Abstract
Introduction
Decisions on appropriate time of extubation after pediatric neurosurgery are often challenging for anesthesiologists. The primary goal was to investigate the incidence of delayed extubation after pediatric neurosurgery. The secondary goal was to identify the factors affecting delayed extubation in these patients.
Methods
This retrospective study was done in pediatric patients who underwent neurosurgery at a university hospital in a 5-year period from April 2015 to March 2020. Delayed extubation was that the patients who were not extubated at the end of procedure before leaving the operating room. Demographic data, preoperative and intraoperative factors associated with delayed extubation were collected and analyzed.
Results
A total of 539 pediatric patients were included in our study. There were 56 children in delayed extubation group with the incidence of 10.4%. In the multivariate analysis, the factors associated with delayed extubation were including neonates (adjusted odds ratio [aOR], 3.743; 95% confidence interval [CI], 1.076–13.028), American Society of Anesthesiologists physical status III–IV (aOR, 3.010; 95% CI, 1.057–8.573), preoperative oxygen supplement (aOR, 6.033; 95% CI, 1.713–21.243), intracranial surgery (aOR, 4.494; 95% CI, 1.458–13.847), estimated blood loss (EBL) ≥ 40% of total blood volume (TBV) (aOR, 5.465; 95% CI, 1.640–18.210), and finishing operation after official hours (aOR, 3.810; 95% CI, 1.633–8.889).
Conclusions
There were the preoperative and intraoperative factors associated with delayed extubation such as preoperative oxygen supplement, intracranial surgery, or EBL ≥ 40% of TBV. These might be useful for anesthesiologists in making decisions about the planning of extubation after neurosurgery in children.
Keywords
delayed extubation, neurosurgery, pediatric
Introduction
Decisions on appropriate time of extubation at the end of pediatric neurosurgery are often challenging for anesthesiologists. Early emergence and tracheal extubation after anesthesia can help facilitate rapid neurological assessment for early diagnosis of postoperative complications. It can also improve patient outcomes and lower stress response measured by noradrenaline blood level.1,2 An important consideration of early extubation in pediatric neurosurgery is the drawbacks of failed extubation including hypercarbia, intracranial hypertension, and aspiration which can affect neurological outcomes. Reintubation is associated with increased length of intensive care unit (ICU) and hospital stay, increased mortality, prolonged duration of mechanical ventilation, increased tracheostomy rate, and higher hospital costs.3
Many studies have demonstrated factors associated with immediate extubation after pediatric cardiac surgery.4-6 Other studies have demonstrated factors that influence delayed extubation in the neurosurgical patients such as age, total fluid volume administered, estimated blood loss (EBL), duration of surgery, and operation end time after official hours.7-9 There are several differences between pediatric and adult in neurological anesthesia such as the incidence of disease, location of tumor, anatomy and physiology of brain, airway and respiration which affects the anesthesia techniques as well as surgical outcomes. For pediatrics, it has been suggested that candidates for delayed extubation include preoperative altered mental status, longer duration of surgery (> 6 hours), large tumor resection, injury to cranial nerve (especially cranial nerves IX, X, XII), complications during surgery, intraoperative brain swelling, and hypothermia.10
The principal goal of this study was to investigate the incidence of delayed extubation in neurosurgery among pediatric patients. The secondary goal was to identify the factors associated with delayed extubation in these patients. Results can help guide anesthesiologists make better decisions for safe extubation and minimize complications of failed extubation.
Methods
This retrospective study was approved by the Chulalongkorn University Institutional Review Board (IRB No.734/63). The authors reviewed pediatric patient medical records (0–15 years old) who underwent neurosurgery at King Chulalongkorn Memorial Hospital in a 5-year period from April 2015 to March 2020. The exclusion criteria were patients with preoperative intubation or tracheostomy, patients scheduled for tracheostomy following the operation, episode of repeated operation within 7 days, anesthesia without endotracheal tube, and incomplete medical data. Delayed extubation was defined as a patient who was not extubated at the end of the procedure before leaving the operating room. These patients were sent to ICU and ventilated with mechanical ventilation. In addition to patient characteristics, factors associated with delayed extubation were divided into two types. The first type was preoperative factors including history of prematurity, coexisting cardiac anomalies, coexisting respiratory diseases, failure to thrive, delayed development, American Society of Anesthesiologists (ASA) classification, preoperative oxygen supplements, type of operation (intracranial or spinal surgery), and undergoing multiple operations during the same admission. The second set was intraoperative factors including anesthesia technique, opioid dosage, ease of airway management, intraoperative cardiovascular events including hypotension with or without vasopressor/inotropic agent required and bradycardia required atropine, EBL, volume of fluid administration, blood components administration, body position during the procedure, duration of surgery, body temperature at emergence phase, and operation end time after official hours.
