Abstract
Background
The hemodynamic consequences of sympathetic blockade under spinal anesthesia remains a major concern especially in elderly frail patients. The baricity of the injected solution remains the principal factor controlling the diffusion of spinal anesthetics and the resulting sympathetic blockade. In this study, the sequential administration of isobaric and hyperbaric bupivacaine (HB) is evaluated regarding the incidence of hypotension during orthogeriatric surgery.
Methods
Fifty elderly patients (age > 60), scheduled for lower limb orthopedic surgery were randomly divided into two groups. In group HIB (n = 25), sequential injection of two syringes, 1.5 mL of 0.5% HB with 15 µ of fentanyl was injected, followed immediately by 1.5 mL of 0.5% isobaric bupivacaine, and in group HB (n = 25), 3 mL of 0.5% HB mixed with 15 µ of fentanyl citrate (0.3 mL of fentanyl 50 µg/mL) were used for spinal anesthesia.
Results
No statistical difference was found between the two groups regarding patient demographics, comorbidities, or preoperative laboratory data. The absolute incidence of hypotension (16% vs. 44%,
Conclusions
Our results show a better hemodynamic profile of the sequentially injected mixture with a lower incidence of intraoperative hypotension and subsequent lower vasopressor requirements.
Keywords
baricity, elderly, hypotension, orthogeriatric, sequential, spinal
Introduction
Orthopedic surgeries in geriatrics carry a significant risk of both morbidity and mortality,1 and rapid surgical intervention is warranted to reduce the incidence of complications and fasten the hospital discharge.2,3 Despite the debate regarding the preferred type of anesthesia in the elderly population, spinal anesthesia has shown the advantage of the simplicity of the technique, the better analgesic profile, and the lower incidence of thromboembolic events. However, the hemodynamic consequences of sympathetic blockade under spinal anesthesia remains a major concern especially in frail patients.4,5
Many modifications of the spinal anesthesia technique in the elderly population were used to avoid complications like hypotension, bradycardia, cerebral hypoperfusion, and higher block levels. These techniques included unilateral spinal techniques or lowering the dose of local anesthetics (LA).6-8 Yet, if the patient position and the LA dose are fixed, the principal factor controlling the intrathecal diffusion of injected anesthetic medications and the resulting sympathetic blockade would be the baricity injected solution. While the hyperbaric solutions spread is mainly controlled by gravity, the isobaric LA solutions have a limited spread in the cerebrospinal fluid (CSF), especially in small doses.9-11 In this study, we studied the sequential administration of a low dose of isobaric and hyperbaric bupivacaine (HB) in geriatric patients undergoing orthopedic surgery. This sequence of injection is assumed to avoid the disadvantages of hyperbaric and isobaric LA solutions while maintaining the privileges of both. The low dose HB achieves less dense anesthesia at lower dermatomal levels while the sequential low dose plain bupivacaine would secure sufficient segmental anesthesia for the surgical procedure, sparing the sympathetic system integrity and maintaining hemodynamic stability. The primary outcome was the incidence of arterial hypotension in elderly patients after spinal anesthesia, and secondary outcomes included the use of vasopressors, spinal block characteristics, and perioperative complications, including nausea, vomiting, shivering, pruritus, respiratory depression, shivering, and delirium.
