Abstract
Background
Hemodynamic changes are the most common predicted response after laryngoscopy and intubation during general anesthesia. We compared the efficacy of buprenorphine with fentanyl to attenuate this stress response.
Methods
One hundred and thirty patients of either sex between the age group of 18–70 years, admitted for the routine surgical procedure under general anesthesia were enrolled in this double blind, randomized, clinical study. Patients were randomly assigned into two equal groups (60 patients in each group): group F received fentanyl 2 µg/kg, and group B received buprenorphine 2.5 µg/kg; both via intravenous route. Each group received a total volume of 10 mL by adding normal saline to the total drug volume, given over 60 seconds, 5 minutes before intubation. Thereafter patients were induced using routine balanced anesthesia technique, and the hemodynamic parameters were observed at baseline (0 minute), 1, 3, and 5 minutes after the administration of the study drug and again at 1, 3, 5, 7, and 10 minutes after intubation. Continuous variables were presented as mean with an 80% confidence interval, and a
Results
In both groups, mean arterial blood pressure (MAP) and heart rate (HR) were statistically insignificant up to 5 minutes after study drug, thereafter mean HR and MAP at 1, 3, 5, 7, and 10 minutes after intubation, were statistically significant between the two groups, and
Conclusions
The dose of 2.5 µg/kg buprenorphine is an effective alternative to fentanyl 2 µg/kg for attenuating the hemodynamic response accompanying laryngoscopy and tracheal intubation without causing any hemodynamic adverse effect.
Keywords
buprenorphine, endotracheal intubation, fentanyl, hemodynamic changes, laryngoscopy
Introduction
Hemodynamic changes are the most common predicted response after laryngoscopy and intubation even in normotensive patients but are well tolerated. These stress responses like tachycardia and hypertension might have deleterious effects on patients with pre-existing cardiovascular or cerebrovascular conditions and can lead to fatal arrhythmias, myocardial infarction, and intracerebral bleeding.1,2
Various prophylactic pharmacological interventions have been tried to blunt stress response, like the administration of short-acting beta-blockers, intravenous (IV) lignocaine, calcium channel blockers, vasodilators, magnesium sulphate, alpha 2 [α-2] adrenergic agonists, propofol, and opoids.3
In the recent past, fentanyl is the most common drug being used for attenuating the pressure response after intubation. Although fentanyl has numerous advantages, it has its own limitations, such as nausea, vomiting, respiratory depression, and poor availability owing to the strict narcotic laws. Therefore, there was a continuous effort to find out drugs that provide better attenuation of pressure response after intubation, have fewer side effects, and are easy to be available in most parts of a developing country like India.
Buprenorphine is one of the semisynthetic opioids that has the effects of both weak partial mu-opioid receptor agonist and weak kappa-opioid receptor antagonist and is used for the treatment of severe pain.4,5 It has less effect on Qtc interval prolongation,6,7 fewer drug interactions,8,9 improved safety profile with a lower risk of overdose and respiratory depression.10-12
Review of literature shows that the studies on the use of buprenorphine to attenuate the hemodynamic changes after laryngoscopy and intubation are scarce. Hence, we designed this study to compare the efficacy of fentanyl and buprenorphine to blunt stress response after laryngoscopy and intubation.
Methods
After the approval of institutional ethical committee and informed written consent, 130 patients of either sex, in the age group of 18–70 years, with American Society of Anesthesiologists (ASA) physical status I or II, and scheduled for elective surgeries under general anesthesia were enrolled during the study period from April 2018 to September 2019. This double blind, randomized-controlled trial was registered with Clinical Trial Registry–India (CTRI/2018/04/013180). The exclusion criteria included ASA physical status III and IV, full stomach, pregnancy, emergency surgery, protocol violation by participants, and laryngoscopy lasting more than 25 seconds.
All patients were randomly assigned into two equal groups (n = 60) using sequentially numbered, opaque, sealed envelope based on computer-generated random numbers. Group F received fentanyl 2 µg/kg,
and group B received buprenorphine 2.5 µg/kg prepared as 10 mL solution by adding normal saline to the drug volume, given over 60 seconds. The study drugs were prepared by an independent anesthesiologist not associated with the study. Both patients and the attending anesthesiologist were unaware of the group allocation.
