Anaphylaxis is a systemic hypersensitivity reaction of sudden onset that is often life-threatening. Various agents such as neuromuscular blocking agents (NMBAs), latex, and antibiotics may cause anaphylactic reactions, potentially leading to death. In approximately 60% of anesthesia-related cases, anaphylaxis is caused by NMBA usage.1 Accordingly, it is mandatory to accurately determine causative agents for anaphylaxis to ensure safe surgery after a previous episode of anesthesia-related anaphylaxis.
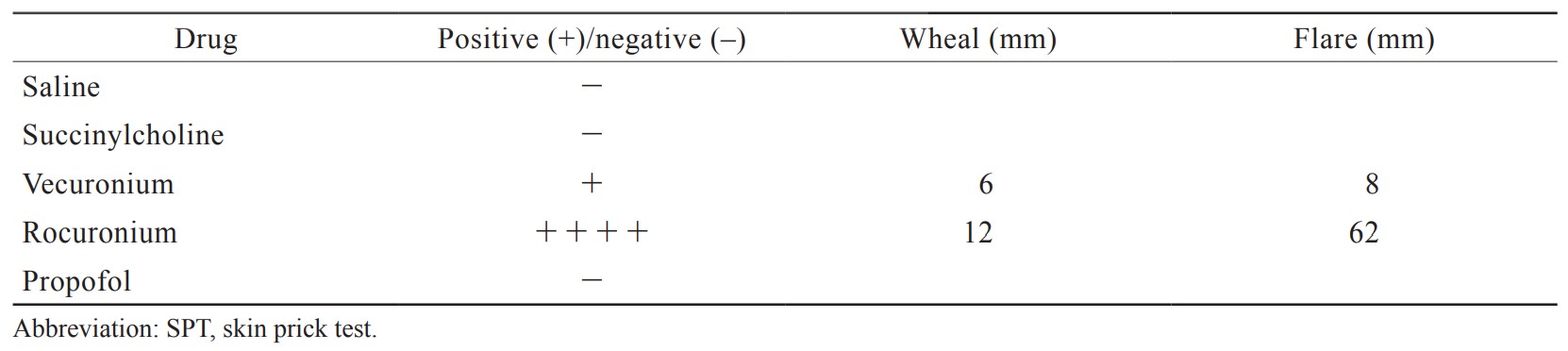
An 82-year-old man was scheduled to undergo surgery for an external dental fistula on the mentum. The patient had not previously undergone any general anesthesia. Anesthesia was induced with propofol, continuous infusion of remifentanil, and rocuronium. After administration of rocuronium, his entire body began to flush with erythema and wheals. After tracheal intubation, peak airway pressure increased to > 40 cmH2O with a tidal volume of less than 200 mL. His oxygen saturation decreased to 90%, despite ventilation with 100% oxygen. Furthermore, his systolic blood pressure decreased to 44 mmHg and his heart rate increased to 120 bpm. Expiratory wheezing was observed throughout the chest. Because we suspected an anaphylactic reaction, 100 mg hydrocortisone and 0.2 mg epinephrine were administered intravenously and intramuscularly, respectively. He was also treated with repeated salbutamol inhalation and 5% sevoflurane for bronchospasm. His respiratory and hemodynamic status improved to almost normal approximately 10 min after administration of epinephrine. However, the surgery was canceled. Twenty minutes after recovery from the shock state, 2 mg neostigmine with 1 mg atropine was administered to reverse residual blockade. After we confirmed that his respiratory condition met the criteria for extubation, his trachea was extubated uneventfully. The patient was observed until his hemodynamic and respiratory conditions were stabilized under spontaneous breathing. The patient was then transferred to the ward, and we performed drug-induced lymphocyte stimulation tests (DLSTs) for propofol, vecuronium, succinylcholine, and rocuronium. However, the results for all agents were negative. Surgery was scheduled approximately 7 weeks after the anaphylactic reaction. Subsequently, dermatologists were consulted for skin testing. Following consultation, a skin prick test (SPT) for rocuronium, vecuronium, succinylcholine, and propofol was scheduled immediately after hospitalization. SPT was performed in a ward under the strict supervision of physicians, using the original test drug solution and saline as a negative control 7 weeks after the anaphylactic reaction. A histamine test, normally used as a positive control, was not available at our institution. SPT showed a very strong positive reaction to rocuronium and a positive reaction to vecuronium, but a negative reaction to propofol and succinylcholine (Table 1). Surgery was then performed. General anesthesia using succinylcholine was safely performed. The surgery was uneventful and the patient recovered uneventfully.
Download full-size image
The skin test remains the golden standard as a definitive diagnostic tool for perioperative anaphylaxis, according to most guidelines.3,4 It should be performed 4–6 weeks after the onset of anaphylaxis to avoid false-negative results.3 In case of another allergic reaction, the skin test should be undertaken under the strict supervision of physicians. The sensitivity of SPT seems to be inferior to that of the intradermal test (IDT) for most drugs. Thus, it may be desirable to perform SPT followed by IDT. In the present case, results were positive for rocuronium and vecuronium, but negative for succinylcholine, suggesting a cross-reaction between the two non-depolarizing NMBAs. In the present case, IDT was not performed following SPT. However, considering the possibilities of false-negative results with SPT and the cross-reaction between rocuronium and succinylcholine,5 it would be better to perform IDT for succinylcholine, in addition to SPT.
The skin test is the golden standard for the postoperative diagnosis of anaphylaxis.
Acknowledgments
Not applicable.
Conflict of Interest
The authors declare no potential conflicts of interest relevant to this article.
References
| 1 |
Chiriac AM, Tacquard C, Fadhel NB, et al.
Safety of subsequent general anaesthesia in patients allergic to neuromuscular blocking agents: value of allergy skin testing.
Br J Anaesth. 2018;120(6):1437-1440.
|
| 2 |
Tokuwaka J, Takahashi S, Tanaka M.
Anaphylaxis after sugammadex administration.
Can J Anaesth. 2013;60(7):733-734.
|
| 3 |
Takazawa T, Yamaura K, Hara T, et al.
Practical guidelines for the response to perioperative anaphylaxis.
J Anesth. 2021;35(6):778-793.
|
| 4 |
Harper NJ, Dixon T, Dugué P, et al.
Suspected anaphylactic reactions associated with anaesthesia.
Anaesthesia. 2009;64(2):199-211.
|
| 5 |
Russell WJ, Lee C, Milne D.
Is allergy to rocuronium a high probability cross-reaction with suxamethonium?
Anaesth Intensive Care. 2003;31(3):333.
|