Methods
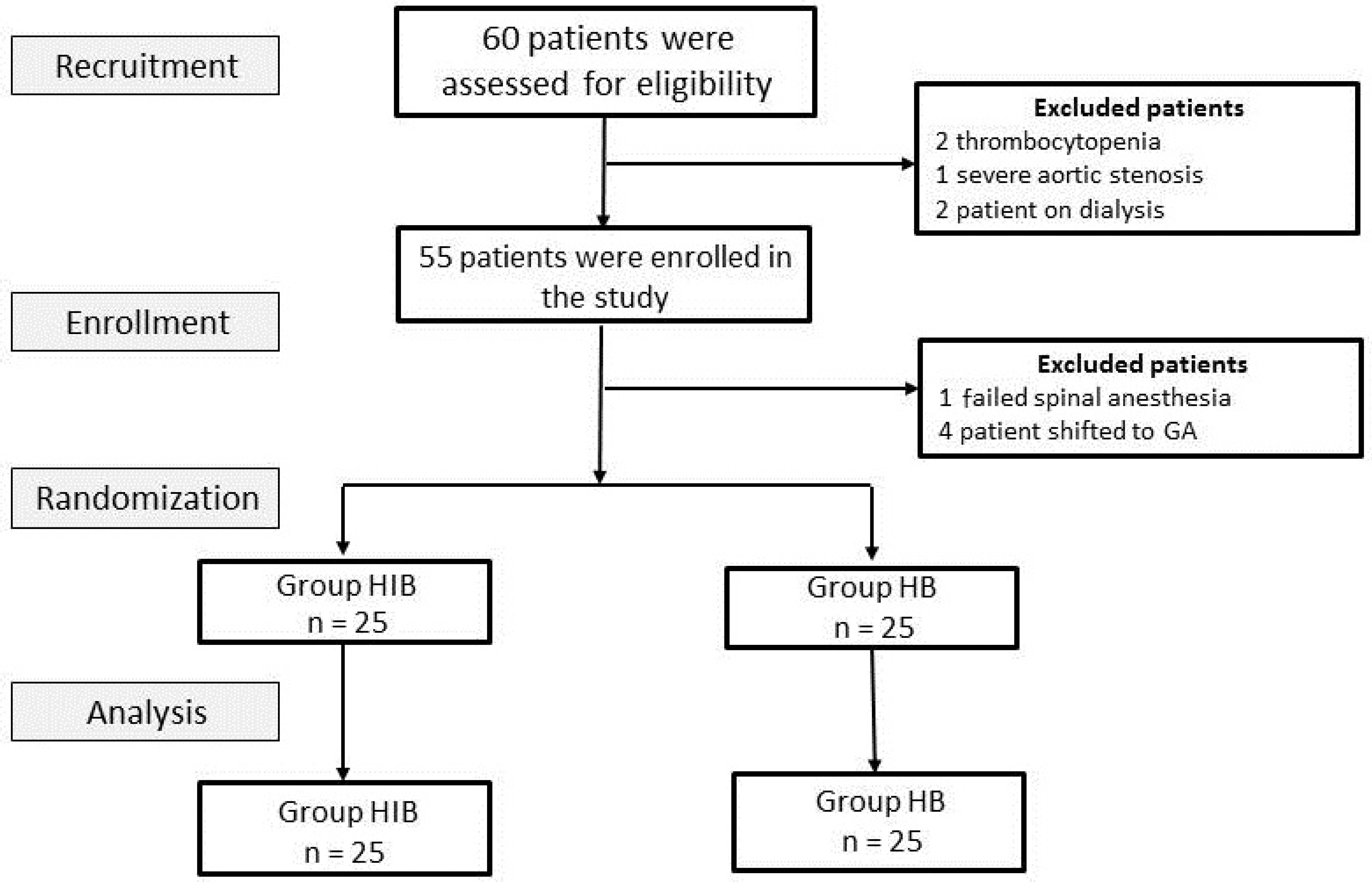
This prospective randomized double-blinded study was conducted after approval of the Institutional Research Board (R.20.01.720) and trial registry (PACTR202002695592368). Informed consent was obtained from elderly patients (age > 60), scheduled for lower limb orthopedic surgery. Patients with one or more of the following factors were excluded from the study: spine deformities on preoperative radiology, local skin infection, coagulation disorders, allergy to LA, neurological disorders, and severe valvular stenotic lesions. Patients were randomly divided into two groups, in blocks of 10, by using a closed envelope technique (Figure 1): group HB (n = 25) and group hyperbaric–isobaric bupivacaine (HIB) (n = 25).
Download full-size image
Abbreviations: HB, hyperbaric bupivacaine; HIB, hyperbaric–isobaric bupivacaine.
After a detailed preoperative assessment, patients were instructed to be fasting for 6 hours. On arrival in the operating theater, pulse oximetry, electrocardiograph, and automatic noninvasive blood pressure were attached, and a large-bore intravenous (IV) line was secured. Ringer’s lactate solution 10 mL/kg was infused over 15–30 min followed by a continuous infusion at a rate of 10–15 mL/kg/h during the operation.
Under full aseptic technique, with the patient in the sitting position, the dural puncture in the midline was performed at L3–4 interspace by using a 25-G Quincke needle with its bevel initially oriented laterally. The needle was advanced slowly till loss of resistance is encountered, and free flow of CSF is detected. The needle bevel is rotated cranially. In the HB group, 3 mL of 0.5% HB mixed with 15 µ of fentanyl citrate (0.3 mL of fentanyl 50 µg/mL) were slowly injected without barbotage. In group HIB, sequential injection of two syringes, 1.5 mL of 0.5% HB with 15 µ of fentanyl citrate (0.3 mL of fentanyl, 50 µg/mL) was injected, followed immediately by 1.5 mL of 0.5% IB, without barbotage.
After we withdrew the spinal needle, all patients were immediately positioned supine for 5 minutes at least if the surgery necessitates another position. An anesthetist not involved in the study protocol assessed and documented the patient data. A sensory level block at T10 was confirmed by loss of sharp pinprick sensation up on both sides and was regarded as sufficient for surgery to proceed. The highest sensory level was recorded. After the patient positioned for surgery, oxygen supplementation was administered at a flow rate of 4 L/min via nasal prongs, and 1–2 mg of midazolam was administered intravenously. Patients’ blood pressure and heart rate (HR) were measured at 5, 10, 20, 30, 60, 75, 90 minutes, and then every 30 minutes till the end of surgery. Additionally, the sensory level was assessed every 30 minutes until time to 2 regressions was recorded. Time to motor function recovery was also documented, indicated by the free movement of the patient foot.