Patients were evaluated on the day before surgery by an anesthesiologist and premedicated with alprazolam 0.5 mg and ranitidine 150 mg orally on the night before surgery. All patients received injection glycopyrrolate 0.2 mg intramuscular 30 minutes before the induction of general anesthesia. On arrival into the operating room, standard monitors were placed and baseline parameters were recorded in the form of heart rate (HR), mean arterial blood pressure (MAP), and oxygen saturation. After we secured peripheral 18 G IV catheter on the ventral aspect of the left forearm, the study drug was injected slowly over 1 minute and 5 minutes before the intubation. Patients were induced with propofol IV in a dose of 2 mg/kg body weight over 30 seconds, followed by vecuronium 0.1 mg/kg IV. After 3 minutes of bag and mask ventilation, tracheal intubation was performed with an appropriately sized cuffed tracheal tube. All the intubation was performed by an experienced anesthesiologist who had an experience of performing at least 60 intubation per month. Anesthesia was maintained with controlled ventilation on a mixture of O2 : N2O (33% : 66%), isoflurane, and intermittent injections of vecuronium 0.01 mg/kg repeatedly every 20 minutes. Surgical stimulation was not allowed for 10 minutes after intubation. After meeting the extubation criteria, patients with residual neuromuscular weakness were reversed with injection glycopyrrolate 10 µg/kg IV and injection neostigmine 50 µg/kg IV at the end of surgery and shifted to postanesthesia care unit for further vital monitoring.
Vital parameters like HR and MAP were observed at 0 (basal value), 1, 3, and 5 minutes after study drug and again at 1, 3, 5, 7, 10 minutes after intubation and cuff inflation. Our study was terminated after 10 minutes of study, but all essential vital parameters were monitored till the end of surgery. Hypertension, defined as an increase of blood pressure (BP) by more than 20% from baseline, was treated with incremental IV infusion doses of nitro-glycerine 5 mg/min. Tachycardia, defined as an increase of HR by more than 20% from baseline, was treated with an incremental IV doses of esmolol 0.5 mg/kg body weight. Bradycardia, defined as HR < 50 beats per minute, was treated with IV atropine 0.3–0.6 mg. Patients were observed for any adverse effects like nausea, vomiting, arrhythmia, bradycardia, shivering, pruritus, respiratory depression, and sedation.
We estimated our sample size and regarded mean BP as the most important hemodynamic parameters. We assumed a difference of 5 units in attenuating the mean BP between F and B groups as clinically significant at 1 minute’s post-intubation. To achieve a power of 80% and a level of significance of 5% (two-sided), the desired sample size was calculated as 65 cases in each group to detect a difference of 5 units in MAP between F and B groups. Finally, 60 cases were recruited in each group for this study considering the probability of any dropouts.
Statistical testing was conducted with the statistical package for the social science system version SPSS 17.0 (SPSS Inc, Chicago, IL, USA). Continuous variables are presented as mean ± standard deviation, and categorical variables are presented as absolute numbers and percentages. Nominal categorical data between the groups were compared by using chi-square test or Fisher’s exact test as appropriate.
Primary outcome measures were the efficacy of buprenorphine compared with fentanyl to attenuate the hemodynamic stress response (MAP and HR) accompanying laryngoscopy and intubation. A secondary outcome was to look for any adverse effects of these interventions.
