Abstract
Background
Adductor canal block (ACB) is a motor sparing block providing analgesia for surgeries involving anterior part of the knee. The aim of our study was to evaluate the analgesic efficacy of ACB to reduce pain in arthroscopic knee surgeries done under spinal anesthesia. Our primary objective was to evaluate the 24 hours postoperative morphine consumption. The secondary objectives were to evaluate the visual analog scale (VAS) scores at rest and during knee flexion, hemodynamics and side effects of the block.
Methods
In this prospective randomised controlled trial, 70 patients who underwent arthroscopic knee surgeries were randomly divided into two groups, A and C. Surgeries were done under spinal anesthesia. Group A patients received ACB with 20 mL of 0.5 % ropivacaine using ultrasound postoperatively. Block was not performed in group C. The amount of morphine consumption in PCA pump, duration of analgesia, mean VAS scores at rest and flexion, hemodynamics and adverse effects were monitored.
Results
The average morphine consumption was significantly lesser with a
Conclusions
We conclude that ultrasound-guided ACB resulted in significantly lesser morphine consumption after arthroscopic knee surgeries. ACB prolonged the duration of analgesia with better hemodynamics, lesser VAS pain scores and with no complications.
Keywords
adductor canal block, knee surgeries, patient controlled analgesia, postoperative analgesia, visual analogue scale
Introduction
Orthopedic surgeries are usually associated with intense pain and require adequate pain relief for early postoperative mobilization and to decrease the complications associated with prolonged immobility. NSAIDs (non-steroidal anti-inflammatory drugs) and opioids are the commonly prescribed drugs that have side effects like gastritis, renal toxicity, sedation, pruritus, nausea, vomiting, and respiratory depression.1,2 Epidural analgesia is considered the gold standard for lower limb orthopedic surgeries which may be associated with motor blockade in both legs and hemodynamic instability.3 Regional anesthetic techniques like femoral nerve block, adductor canal block (ACB), local infiltration anesthesia, iPACK (infiltration between the popliteal artery and capsule of the knee) and sciatic nerve block are alternate methods used to control pain following knee surgeries. Peripheral nerve blocks provide adequate analgesia, early postoperative mobilization, decreased morbidity and decreased length of hospital stay.4
ACB is a novel motor sparing block that can be used as an alternative to femoral nerve block with the advantage of earlier mobilization of the patient. There was limited literature published on ACB using ropivacaine. Hence, we conducted this study to evaluate the analgesic efficacy of ACB in arthroscopic knee surgeries. The primary objective of the study is to evaluate the total morphine consumption for 24 hours after surgery. The secondary objectives were to evaluate the average visual analog scale (VAS) scores in 24 hours at rest and during flexion, postoperative hemodynamic parameters and side effects of the block. We hypothesized ACB would provide effective postoperative analgesia in terms of reduced morphine consumption, VAS scores for pain and adverse effects.
Methods
This study was registered in Clinical Trial Registry-India (CTRI/2019/09/021182). After institutional ethics committee approval and getting informed consent from patients, this study was done on 70 patients who underwent elective knee arthroscopic procedures under spinal anesthesia. The patients were divided into two equal groups—group A, who received ultrasound-guided ACB with 20 mL of 0.5% ropivacaine and group C, who did not receive a block. This study was a single-blinded, randomized controlled trial done from October 15, 2019, to September 30, 2020. Patients of American Society of Anesthesiologists (ASA) grade 1 and 2, aged between 18 and 60 years and BMI ranging from 18 to 30, posted for elective knee arthroscopic procedures were included in the study. Those who were unwilling to take part, had an allergy to study drugs, were pregnant, had coagulation abnormalities and undergoing bilateral or revision knee surgeries were excluded.
Patients were randomly divided into two groups by computer-generated random numbers, and group allocation was done by sealed envelope method. The patients fasted 6 hours before surgery and oral premedication was done with alprazolam 0.5 mg, ranitidine 150 mg, and ondansetron 4 mg 2 hours before surgery. Standard monitors like electrocardiogram, non-invasive blood pressure and pulse oximetry were instituted in all cases. All the surgeries were done under spinal anesthesia with 15 mg of hyperbaric bupivacaine to achieve a sensory blockade up to the level of T10. Patients in group A received ACB after the surgery, and no block was given to patients in group C. The ACB was given at the end of surgery after the recession of spinal sensory level till T12.