Intraoperative hypotension was defined as the drop of systolic blood pressure by 25% of the basal reading or the drop of mean blood pressure below 60 mmHg. IV vasopressor boluses (ephedrine sulfate 3 mg bolus) were given in case of hypotension meeting the above-mentioned definition or being symptomatic with nausea, vomiting, or altered conscious level. Bradycardia (defined as HR less than 60 or symptomatic bradycardia) was treated by IV atropine sulfate 0.6 mg or ephedrine sulfate 3 mg boluses according to the clinical situation. Also, the incidence of nausea and vomiting during surgery was recorded and treated with IV Ondansetron 4 mg concurrently with the management of any simultaneous hypotension. Patients were kept in recovery till total motor power was achieved for both lower limbs.
If the initial block level was insufficient within 10 minutes after the injection, the patient will be withdrawn from the study and shifted to general anesthesia. Any procedure-related complications were documented, including nausea, vomiting, shivering, pruritus, respiratory depression, failure of anesthesia, and postoperative delirium.
Postoperative analgesia was unified among the study groups. Patients received IV paracetamol 1 gram every 8 hours and ketorolac 30 mg IV every 12 hours. If the patient complained of pain and/or visual analog scale (VAS) reported to be more than 3, IV morphine (0.02 mg/kg) was given as rescue analgesia.
Statistical Analysis
Based on the results of previous studies,12-14 the incidence of hypotension following spinal anesthesia in elderly people reached 80%. The authors expected that the used technique would result in a 30% reduction in the incidence of hypotension. G*power software version 3.1.9.4 was utilized to detect the required sample size. A total number of 46 cases were found to be sufficient to achieve a study power of 90%, and an α error of 0.05. To compensate for dropouts, 60 patients were recruited for the study. Perioperative data were tabulated and analyzed by using IBM SPSS software version 22.0 (IBM Corp, Armonk, NY, USA). Continuous data are presented as mean ± standard deviation (SD) or median (min–max) according to the normality of distribution while nominal and categorical data were presented as numbers and percentages. Independent sample
Results
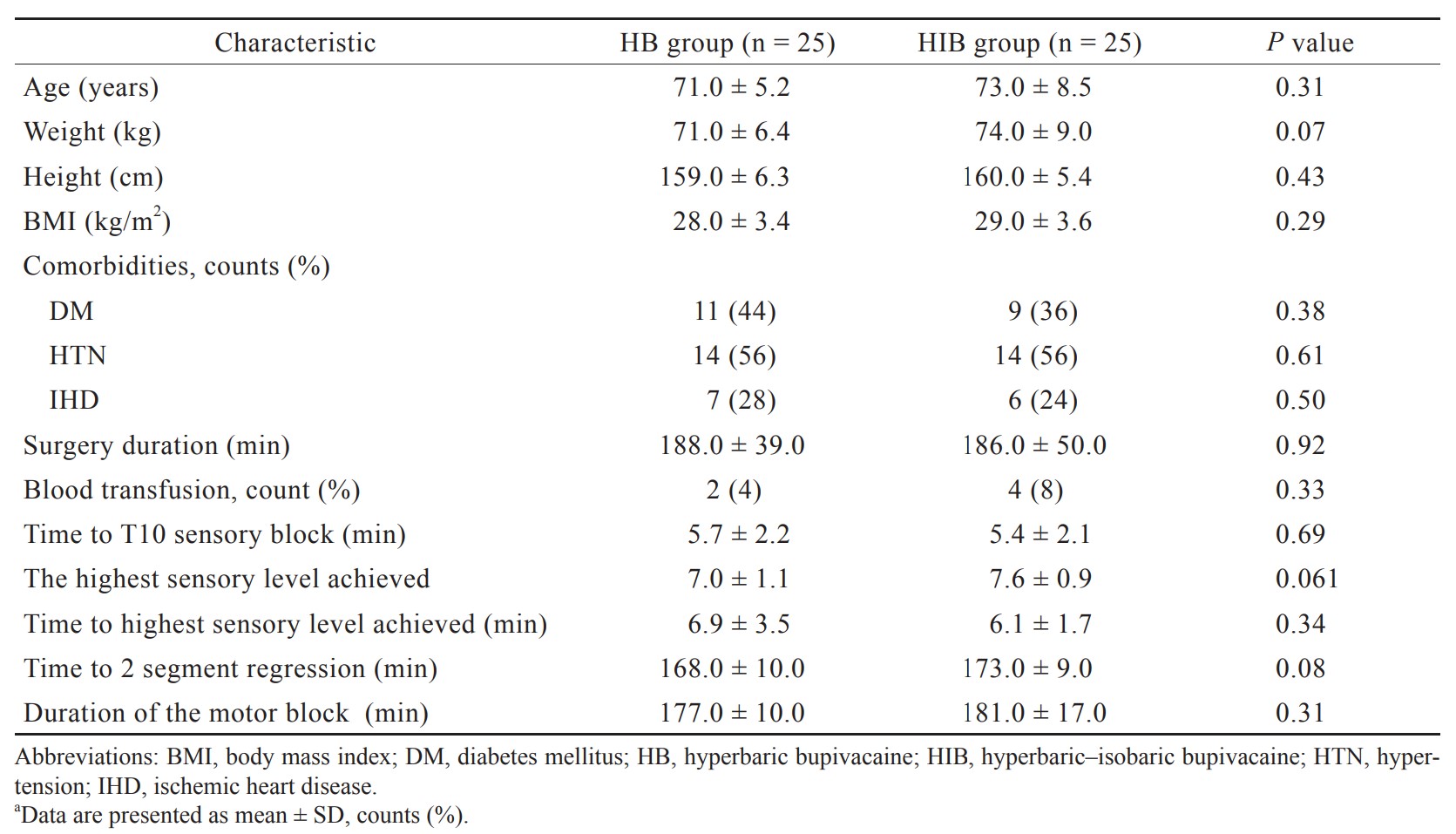
As shown in Figure 1, 60 patients were assessed for eligibility for enrollment where 5 were excluded. Among the eligible patients, 50 patients continued the study protocol, equally divided into the two study groups. Patient demographics, comorbidities, and perioperative characteristics for the whole study cohort and each of the study groups are presented in Table 1. Five minutes after the intrathecal injection, a statistically significant difference in the drop of the mean arterial pressure (MAP) (77 ± 11 mmHg vs. 86 ± 13 mmHg,
Download full-size image
Download full-size image
Abbreviations: HB, hyperbaric bupivacaine; HIB, hyperbaric–isobaric bupivacaine.