Results
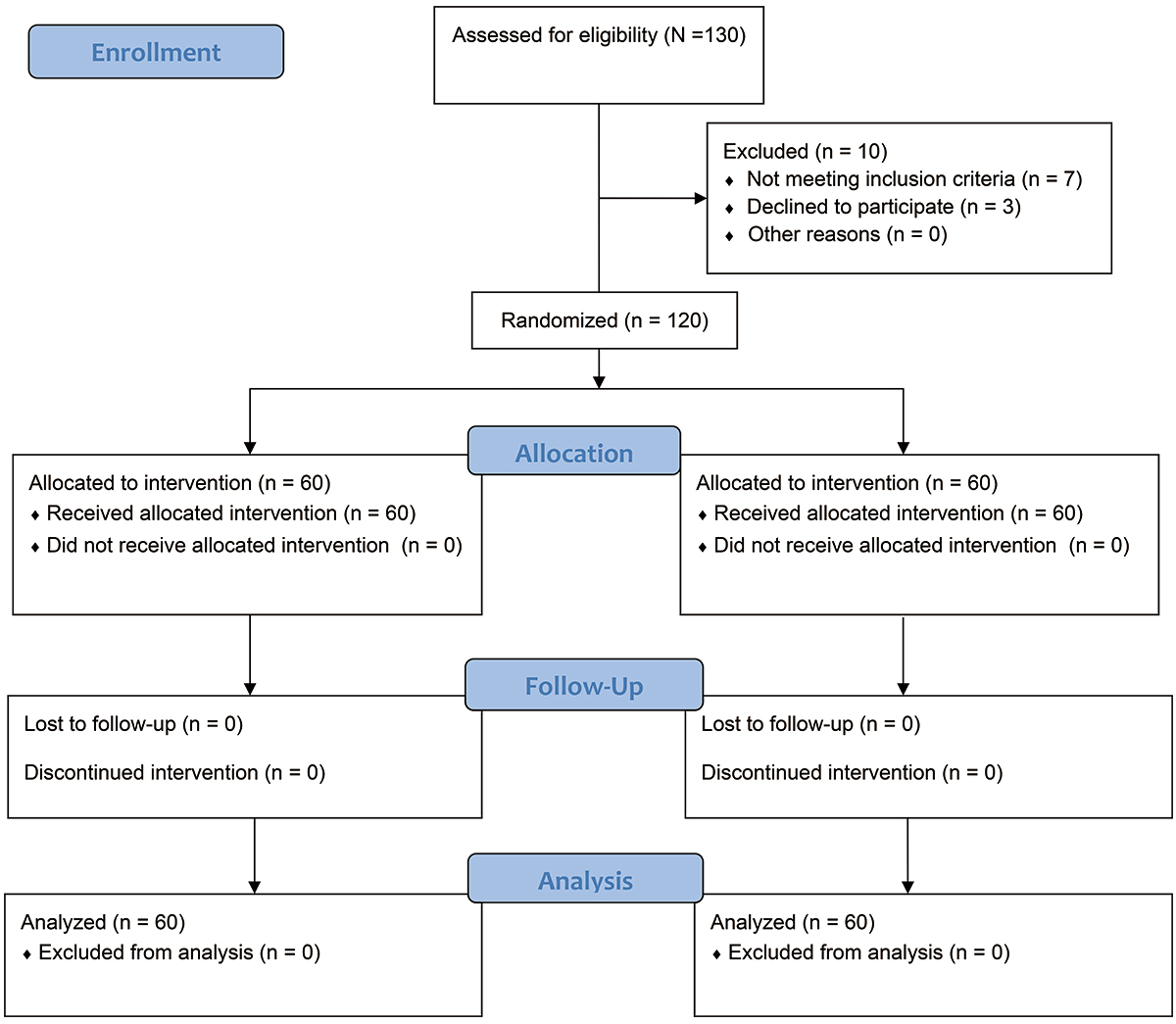
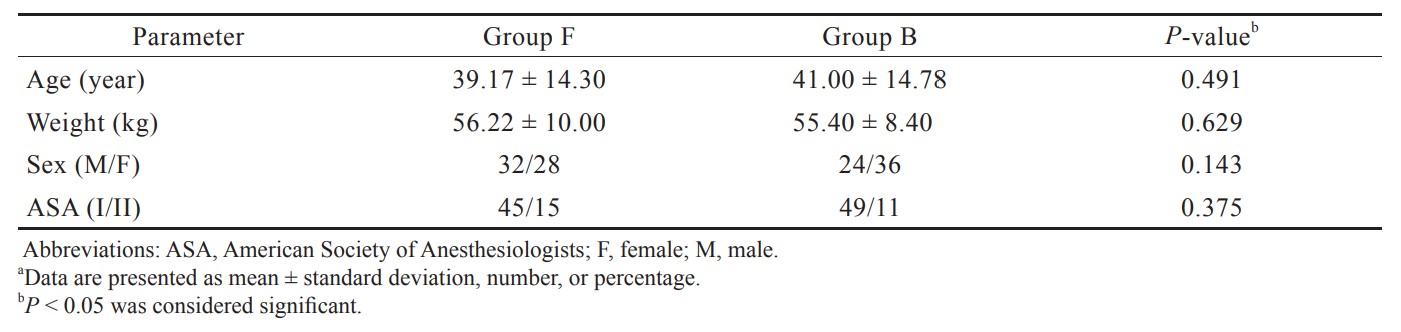
Figure 1 shows a CONSORT flow diagram of patients of the study. Out of 130 patients, 120 completed the study successfully. Both groups were comparable with respect to age, sex, weight, and ASA classification (Table 1). On intergroup comparison, there was a decrease in mean HR till 5 minutes in group F, and a continuous increase in mean HR in group B till 5 minutes after the study drug was given, and was found to be statistically insignificant (
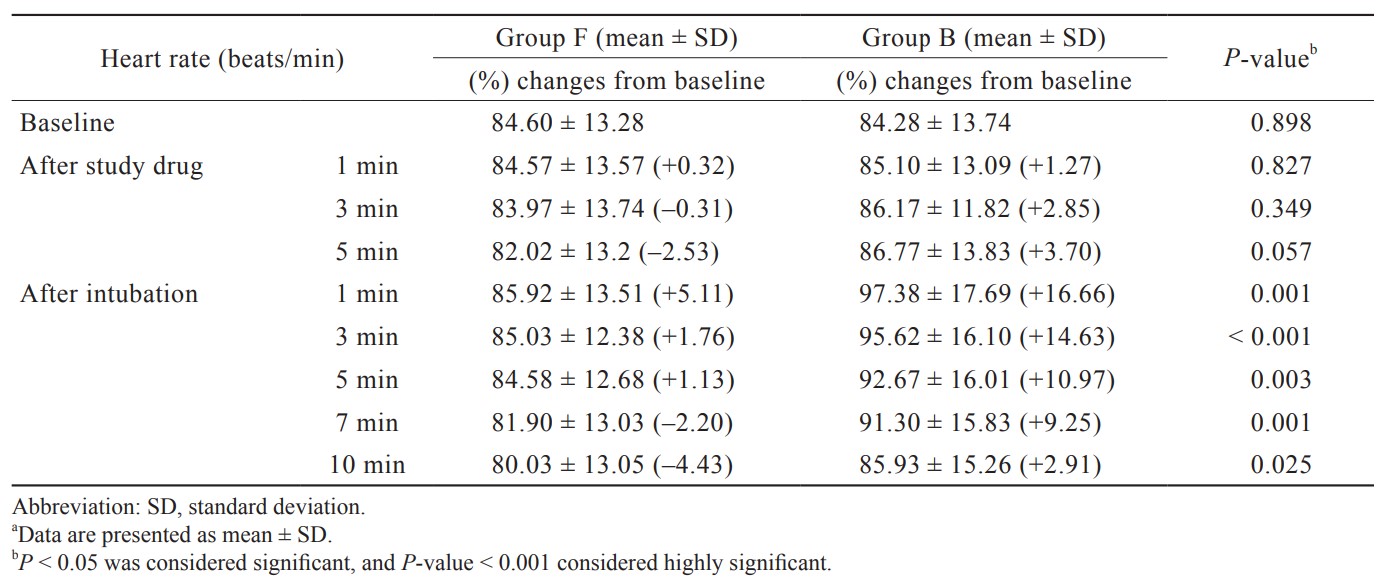
On comparison of MAP (Table 3), in group F, there was a decrease of MAP till 5 minutes after the study drug was given and the maximum rise of MAP 1 minute after intubation was 99.57 ± 14.70 (mmHg). Thereafter, MAP started to decrease and returned nearer to baseline at 5 minutes and remained below the baseline till the end of 10 minutes. In group B, there was a decrease in MAP till 5 minutes after the study drug was given, and the maximum rise observed at 1–minute post-intubation was 105.45 ± 14.63 (mmHg); thereafter, MAP started to decrease till the end of 10 minutes and remained above the baseline MAP.