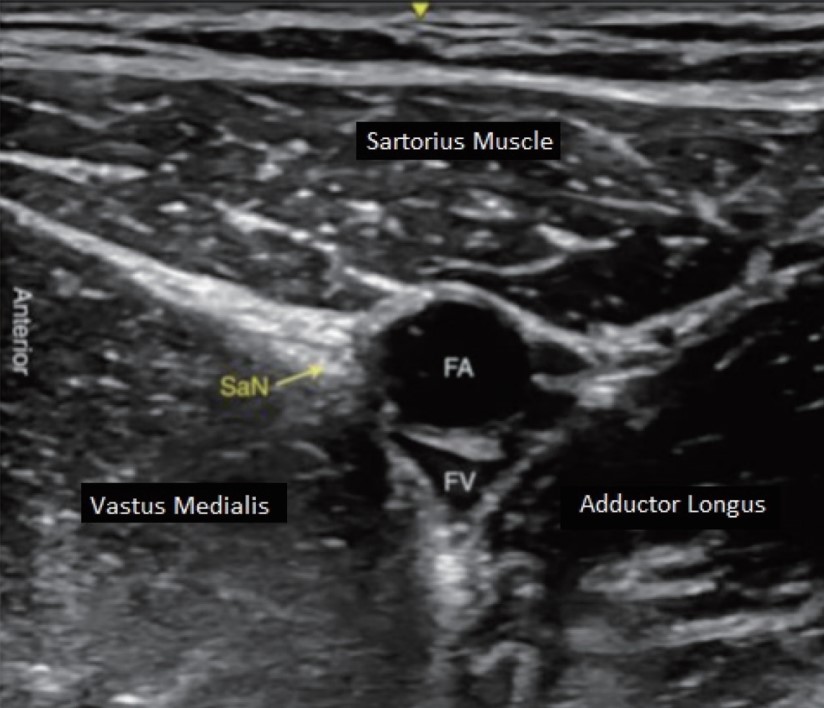
A high-frequency linear ultrasound transducer (7–13 MHz) in LOGIQ V2 (GE Healthcare, Chicago, IL, USA) ultrasound machine was placed in the medial compartment of the thigh midway between anterior superior iliac spine and patella with the leg moderately rotated outwards. In the adductor canal, the femoral artery was visualized in the short axis below the sartorius muscle and medial to vastus medialis (Figure 1). Under aseptic precautions, a 22 G stimuplex needle was inserted using an in-plane technique from the lateral side of the ultrasound transducer. The needle tip was positioned below the sartorius muscle lateral to the artery and saphenous nerve. After we pierced the vastoadductor membrane, 2–3 mL of saline was used to confirm the correct position. Moreover, 20 mL of 0.5% ropivacaine was slowly injected around the saphenous nerve in the adductor canal in 5 mL aliquots after repeated aspiration.
Download full-size image
Abbreviations: FA, femoral artery; FV, femoral vein; SaN, saphenous nerve.
Patients were shifted to postanesthesia care unit and VAS scores were measured every hour up to 4 hours, every 2 hours up to 12 hours and every 6 hours up to 24 hours postoperative period, both at rest and 45° flexion (measured using goniometer). Morphine was administered through patient-controlled analgesia (PCA) pump postoperatively with a basal infusion of 0.1 mg/h, a bolus dose of 1 mg and lockout interval of 10 minutes in both the groups. The patients were explained about the use of PCA pump during preoperative assessment and also before connecting to the patient. Paracetamol 1 g was administered intravenously every 6 hours in the postoperative period as a part of multimodal analgesia in patients of both the groups. Tramadol 2 mg/kg was used as a rescue analgesic if the patient had significant pain (VAS ≥ 4) in both the groups despite PCA morphine boluses. Patients were monitored in the postoperative period for the amount of morphine consumption in the first 24 hours, time to first rescue analgesia (time from the end of the surgery to first bolus dose in PCA pump), VAS pain score over 24 hours, postoperative hemodynamics, complications of the block, if any and side effects related to morphine infusion.