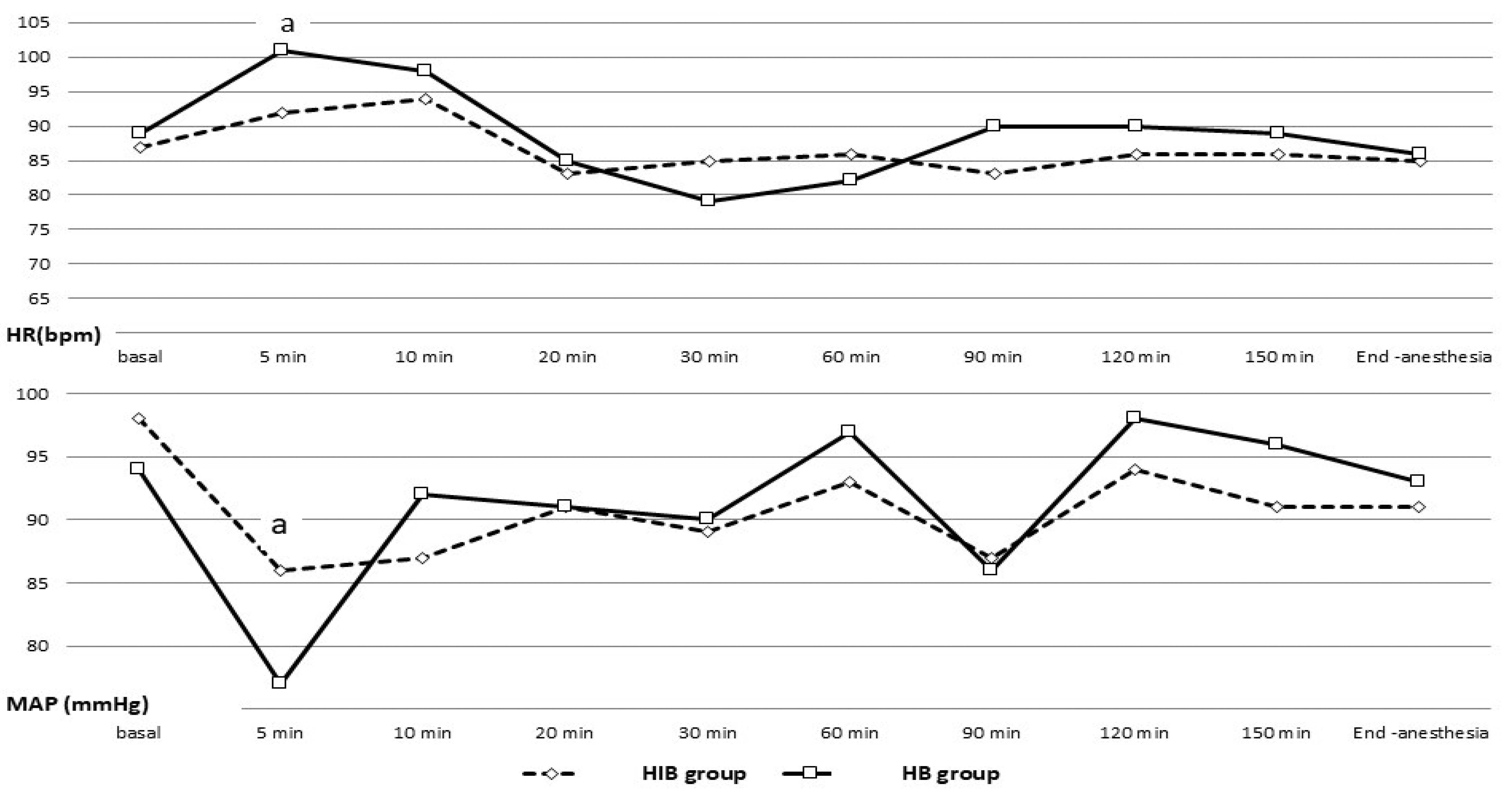
As shown in Figure 3, the absolute incidence of hypotension (16% vs. 44%,
Download full-size image
Abbreviations: HB, hyperbaric bupivacaine; HIB, hyperbaric–isobaric bupivacaine.
