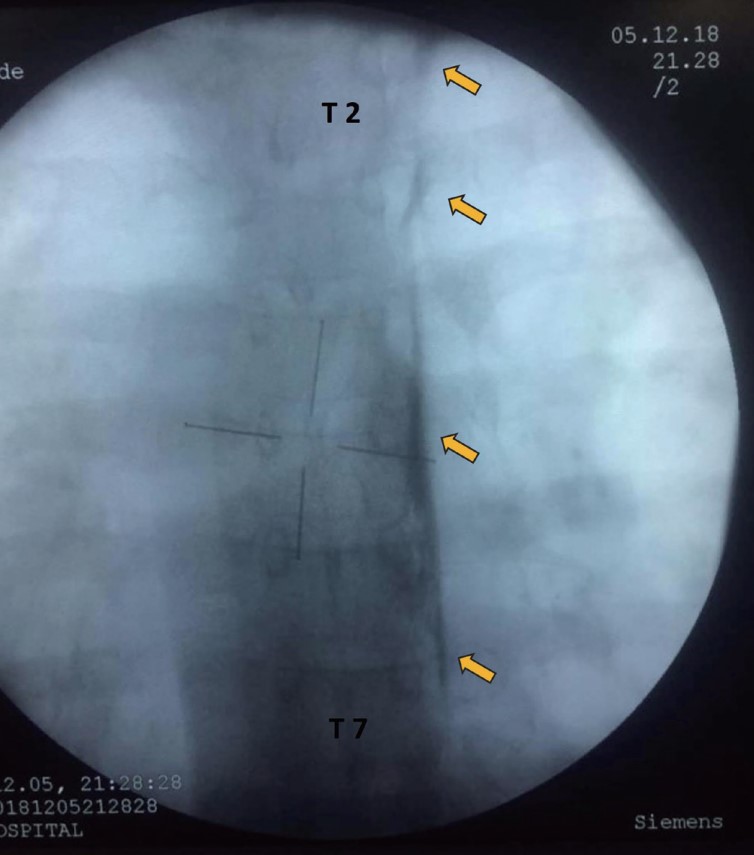
We observed ipsilateral miosis, ptosis, and conjunctival hyperemia suggestive of Horner’s syndrome in a patient following a thoracic paravertebral catheter inserted at the T7 level. A fluoroscopic study of catheter position using 4.5 mL of iohexol 240 mg/mL through the paravertebral catheter showed a tight linear spread of contrast, lateral to the vertebral body up to the T1 level (Figure 1). The clinical finding of Horner’s syndrome and the pattern of spread of contrast were suggestive of blockade of the sympathetic trunk up to the stellate ganglion. The existing literature suggests that the thoracic paravertebral space is divided into two compartments by the endothoracic fascia with the sympathetic trunk in the anterior compartment and the spinal nerves in the posterior compartment.1 Prior literature also suggests that any injection anterior to the endothoracic fascia is likely to spread to the contralateral side.2 However, in the present case, we did not observe a contralateral spread of the drug although the sympathetic trunk was blocked.
Download full-size image
Fluoroscopic image after injection of 4.5 mL of contrast through the paravertebral catheter. The yellow arrows indicate the linear spread of contrast lateral to the thoracic vertebral body from T7 to T1.