Factor definitions included: (1) prematurity was defined as a patient born before 37 weeks of pregnancy, and (2) failure to thrive denoted weight less than the third percentile for age. Coexisting cardiac anomalies were classified in three groups: no risk, minor risk (cardiac condition with or without medication and maintenance or status post repair congenital heart disease with normal cardiovascular function), and major risk (status post repair congenital heart disease with residual hemodynamic abnormality, uncorrected cyanotic heart diseases or congestive heart failure). Coexisting respiratory diseases included bronchopulmonary dysplasia, respiratory distress syndrome, and obstructive sleep apnea. Patients who received supplementary preoperative oxygen delivered by any modality for any reasons were included as an associated factor. Hypotension was defined as a decrease in blood pressure of more than 20% from baseline. Estimated total blood volume (TBV) of children was referred from standard textbook.11 Massive blood transfusion was defined as administering blood totaling > 100% of TBV during the operation.
We analyzed differences in clinical outcomes between two groups including length of ICU and hospital stay, discharge status, and airway status at discharge. The incidence of reintubation within 72 hours in immediate extubation group and time to extubation in delayed extubation group were also collected.
In the analysis, our estimated sample size was calculated as 437 patients based on a 17% rate of delayed extubation in pediatric neurosurgery found in our pilot observational study, 95% confidence interval (CI) and 20% acceptable relative error of incidence. Categorical variables were represented by number and percentage (%). Continuous variables were represented as mean and standard deviations (mean ± SD) or median and range (min–max). Univariate analysis was used for comparing two categorical variables via chi-square test or Fisher’s Exact test, and two continuous variables were tested by independent sample
Results
A total of 539 pediatric patients were included in our study. The mean age of our patients was 5.5 ± 4.9 years including 130 patients (24.1%) less than 1 year old. The majority of patients were ASA physical status I–II (89.4%), elective surgery (88.1%), and intracranial procedures (78.3%). Two patients underwent both ventriculoperitoneal shunt and lumbo-sacral myelomeningocele repair procedure simultaneously. Intracranial procedures included craniotomy or craniectomy (44.1%), shunt procedure included burr hole (40.3%), cranial reconstruction (12.3%) and other procedures such as wound debridement or transsphenoidal pituitary surgery (3.3%). The majority of spinal procedures were thoraco-lumbo-sacral spine (86.1%). The duration of surgery was 177.7 ± 121.7 minutes. Most patients were anesthetized by inhalation (90.2%) and operated in supine position (56.8%). Fentanyl was administrated in 517 patients (95.9%) and the mean of dosage was 0.89 ± 0.65 mcg/kg/hr. Mean volume of crystalloid, blood components administration, and EBL were 29.5 ± 24.1 mL/kg, 75.7 ± 339.0 mL, and 169.7 ± 364.9 mL, respectively. Only 9.7% of children were hypothermic with a body temperature of less than 35°C. Two hundred and ten procedures (39%) were finished after regular office hours. Postoperative ICU admission requirement was 58.3%.
The incidence of delayed extubation group was 10.4%. The preoperative factors which had statistically significant differences were age group, body weight, preoperative oxygen supplement, coexisting respiratory diseases, and intracranial surgery (Table 1). The intraoperative factors included positioning, intraoperative cardiovascular event, dose of fentanyl, massive blood transfusion, volume of blood components, crystalloid and colloid administration, duration of surgery, and operation end time after official hours were significantly associated with delayed extubation group (Table 2). All 5 patients with massive blood transfusion remained intubation at the end of surgery. In the multivariate logistic regression model, age ≤ 1 month old, ASA physical status III–IV, preoperative O2 supplement, intracranial surgery, EBL ≥ 40% of TBV and operation end time after official hours were the statistically significant factors associated with delayed extubation after pediatric neurosurgery (Table 3). Body weight, coexisting respiratory diseases, operative time ≥ 120 minutes, intraoperative cardiovascular event, prone position, crystalloid ≥ 50 mL/kg administered, colloid ≥ 10 mL/kg administered, blood transfusion, and dose of fentanyl were not found significant in the multivariate logistic regression.