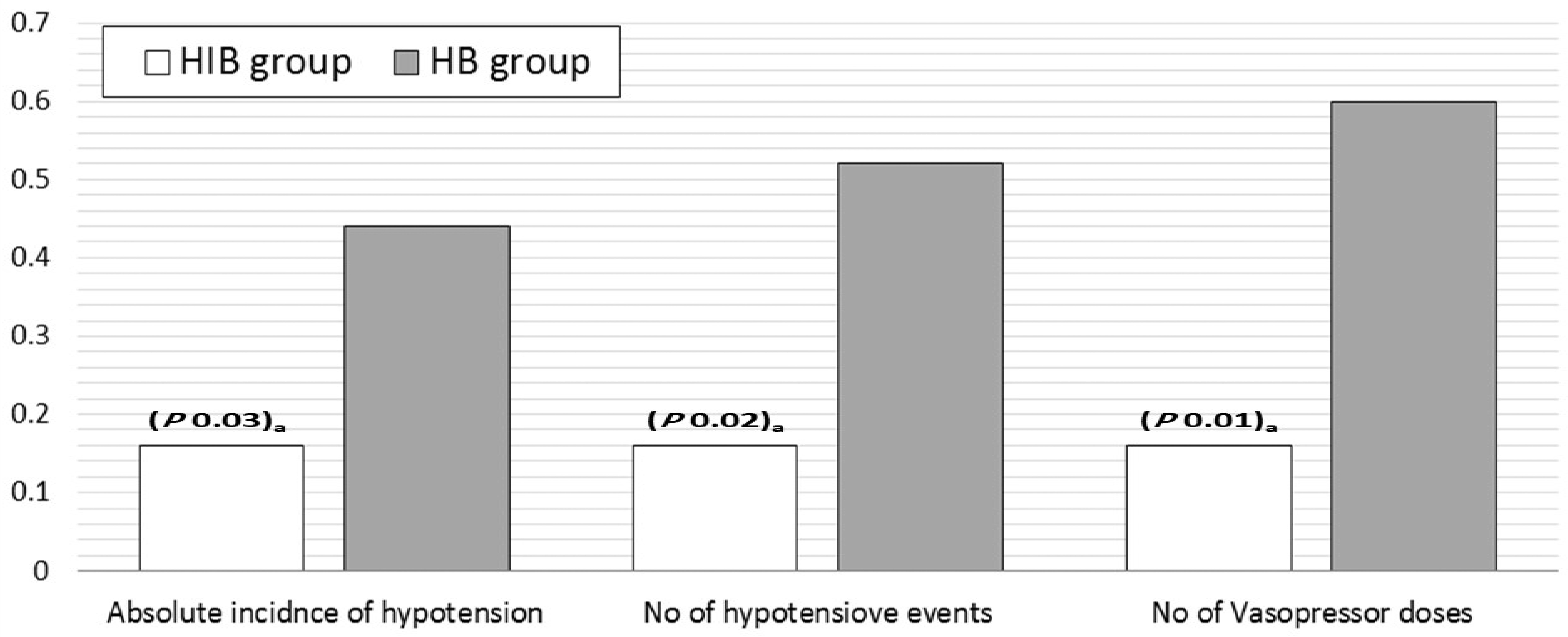
The postoperative analgesic profile is shown in Figure 4; no statically significant difference is detected between the two groups regarding the VAS, time to analgesic request, and postoperative morphine consumption.