Download full-size image
Download full-size image
Download full-size image
Download full-size image
On intergroup comparison, these changes were statistically insignificant (
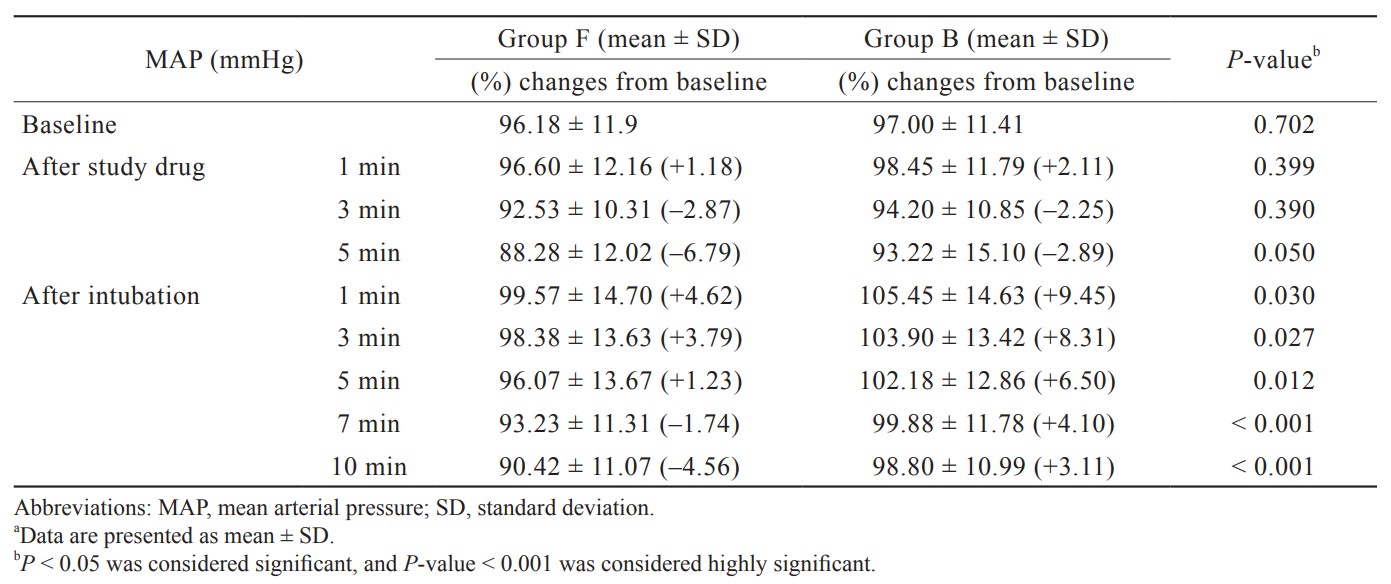
In group F, 2 patients had transient episodes of bradycardia, and in group B, 2 patients had episodes of transient ventricular premature contraction after intubation. None of these patients required pharmacological intervention and was hemodynamic stable (Table 4).
