kalagara HKP.
Neuraxial anaesthesia and peripheral nerve blocks during the COVID-19 pandemic: a literature review and practice recommendations.
Anaesthesia. 2020;75(10):1350-1363.
|
| 26 |
Anesthetic management and endotracheal intubation of patients with or suspected of COVID-19.
Japanese Society of Anesthesia HP.
https://anesth.or.jp/img/upload/news/cb72269d596637cba065542e74178803.pdf.. Accessed July 6, 2021.
|
| 27 |
El-Boghdadly K, Cook TM, Goodacre T, et al.
SARS-CoV-2 infection, COVID-19 and timing of elective surgery: a multidisciplinary consensus statement on behalf of the Association of Anaesthetists, the Centre for Peri-operative Care, the Federation of Surgical Specialty Associations, the Royal College of Anaesthetists and the Royal College of Surgeons of England.
Anaesthesia. 2021;76(7):940-946.
|
| 28 |
Hand hygiene recommendations.
Guidance for healthcare providers about hand hygiene and COVID-19.
https://www.cdc.gov/coronavirus/2019-ncov/hcp/hand-hygiene.html.. Updated May 17, 2020. Accessed June 18, 2021.
|
| 29 |
Vaccinated patients guidance.
Royal College of Surgeons of England.
https://www.rcseng.ac.uk/coronavirus/vaccinated-patients-guidance/.. Published January 22, 2021. Accessed June 18, 2021.
|
| 30 |
When you’ve been fully vaccinated.
Centers for Disease Control and Prevention.
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated_archived.html.. Updated October 15, 2021. Accessed January 23, 2022.
|