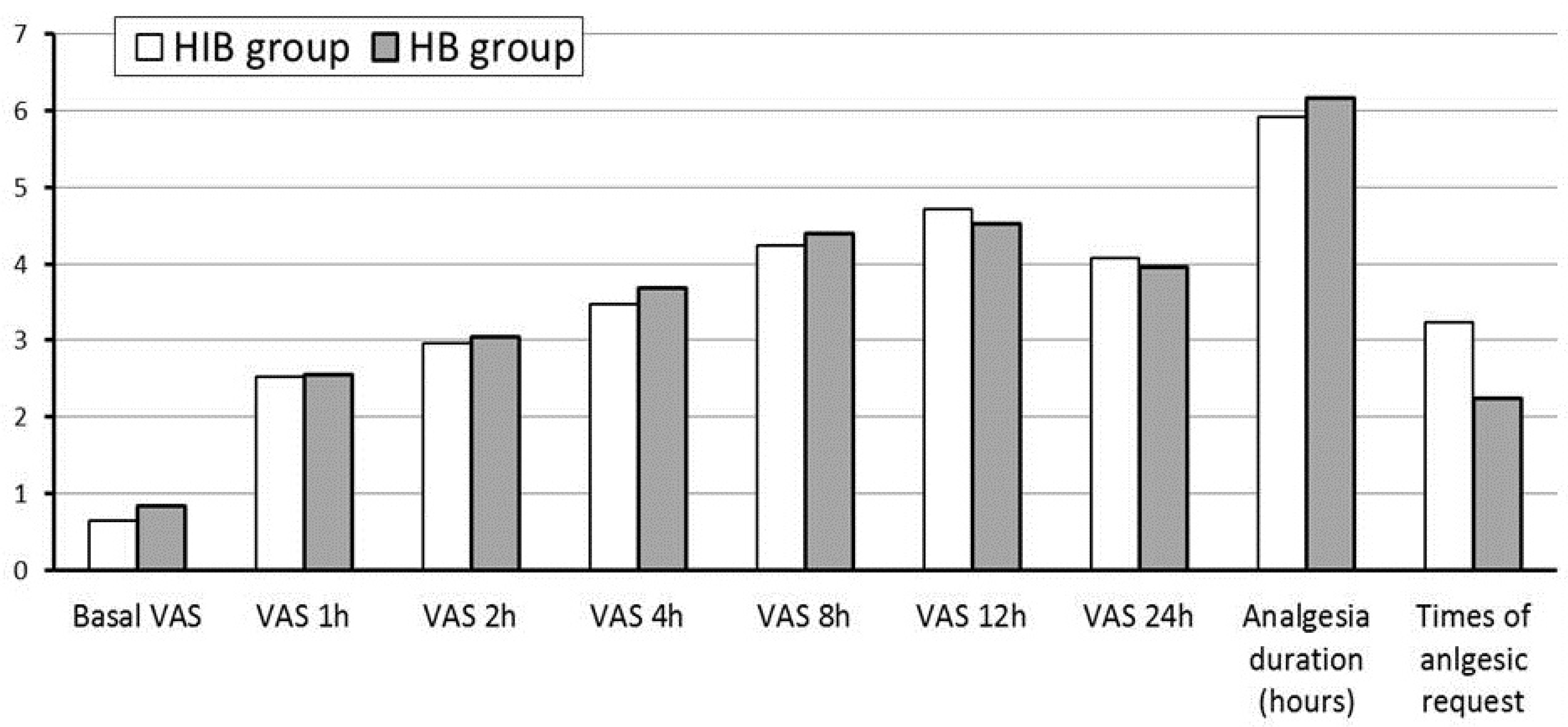
Download full-size image
Abbreviations: HB, hyperbaric bupivacaine; HIB, hyperbaric–isobaric bupivacaine; VAS, visual analog scale.
Discussion
In this study, sequential intrathecal injection of hyperbaric and IB was compared to isolated HB in the elderly population undergoing orthopedic surgeries. Our results show a more stable hemodynamic profile, with a significantly lower incidence of hypotension, lower number of hypotensive episodes, and fewer intraoperative vasopressors doses in the HIB group. The block characteristics regarding the onset, block-level, duration, and postoperative analgesia were compared between the two study groups.
Orthopedic surgery in geriatric patients is associated with higher morbidity and mortality rates; hence, early surgery is warranted to allow earlier mobilization and lower pain levels. Despite no superior advantage for the neuraxial techniques over general anesthesia regarding long-term survival, still it is associated with lower blood loss, better postoperative analgesic profile, and lower incidence of thromboembolism,15 and cognitive dysfunction.16-18 The aging process is associated with decreased physiological reserve especially for the cardiovascular and respiratory system resulting in a higher chance for neuraxial blocks related complications.19-21 Furthermore, orthopedic surgeries mandate larger LA doses to guarantee adequate anesthesia density and duration, which results in a higher sympathetic block and a higher risk of hemodynamic instability.22
To prevent complications like higher block levels, hypotension, bradycardia, cardiac events, and cerebral hypoperfusion, many techniques were tried to modify the classic approach to spinal anesthesia in the elderly population.23-26 Some studies utilized a small dose of local anesthetic while others with or without adjuvant lipophilic opioids27 or lateral positioning of the patient to induce a unilateral block28 and while others tried different medications like levobupivacaine and ropivecaine.29 Yet, it is the baricity that mostly affects the behavior of the injected drug and subsequently the block quality.30
A meta-analysis of 16 studies investigated the differences between HB and IB for non-obstetric surgeries.8 There was no difference in the incidence of hypotension between both formulations. IB resulted in longer block duration and was suggested for longer operative time especially those operated in the lateral position like hip surgeries. The authors suggested that the longer duration is related to higher concentration maintained at the site of injection because of the limited spread of IB versus HB. Likewise, in a meta-analysis of 16 randomized controlled trials involving 724 patients, HB used for spinal anesthesia in non-obstetric surgeries resulted in a shorter duration of both motor and sensory block with no difference in the adverse effects.8 Also, Malinovsky et al.31 studied the effect of volume and baricity of intrathecal bupivacaine and concluded that hyperbaric solution induces shorter sensory anesthesia and motor blockade than an isobaric solution. This was attributed to the restricted spread of HB in the CSF. In our results, time to 2-segment regression was longer in the HIB group; however, this did not reach statistical significance.