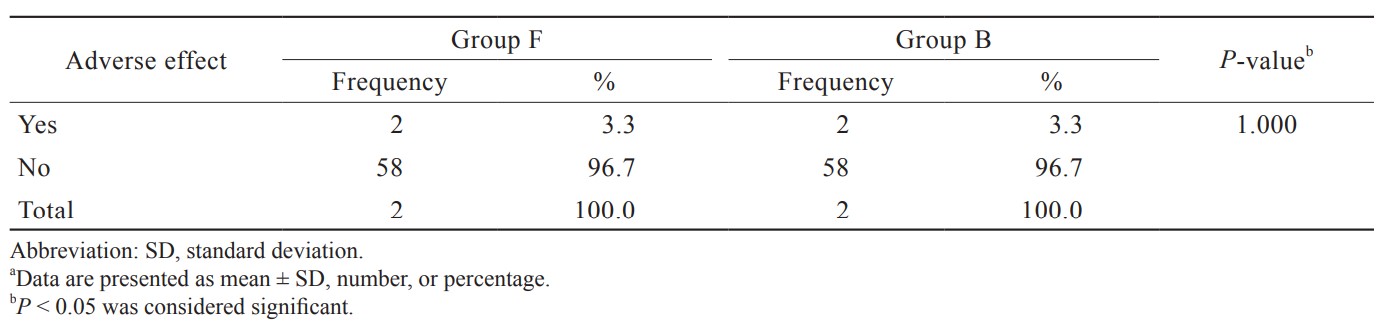
Download full-size image
Discussion
Laryngoscopy and endotracheal intubation are usually associated with the pressor response that leads to transient hemodynamic changes in the form of an increase in HR and BP, which can be fatal to patients with pre-existing cardiovascular or cerebrovascular conditions. Studies have shown that narcotics such as fentanyl13 and buprenorphine14 are effective in blunting pressor response to laryngoscopy and endotracheal intubation. We observed in our study that buprenorphine was effective in partially attenuating stress response accompanying laryngoscopy and intubation but not completely obliterating stress response like fentanyl.
In this present study, on comparison of mean HR between the two groups, mean HR was statistically non-significant (
on hemodynamic response during oro-tracheal and fiberoptic intubation, concluded that the administration of fentanyl suppresses the hemodynamic responses to endotracheal intubation more than it does to laryngoscopy. There was no significant difference in the hemodynamic responses to orotracheal intubation by fiberscopy and laryngoscopy without fentanyl pre-treatment, whereas 2 μg/kg fentanyl significantly reduced the hemodynamic responses in the group intubated by fiberscopy.
In contrast to our study, Sharma and Parikh21 did not find any statistically significant differences of HR and BP between fentanyl and nalbuphine at any point of time interval (
The best possible mechanism of action of fentanyl and buprenorphine to attenuate the hemodynamic response to intubation can be explained by strong and selective µ receptor agonistic action of fentanyl and partial µ receptor agonist, delta receptor agonist, and kappa receptor antagonistic action of buprenorphine. In group F, initial fall of HR and BP is caused by its strong and predominant µ receptor agonistic action, and maximum rise of HR and BP after intubation is due to sympathoadrenal stimulation.22 Thereafter early fall of all hemodynamic parameters to its baseline value is due to its pure µ agonist action and is known to cause a decrease in BP, HR, systemic vascular resistance (SVR), plasma catecholamine level, and cardiac afterload. In group B, initial slow rise of all hemodynamic parameters is caused by its partial µ receptor agonist. Its ability to cause an increase in HR, BP, plasma catecholamine level, SVR, and delayed fall of all hemodynamic parameters to its baseline value may be due to its physiological action to increase cardiac afterload and depress myocardial contractility.
Conclusions
The dose of 2.5 µg/kg IV buprenorphine is an effective alternative to fentanyl 2 µg/kg IV for attenuating the hemodynamic response accompanying laryngoscopy and tracheal intubation without causing any hemodynamic adverse effect.
However, there are some limitations to the study. All the patients included in the study were ASA physical status I and II, and therefore, caution must be exerted while one generalizes the results to ASA physical status III and IV patients. We could not quantify the plasma level of catecholamine at our centre, which could have shown more accurate attenuation. Further clinical trials are needed in a larger population to externally validate our study.
References
| 1 |
Edwards ND, Alford AM, Dobson PM, Peacock JE, Reilly CS.
Myocardial ischaemia during tracheal intubation and extubation.
Br J Anaesth. 1994;73(4):537-539.
|
| 2 |
Fox EJ, Sklar GS, Hill CH, Villanueva R, King BD.
Complications related to the pressor response to endotracheal intubation.
Anesthesiology. 1977;47(6):524-525.
|
| 3 |
Kay B, Healy TE, Bolder PM.
Blocking the circulatory responses to tracheal intubation.
Anaesthesia. 1985;40:960-963.
|
| 4 |
Lutfy K, Eitan S, Bryant CD, et al.
Buprenorphine-induced antinociception is mediated by mu-opioid receptors and compromised by concomitant activation of opioid receptor-like receptors.