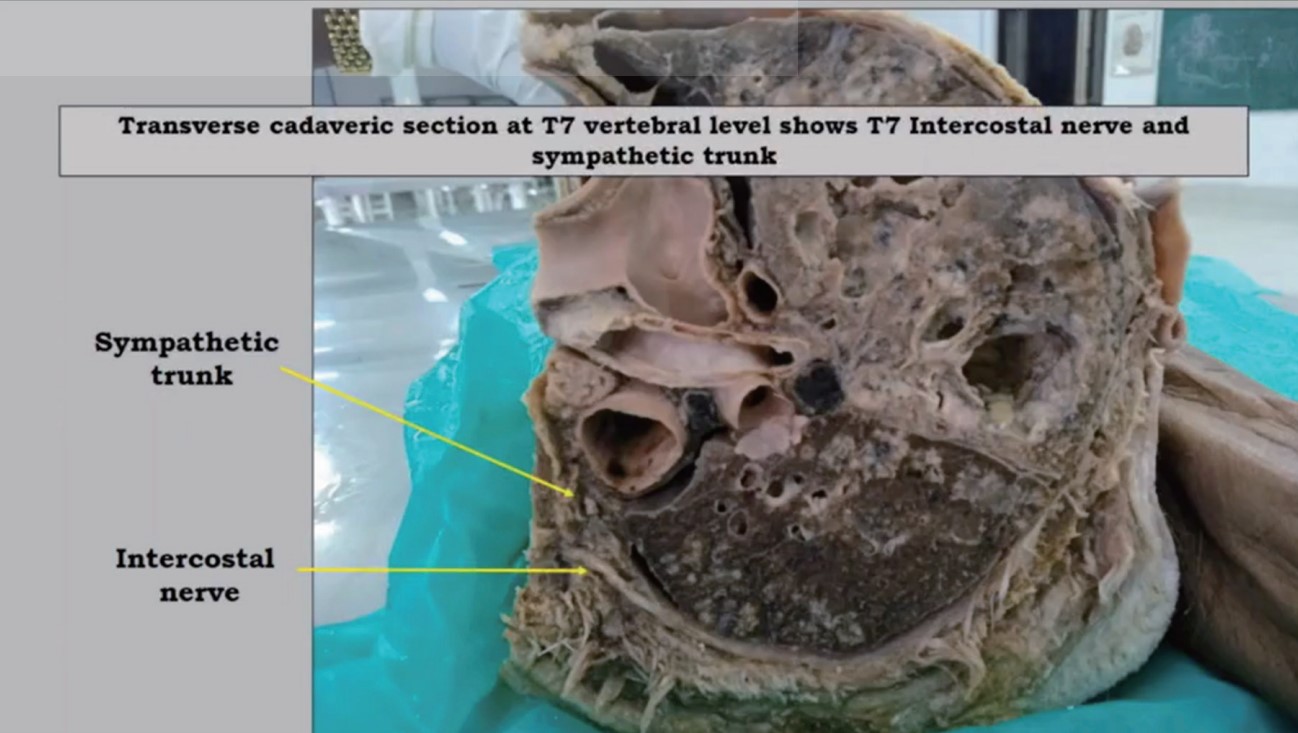
To understand the fascial arrangements that can result in such a spread, the posterior thoracic wall of two cadavers was dissected after eviscerating the lungs. The step-wise dissection to expose the sympathetic trunk is illustrated in Video 1. The cadaveric dissection made clear the following anatomical relationships between the endothoracic fascia and the sympathetic chain in the paravertebral space. First, the sympathetic trunk and the spinal nerves both lie posterior to the endothoracic fascia. Second, the endothoracic fascia encloses the sympathetic trunk against the vertebral body. A local anesthetic injected into the endothoracic fascial pocket enclosing the sympathetic trunk can produce a dense unilateral sympathetic block. It is likely that our catheter was threaded into this compartment.
Download full-size image
Transverse cadaveric section at T7 vertebral level showing T7 intercostal nerve and sympathetic trunk. Parietal pleura can be seen on eviscerating the lung. The parietal pleura could be easily separated from the endothoracic fascia. When the parietal pleura is separated from the endothoracic fascia, the intervening subserous fascia is seen between the two layers. The elevation of endothoracic fascia exposes the sympathetic trunk on the anterolateral aspect of the vertebral body. Both the sympathetic chain and the intercostal nerves are seen to lie posterior to the endothoracic fascia. The internal intercostal membrane and innermost intercostal muscles are also seen. The endothoracic fascia is seen adhered to the vertebral body on either side of the sympathetic chain. The medial end of the clavicle is cut and the sympathetic trunk is exposed from the thoracic level to the neck. The endothoracic fascia continues as prevertebral fascia above T3 vertebral level.
Acknowledgments
None.
Conflict of Interest
None.