Similar to our study, compared to HB in 120 patients undergoing hip surgery,29 isobaric levobupivacaine was associated with better hemodynamic stability. Similar results were demonstrated when HB 0.5% was used for spinal anesthesia in urologic surgery, as the sensory and motor block were faster, resulting in a higher incidence of hypotension.32
The abovementioned differences between the two medications supported our hypothesis that a combination of both may add to the advantage of each one and avoid the related complications. A similar mixture was used during anesthesia for caesarian delivery by Cesur et al.33 who compared the hemodynamic effect of 10 mg HB to sequentially injected IB and HB where the sequential injection resulted in a significantly lower incidence of hypotension, nausea, and vomiting.
An important meta analysis8 compared the use of both formulations in non-obstetric setup, similar results are illustrated in our study. The longer duration of sensory and motor block with IB is an advantage that can be of clinical importance in major orthopedic lower limb surgeries, which is a typical situation in our study layout. As shown in Table 1, in our results, duration of motor block and time required for 2 segment regressions were longer when IB was added to the injected LA. Interestingly, the difference between some study endpoints and those reported in the abovementioned meta analysis8 can be attributed to the addition of narcotics to the injected LA, and importantly, the sequential use of HB and IB in our interventional group while studies with similar methodology were excluded from the meta analysis. Also, the different pharmacodynamic and kinetics expected in the geriatric group population were included in our study.
However, our study has limitations. Invasive arterial monitoring could give additional and valuable data about blood pressure affection in the study. The relatively high dose of LA used in the study is attributed to the nature of complex cases and the application of the study in an educational hospital which adds to the surgical duration, exceeding 3 hours in Table 1; however, we believe this would strengthen the value of the reported results owing to the associated heavier block and hemodynamic effects. Future studies are encouraged to assess if the suggested combination can lower the utilized dose of LA.
In conclusion, our results showed that sequential administration of IB and HB provided the advantage of both formulations and avoided the undesired side effects in the meantime. The lower incidence of intraoperative hypotension and subsequent lower vasopressor requirements indicate the better hemodynamic profile of the sequentially injected mixture while satisfactory block characteristics (e.g., onset, intensity, and duration) were compared to HB alone.
Conflict of Interest
None.
Funding
Support was provided solely from institutional and departmental sources.
IRB Approval
(R.20.01.720) Institutional Research Board, Mansoura University, Egypt.
Trial Registry
PACTR202002695592368, January, 2020.
References
| 1 |
Roberts SE, Goldacre MJ.
Time trends and demography of mortality after fractured neck of femur in an English population, 1968–98: database study.
BMJ. 2003;327(7418):771-775.
|
| 2 |
Borges FK, Bhandari M, Patel A, et al.
Rationale and design of the HIP fracture Accelerated surgical TreaTment and Care tracK (HIP ATTACK) Trial: a protocol for an international randomised controlled trial evaluating early surgery for hip fracture patients.
BMJ Open. 2019;9(4):e028537.
|
| 3 |
Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB.
Incidence and mortality of hip fractures in the United States.
JAMA. 2009;302(14):1573-1579.
|
| 4 |
Kowark A, Rossaint R, Coburn M.
General versus spinal anesthesia for the elderly hip fractured patient.
Curr Opin Anaesthesiol. 2019;32(1):116-119.
|
| 5 |
Atallah MM, Abdel Dayem OT.
Effect of different baricities of intrathecal bupivacaine on the quality of spinal block in elderly patients undergoing transurethral resection of the prostate.
Res Opin Anesth Intensive Care. 2015;2(4):121-125.
|
| 6 |
Atashkhoei S, Abedini N, Pourfathi H, Znoz AB, Marandi PH.
Baricity of bupivacaine on maternal hemodynamics after spinal anesthesia for cesarean section: a randomized controlled trial.
Iran J Med Sci. 2017;42(2):136-143.
|
| 7 |
Gupta R, Bogra J, Singh PK, Saxena S, Chandra G, Kushwaha JK.
Comparative study of intrathecal hyperbaric versus isobaric ropivacaine: a randomized control trial.
Saudi J Anaesth. 2013;7(3):249-253.
|
| 8 |
Uppal V, Retter S, Shanthanna H, Prabhakar C, McKeen DM.
Hyperbaric versus isobaric bupivacaine for spinal anesthesia: systematic review and meta-analysis for adult patients undergoing noncesarean delivery surgery.
Anesth Analg. 2017;125(5):1627-1637.
|
| 9 | |
| 10 |
Desai S, Lim Y, Tan CH, Sia ATH.
A randomised controlled trial of hyperbaric bupivacaine with opioids, injected as either a mixture or sequentially, for spinal anaesthesia for caesarean section.
Anaesth Intensive Care. 2010;38(2):280-284.
|
| 11 |
Helmi M, Uyun Y, Suwondo BS, Widodo U.
Comparison of intrathecal use of isobaric and hyperbaric bupivacaine during lower abdomen surgery.