The sample size was determined by evaluating the total morphine consumption in the 24 hours postoperative period which was the primary objective of our study. In a pilot study on 12 patients, 6 patients received spinal anesthesia with ACB and 6 patients received only spinal anesthesia. Pooled standard deviation was 5, and the mean difference between the two groups was 3.21 with a study power of 90% and β-error of 0.05.
(r = n1/n2 = 1, Zα/2 = 1.96, Z1 – β = 90%, study power = 1.28, σ = pooled standard deviation = 5, d = mean difference = 3.21). The value of N derived was 52.5. We have taken 35 patients in each group to compensate for the risk of dropouts.
Results
Data were entered in MS-Excel spreadsheet (2010) and were found to be normal in distribution. No skewing of data was noted. Descriptive statistics were done for all data and were reported in terms of mean values and percentages. Suitable statistical tests of comparison were applied in Statistical Package for Social Sciences (SPSS) version 22.0 (IBM corp., Armonk, NY, USA). Continuous variables were analyzed with the unpaired
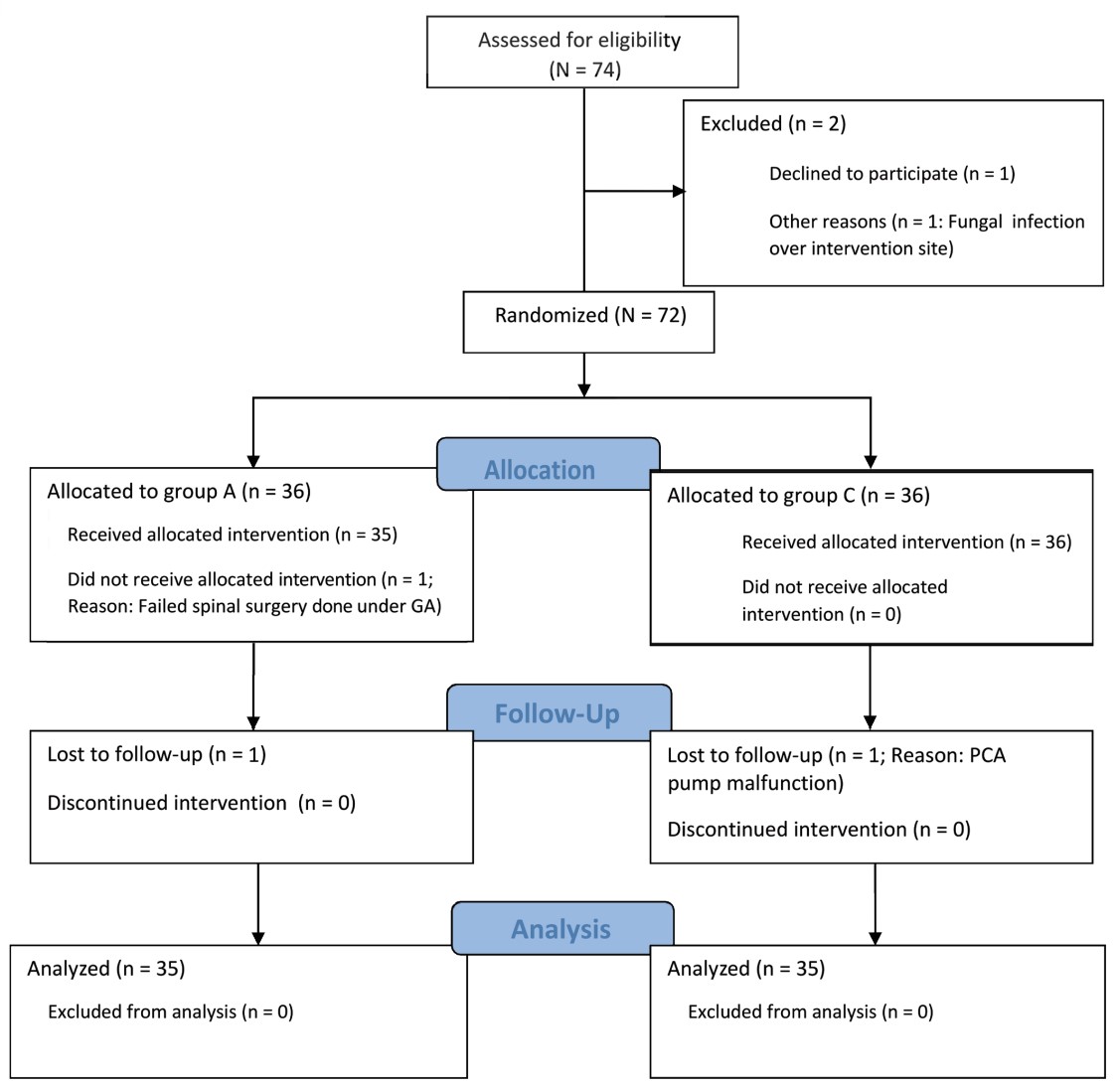
Seventy-four patients were assessed for eligibility and after we excluded 4 patients during the study, 70 patients were finally analyzed (n = 35 in each group). The flow of patients was shown in the CONSORT (CONsolidated Standards Of Reporting Trials) diagram as in Figure 2.