J Neurosci. 2003;23(32):10331-10337.
|
| 5 |
Lutfy K, Cowan A.
Buprenorphine: a unique drug with complex pharmacology.
Curr Neuropharmacol. 2004;2(4):395-402.
|
| 6 |
Wedam EF, Bigelow GE, Johnson RE, Nuzzo PA, Haigney MCP.
QT-interval effects of methadone, levomethadyl, and buprenorphine in a randomized trial.
Arch Intern Med. 2007;167(22):2469-2475.
|
| 7 |
Anchersen K, Clausen T, Gossop M, Hansteen V, Waal H.
Prevalence and clinical relevance of corrected QT interval prolongation during methadone and buprenorphine treatment: a mortality assessment study.
Addiction. 2009;104(6):993-999.
|
| 8 |
Obadia Y, Perrin V, Feroni I, Vlahov D, Moatti JP.
Injecting misuse of buprenorphine among French drug users.
Addiction. 2001;96(2):267-272.
|
| 9 |
Reynaud M, Petit G, Potard D, Courty P.
Six deaths linked to concomitant use of buprenorphine and benzodiazepines.
Addiction. 1998;93(9):1385-1392.
|
| 10 |
Bruneau J, Ahamad K, Goyer MÈ, et al.
Management of opioid use disorders: a national clinical practice guideline.
CMAJ. 2018;190(9):E247-E257.
|
| 11 |
Luty J, O’Gara C, Sessay M.
Is methadone too dangerous for opiate addiction?
BMJ. 2005;331(7529):1352-1353.
|
| 12 |
Marteau D, McDonald R, Patel K.
The relative risk of fatal poisoning by methadone or buprenorphine within the wider population of England and Wales.
BMJ Open. 2015;5(5):e007629.
|
| 13 |
Bennett GM, Stanley TH.
Human cardiovascular responses to endotracheal intubation during morphine—N2O and fentanyl—N20 anesthesia.
Anesthesiology. 1980;52(6):520-522.
|
| 14 |
Khan FA, Kamal RS.
Effect of buprenorphine on the cardiovascular response to tracheal intubation.
Anaesthesia. 1989;44(5):394-397.
|
| 15 |
Thippeswamy RR, Shetty SR.
Intravenous low dose fentanyl versus lignocaine in attenuating the hemodynamic responses during endotracheal intubation: a randomized double blind study.
Anesth Essays Res. 2018;12(4):778-785.
|
| 16 |
Kothari D, Sharma CK.
Effect of nalbuphine and pentazocine on attenuation of hemodynamic changes during laryngoscopy and endotracheal intubation: a clinical study.
Anesth Essays Res. 2013;7(3):326-330.
|
| 17 |
Khanday SB, Mir AH, Sofi KP, Lone AQ, Shah AN.
Evaluation and comparison of fentanyl versus nalbuphine for attenuation of hemodynamic response to laryngoscopy and endotracheal intubation in general anesthesia.
Anesth Essays Res. 2019;13(1):111-118.
|
| 18 |
Ahsan-ul-Haq M, Kazmi EH, Rao ZA.
Nalbuphine prevents haemodynamic response to endotracheal intubation.
J Coll Physicians Surg Pak. 2005;15(11):668-670.
|
| 19 |
Adachi Y, Takamatsu I, Harada M, et al.
The effects of low-doses of fentanyl, buprenorphine and pentazocine on circulatory responses to endotracheal intubation.
Masui. 1998;47(12):1478-1481.
|
| 20 |
Adachi YU, Satomoto M, Higuchi H, Watanabe K.
Fentanyl attenuates the hemodynamic response to endotracheal intubation more than the response to laryngoscopy.
Anesth Analg. 2002;95(1):233-237.
|
| 21 |
Sharma N, Parikh H.
A comparative study of hemodynamic responses to intubation: fentanyl versus nalbuphine.
Gujarat Med J. 2014;69(2):48-53.
|
| 22 |
Singh M.
Stress response and anaesthesia altering the peri and post-operative management.
Indian J Anaesth. 2003;47(6):427-434.
|