J Anesth. 2014;2014:141324.
|
| 12 |
Olofsson C, Nygårds EB, Bjersten AB, Hessling A.
Low-dose bupivacaine with sufentanil prevents hypotension after spinal anesthesia for hip repair in elderly patients.
Acta Anaesthesiol Scand. 2004;48(10):1240-1244.
|
| 13 |
Minville V, Fourcade O, Grousset D, et al.
Spinal anesthesia using single injection small-dose bupivacaine versus continuous catheter injection techniques for surgical repair of hip fracture in elderly patients.
Anesth Analg. 2006;102(5):1559-1563.
|
| 14 |
Ben-David B, Frankel R, Arzumonov T, Marchevsky Y, Volpin G.
Minidose bupivacaine–fentanyl spinal anesthesia for surgical repair of hip fracture in the aged.
Anesthesiology. 2000;92(1):6-10.
|
| 15 |
Urwin SC, Parker MJ, Griffiths R.
General versus regional anaesthesia for hip fracture surgery: a meta-analysis of randomized trials.
Br J Anaesth. 2000;84(4):450-455.
|
| 16 |
Chen DX, Yang L, Ding L, Li SY, Qi YN, Li Q.
Perioperative outcomes in geriatric patients undergoing hip fracture surgery with different anesthesia techniques: a systematic review and meta-analysis.
Medicine (Baltimore). 2019;98(49):e18220.
|
| 17 |
Guay J, Parker MJ, Gajendragadkar PR, Kopp S.
Anaesthesia for hip fracture surgery in adults.
Cochrane Database Syst Rev. 2016;2(2):CD000521.
|
| 18 |
Alvarez-Bastidas L, Valle-Leal JG, Morales-Vera E, Marroquín-González J.
Delirium in the elderly patient after anesthesia: associated factors.
Colomb J Anesthesiol. 2018;46(4):273-278.
|
| 19 | |
| 20 |
Tarazona-Santabalbina FJ, Belenguer-Varea Á, Rovira E, Cuesta-Peredó D.
Orthogeriatric care: improving patient outcomes.
Clin Interv Aging. 2016;11:843-856.
|
| 21 |
Chan SP, Ip KY, Irwin MG.
Peri-operative optimisation of elderly and frail patients: a narrative review.
Anaesthesia. 2019;74(Suppl 1):80-89.
|
| 22 |
Tsui BC, Wagner A, Finucane B.
Regional anaesthesia in the elderly: a clinical guide.
Drugs Aging. 2004;21(14):895-910.
|
| 23 |
Loubert C, Hallworth S, Fernando R, et al.
Does the baricity of bupivacaine influence intrathecal spread in the prolonged sitting position before elective cesarean delivery?
Anesth Analg. 2011;113(4):811-817.
|
| 24 |
Koo BS, Jung MJ, Lee JH, Cho SH, Kim SH, Chae WS.
Anesthetic experience of spinal anesthesia after sedation in un-cooperated elderly patients.
Soonchunhyang Medical Science. 2016;22(1):59-63.
|
| 25 |
Martyr JW, Clark MX.
Hypotension in elderly patients undergoing spinal anaesthesia for repair of fractured neck of femur.
Anaesth Intensive Care. 2001;29(5):501-505.
|
| 26 |
Sivevski AG, Karadjova D, Ivanov E, Kartalov A.
Neuraxial anesthesia in the geriatric patient.
. Front Med (Lausanne). 2018;5:254.
|
| 27 |
Kumar S, Bajwa SJS.
Neuraxial opioids in geriatrics: a dose reduction study of local anesthetic with addition of sufentanil in lower limb surgery for elderly patients.
Saudi J Anaesth. 2011;5(2):142-149.
|
| 28 |
Kilinc LT, Sivrikaya GU, Eksioglu B, Hanci A, Dobrucali H.
Comparison of unilateral spinal and continous spinal anesthesia for hip surgery in elderly patients.
Saudi J Anaesth. 2013;7(4):404-409.
|
| 29 |
Herrera R, De Andrés J, Estañ L, Olivas FJ, Martínez-Mir I, Steinfeldt T.
Hemodynamic impact of isobaric levobupivacaine versus hyperbaric bupivacaine for subarachnoid anesthesia in patients aged 65 and older undergoing hip surgery.
BMC Anesthesiol. 2014;14:97.
|
| 30 | |
| 31 |
Malinovsky JM, Renaud G, Le Corre P, et al.
Intrathecal bupivacaine in humans: influence of volume and baricity of solutions.
Anesthesiology. 1999;91(5):1260-1266.
|
| 32 |
Critchley LA, Morley AP, Derrick J.
The influence of baricity on the haemodynamic effects of intrathecal bupivacaine 0.
Anaesthesia. 1999;54(5):469-474.
|
| 33 |
Cesur M, Alici HA, Erdem AF, Borekci B, Silbir F.
Spinal anesthesia with sequential administration of plain and hyperbaric bupivacaine provides satisfactory analgesia with hemodynamic stability in cesarean section.
Int J Obstet Anesth. 2008;17(3):217-222.
|