Download full-size image
Abbreviations: GA, general anesthesia; PCA, patient-controlled analgesia.
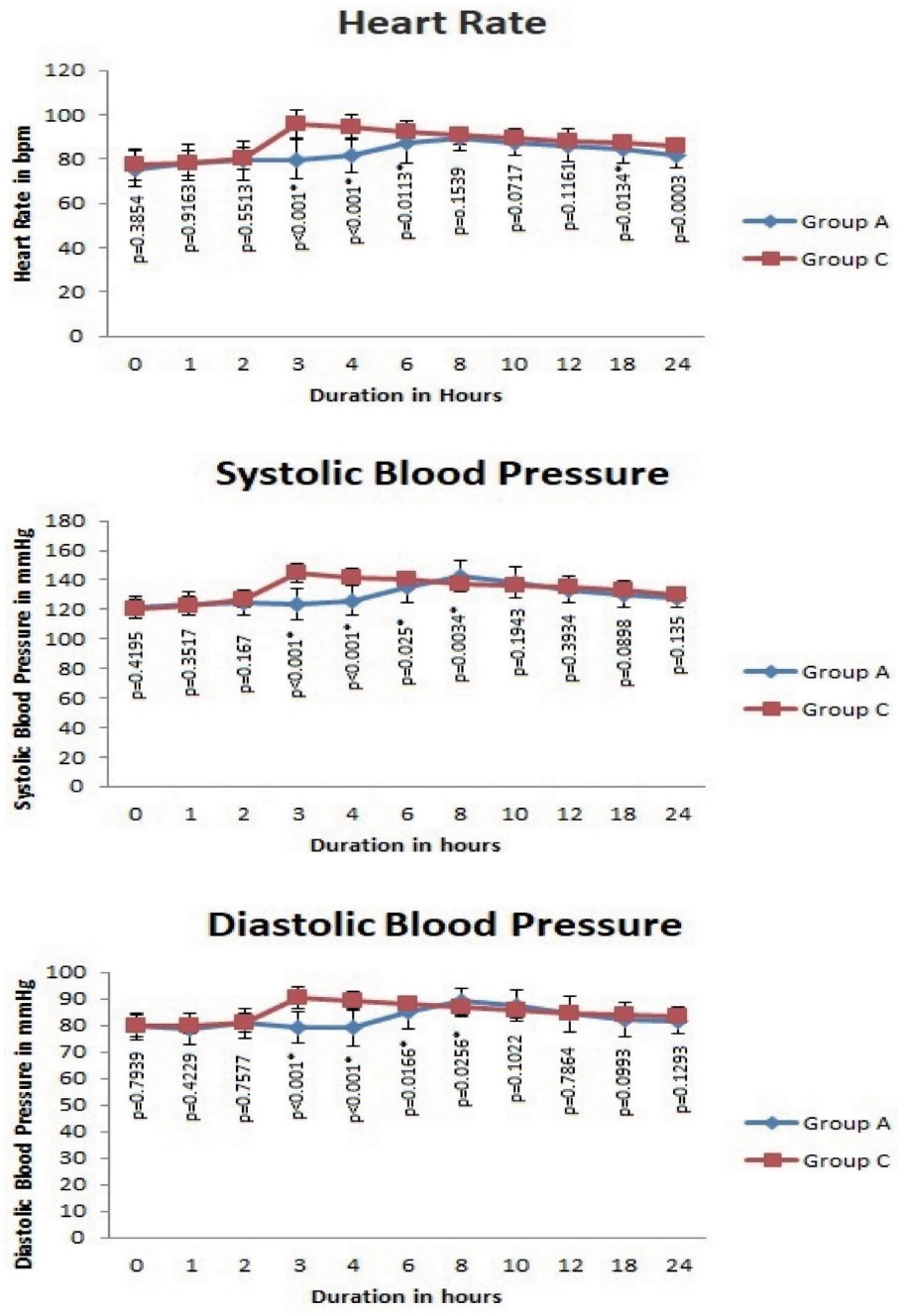
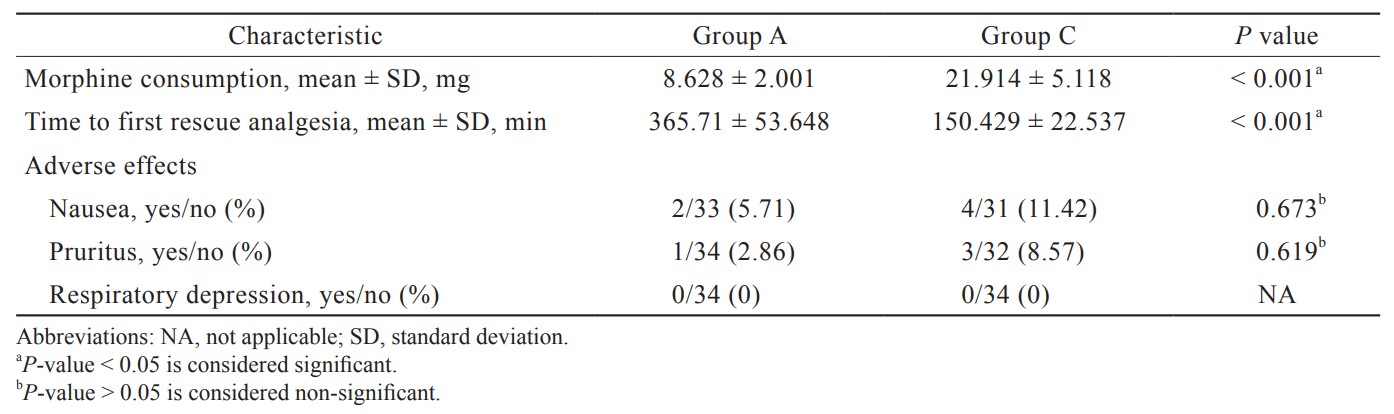
Both the groups exhibited similar patient characteristics like age, gender, weight, height, ASA physical status, and baseline vital parameters, and no significant difference was noted. The duration of surgery was also comparable between the groups (Table 1). The morphine consumption was lesser in group A (8.628 ± 2.001 mg) than in group C (21.914 ± 5.118 mg) with a highly significant statistical difference (
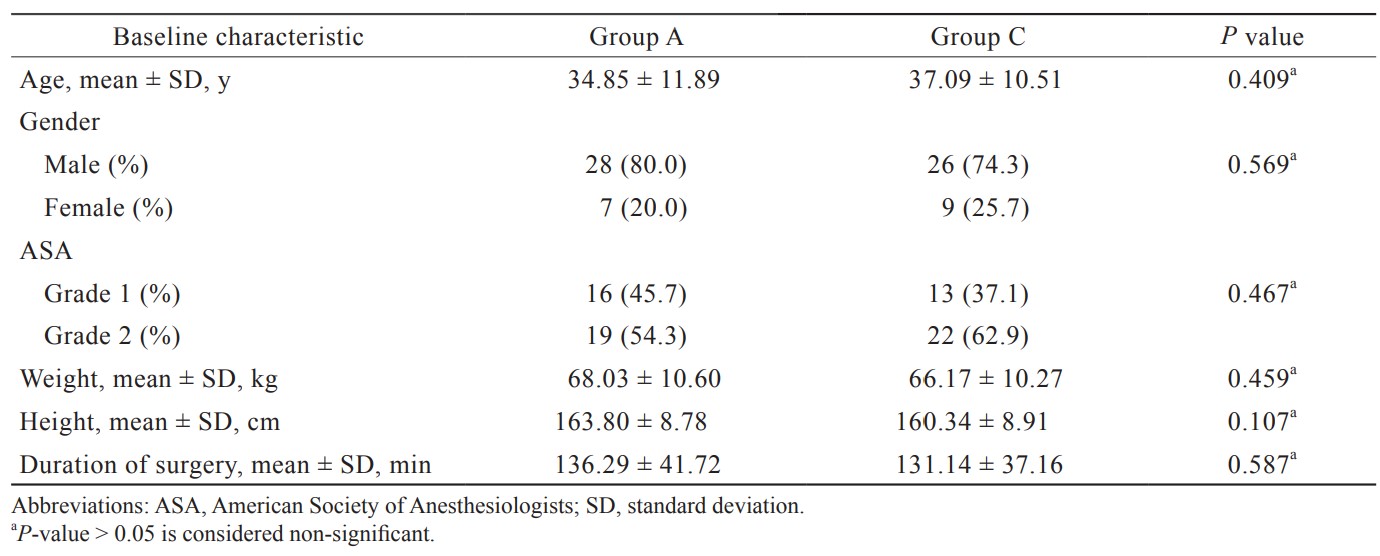
Download full-size image
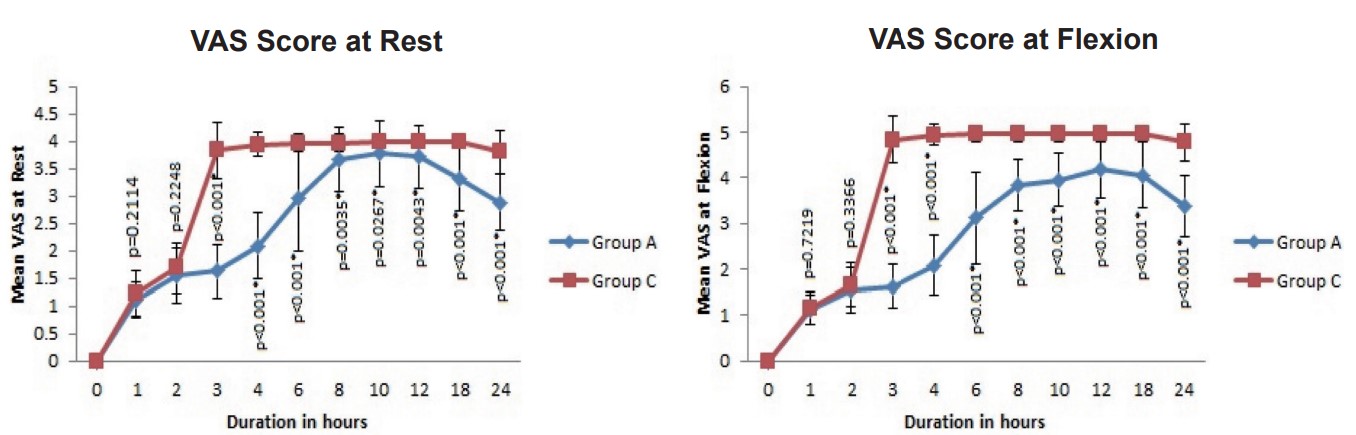
The average VAS scores at rest were significantly lesser in group A between 3 and 24 hours in the postoperative period (
Download full-size image
*
Download full-size image
*
Download full-size image
Discussion
ACB is a motor sparing block, useful as an alternative to the femoral nerve block. It blocks the saphenous nerve and nerve to vastus medialis traversing the adductor canal which is located in the middle third of medial half of the thigh.5 It blocks the femoral nerve after most of the motor branches of quadriceps muscles have left providing anesthesia and analgesia for surgeries involving anterior part of the knee.6 Therefore, ACB results in early mobilization following surgeries.7
