Takotsubo syndrome (TTS) is an acute reversible heart failure syndrome first described in 1990 as hypokinesia or akinesia of the apical segment of the left ventricle.1 TTS was divided into primary and secondary types regarding their potential triggers. Patients with secondary TTS have identical clinical manifestations, but a 2- to 10-fold higher mortality rate compared to primary TTS.2 This report highlights the importance of secondary TTS, which may be elicited by exogenous (i.e., via direct injection) and/or endogenous epinephrine (most often caused by surgical stress).
An 82-year-old female with medically-controlled hypertension underwent scheduled tongue tumor excision. Anesthesia induction was achieved with fentanyl 25 mcg, lidocaine 50 mg, etomidate 13 mg, and cisatracurium 10 mg; the depth was maintained with sevoflurane 1.5%–2.0%. Fentanyl 25 mcg was administered once to manage an intraoperative hyperdynamic state after a local injection of 2% lidocaine 3 mL with 1:200,000 epinephrine for hemostatic prophylaxis. During surgery, her electrocardiogram (ECG) revealed a normal sinus rhythm. Fentanyl 50 mcg was again administered after surgery for postoperative pain control.
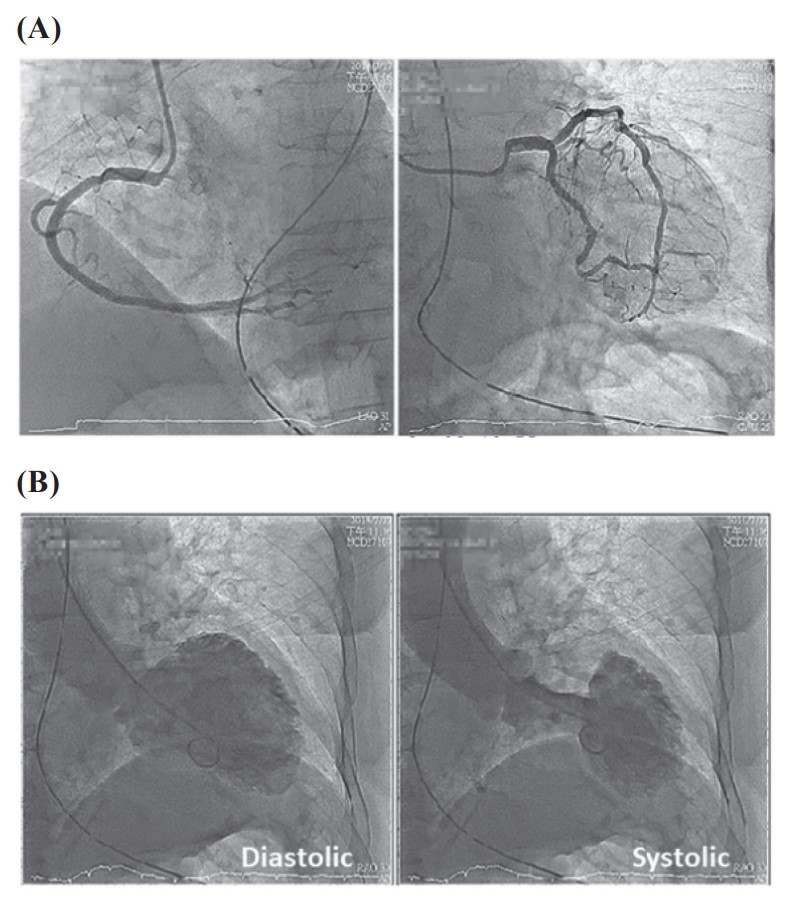
In the postanesthetic care unit, she developed sudden-onset chest tightness. Acute coronary work-up was done with 12-lead ECG revealing ST-segmental elevation in leads V2–V5; laboratory investigations showed elevation of serum troponin-I (3.032 ng/mL) levels. Under the tentative diagnosis of ST-segment elevation myocardial infarction, a cardiologist was consulted for emergent cardiac catheterization. However, no coronary artery stenosis was found (Figure 1A). The left ventriculography revealed a left ventricular apical ballooning pattern during both systolic and diastolic phases (Figure 1B); the diagnosis of TTS was made. After medical treatment, she was discharged under stable condition after 8 days of hospitalization. Unfortunately, the patient suffered from sudden cardiac arrest 40 days after the aforementioned operation.
Download full-size image
(A) A normal coronary angiography without significant stenosis; (B) A left ventricular apical ballooning pattern during systolic and diastolic phases on left ventriculography.
Yamamoto et al.3 described a 78-year-old woman scheduled for endoscopic sinus surgery. After a submucosal injection of 3 mL of 0.5% lidocaine with epinephrine (0.015 mg) immediately before the incision, ventricular tachycardia was found, and left ventriculography established the diagnosis of TTS. After treatment, the patient’s cardiac motion gradually improved, and she was discharged on postoperative day 9.
In the preoperative period, we emphasize the importance of maintaining pre-existing beta-blocker therapy and avoiding psychological stress. Moreover, intraoperative anesthetic goals should always include maintaining adequate anesthetic levels and stabilizing hemodynamic status. If hemodynamic instability or change in ECG is present, differentiating TTS from acute coronary syndrome (ACS) is important. Transthoracic or transesophageal echocardiography should be immediately performed. Early echocardiography in patients later to be found with TTS benefits both treatment and prognosis by identifying any potential complications (e.g., left ventricular outflow tract obstruction, reversible moderate to severe mitral regurgitation, and right ventricular involvement), and is crucial for the management and risk stratification.4 However, coronary angiography is usually still required to exclude ACS; since 10% of the cases with TTS have coexisting ACS, emergent coronary angiography may even be necessary.5
Being aware of the possibility of TTS when patients show symptoms and signs of ACS is important. The ability to differentiate TTS from ACS enables a different and more appropriate management approach.
Conflict of Interest
The authors declare no conflict of interest.
References
| 1 |
Lyon AR, Bossone E, Schneider B, et al.
Current state of knowledge on Takotsubo syndrome: a position statement from the Taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology.
Eur J Heart Fail. 2016;18(1):8-27.
|
| 2 |
Singh K, Carson K, Shah R, et al.
Meta-analysis of clinical correlates of acute mortality in takotsubo cardiomyopathy.
Am J Cardiol. 2014;113(8):1420-1428.
|
| 3 |
Yamamoto W, Nishihara T, Nakanishi K, et al.
Takotsubo cardiomyopathy induced by very low-dose epinephrine contained in local anesthetics: a case report.
Am J Case Rep. 2021;22:e932028.
|
| 4 |
Citro R, Lyon AR, Meimoun P, et al.
Standard and advanced echocardiography in takotsubo (stress) cardiomyopathy: clinical and prognostic implications.
J Am Soc Echocardiogr. 2015;28(1):57-74.
|
| 5 |
Kurisu S, Inoue I, Kawagoe T, et al.
Prevalence of incidental coronary artery disease in tako-tsubo cardiomyopathy.
Coron Artery Dis. 2009;20(3):214-218.
|