We evaluated the efficacy of ACB in providing postoperative analgesia in this study. Our primary objective was to compare morphine consumption during the postoperative period. In group A, the mean morphine consumption was 8.628 ± 2.001 mg, and that of group C was 21.914 ± 5.118 mg over 24 hours. Group A had a significantly lesser consumption of morphine than group C. In a study by Jaeger et al.8 on knee replacement surgeries, the amount of morphine consumption was reduced in ACB group compared to control group (18 ± 11 mg vs. 28 ± 21 mg) which was correlating to our study. The reduction of morphine consumption by ACB was consistently proven in various other studies on knee surgeries.9-11
We found that the mean VAS scores at rest were significantly decreased in group A from 2 to 24 hours than in group C. This may be due to the effect of spinal anesthesia in both the groups during the initial 2 hours. Grevstad et al.12 and Kukreja et al.13 have also demonstrated the significant reduction of VAS scores at rest in patients who underwent knee surgeries under spinal anesthesia and general anesthesia, respectively. The reduction in VAS scores by ACB was found to be comparable to the analgesia provided by femoral nerve block,13 periarticular infiltration of local anesthetics,14 and epidural analgesia.15 In our study, there was a significant reduction in VAS pain scores at flexion from 2 to 24 hours in group A when VAS pain scores at flexion from 2 to 24 hours in group A was compared with one in group C. Similar results were obtained in various other studies on knee arthroplasty patients regarding the reduction of VAS scores during flexion. ACB was found to reduce VAS scores during movement comparable to femoral nerve block by Tan et al.16 and superior to local infiltration anesthesia (LIA) by Kampitak et al.17 in patients who underwent total knee arthroplasty. Even though there are many studies on ACB, the time to first request for analgesia was not evaluated. We found a significantly longer duration to request for analgesia in patients who received ACB (365.71 ± 53.648 min) compared to the control group (150.429 ± 22.537 min). There was a significant difference in the hemodynamic parameters during the postoperative period (approximately 2–8 hours) which was due to the effective analgesia provided by the ACB accounting for better trends in group A.
Since the block was performed under ultrasound guidance, the safety profile was high, and there were no block related adverse effects as in various other studies by Goyal et al.,18 Hanson et al.,11 and Tan et al.16
No statistically significant difference between groups A and C related to morphine infusion was seen concerning nausea (
There are a few limitations in our study. Double blinding was not done because the control group received no placebo injection. Quadriceps muscle strength was not assessed and compared in our study. There is future scope for comparing the ACB with other regional anesthetic techniques in knee surgeries.
Conclusions
Ultrasound-guided ACB resulted in significantly lesser morphine consumption after arthroscopic knee surgeries. ACB considerably prolonged the duration of analgesia with better hemodynamics, lesser VAS pain scores at rest and knee flexion. There were no complications related to block in our study.
References
| 1 |
Ho KY, Gwee KA, Cheng YK, Yoon KH, Hee HT, Omar AR.
Nonsteroidal anti-inflammatory drugs in chronic pain: implications of new data for clinical practice.
J Pain Res. 2018;11:1937-1948.
|
| 2 |
Garimella V, Cellini C.
Postoperative pain control.
Clin Colon Rectal Surg. 2013;26(3):191-196.
|
| 3 |
Paul JE, Arya A, Hurlburt L, et al.
Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trials.
Anesthesiology. 2010;113(5):1144-1162.
|
| 4 |
Jiang X, Wang QQ, Wu CA, Tian W.
Analgesic efficacy of adductor canal block in total knee arthroplasty: a meta-analysis and systematic review.
Orthop Surg. 2016;8(3):294-300.
|
| 5 |
Rasouli MR, Viscusi ER.
Adductor canal block for knee surgeries: an emerging analgesic technique.
Arch Bone Jt Surg. 2017;5(3):131-132.
|
| 6 |
Desai S.
Subsartorial (adductor canal block).
https://www.euroespa.com/wp-content/uploads/2018/01/adductor-canal-block.pdf.. Accessed October 25, 2020.
|
| 7 |
Karkhur Y, Mahajan R, Kakralia A, Pandey AP, Kapoor MC.
A comparative analysis of femoral nerve block with adductor canal block following total knee arthroplasty: a systematic literature review.
J Anaesthesiol Clin Pharmacol. 2018;34(4):433-438.
|
| 8 |
Jaeger P, Grevstad U, Henningsen MH, Gottschau B, Mathiesen O, Dahl JB.
Effect of adductor-canal-blockade on established, severe post-operative pain after total knee arthroplasty: a randomised study.
Acta Anaesthesiol Scand. 2012;56(8):1013-1019.
|
| 9 |
Jæger P, Koscielniak-Nielsen ZJ, Schrøder HM, et al.
Adductor canal block for postoperative pain treatment after revision knee arthroplasty: a blinded, randomized, placebo-controlled study.
PLoS One. 2014;9(11):e111951.
|
| 10 |
Jenstrup MT, Jæger P, Lund J, et al.
Effects of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: a randomized study.
Acta Anaesthesiol Scand. 2012;56(3):357-364.
|
| 11 |
Hanson NA, Allen CJ, Hostetter LS, et al.
Continuous ultrasound-guided adductor canal block for total knee arthroplasty: a randomized, double-blind trial.
Anesth Analg. 2014;118(6):1370-1377.
|
| 12 |
Grevstad U, Mathiesen O, Lind T, Dahl JB.
Effect of adductor canal block on pain in patients with severe pain after total knee arthroplasty: a randomized study with individual patient analysis.
Br J Anaesth. 2014;112(5):912-919.
|
| 13 |
Kukreja P, Bevinetto C, Brooks B, et al.
Comparison of adductor canal block and femoral nerve block for early ambulation after primary total knee arthroplasty: a randomized controlled trial.
Cureus. 2019;11(12):e6331.
|
| 14 |
Cicekci F, Yildirim A, Önal Ö, Celik JB, Kara I.
Ultrasound-guided adductor canal block using levobupivacaine versus periarticular levobupivacaine infiltration after total knee arthroplasty: a randomized clinical trial.
Sao Paulo Med J. 2019;137(1):45-53.
|
| 15 |
Alsheikh KA, Alkhelaifi AS, Alharbi MK, et al.
Adductor canal blockade versus continuous epidural analgesia after total knee joint replacement: a retrospective cohort study.
Saudi J Anaesth. 2020;14(1):38-43.
|
| 16 |
Tan Z, Kang P, Pei F, Shen B, Zhou Z, Yang J.
A comparison of adductor canal block and femoral nerve block after total-knee arthroplasty regarding analgesic effect, effectiveness of early rehabilitation, and lateral knee pain relief in the early stage.
Medicine (Baltimore). 2018;97(48):e13391.
|
| 17 |
Kampitak W, Tanavalee A, Ngarmukos S, Amarase C, Songthamwat B, Boonshua A.
Comparison of adductor canal block versus local infiltration analgesia on postoperative pain and functional outcome after total knee arthroplasty: a randomized controlled trial.
Malays Orthop J. 2018;12(1):7-14.
|
| 18 |
Goyal R, Mittal G, Yadav AK, Sethi R, Chattopadhyay A.
Adductor canal block for post-operative analgesia after simultaneous bilateral total knee replacement: a randomised controlled trial to study the effect of addition of dexmedetomidine to ropivacaine.
Indian J Anaesth. 2017;61(11):903-909.
|