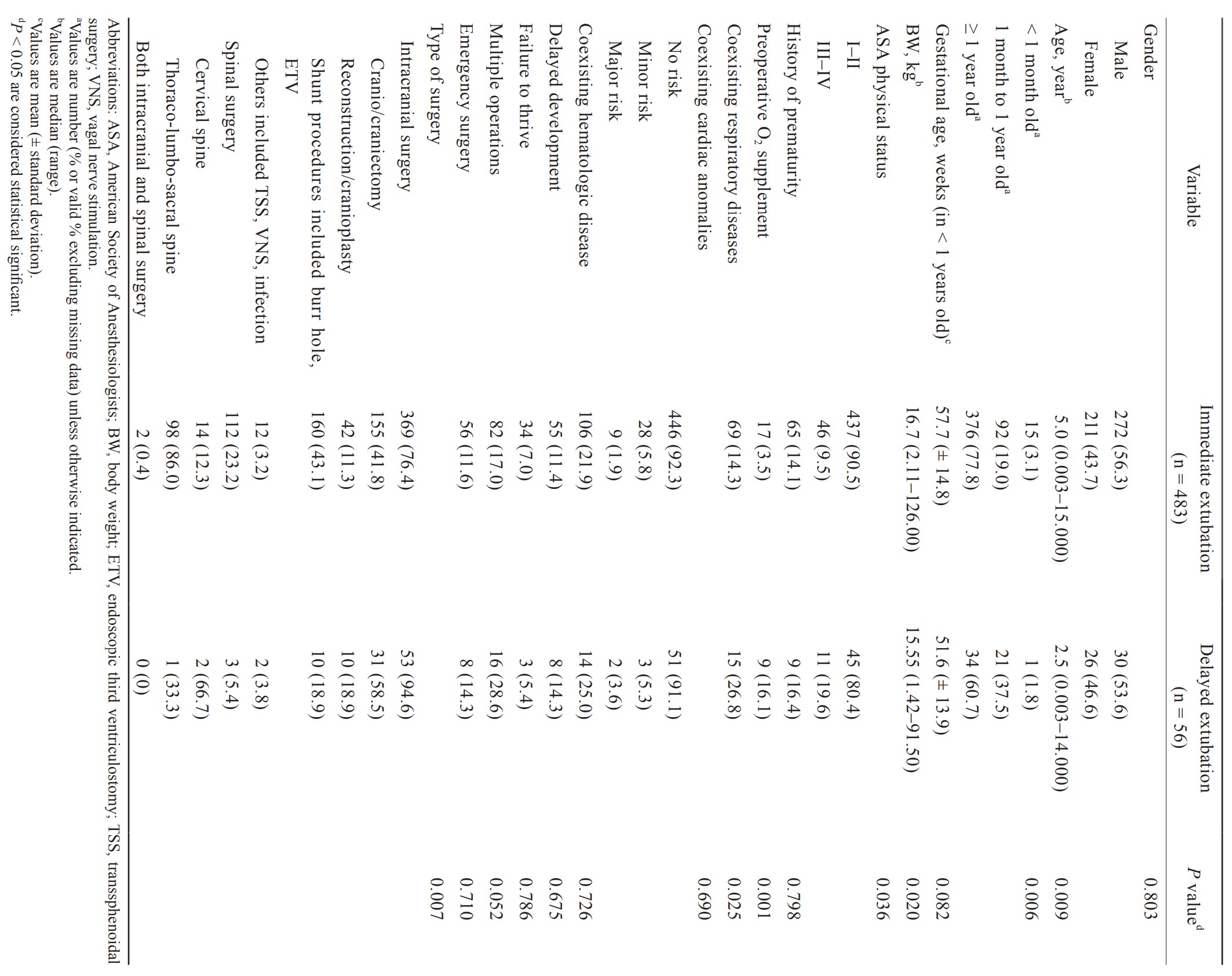
Download full-size image
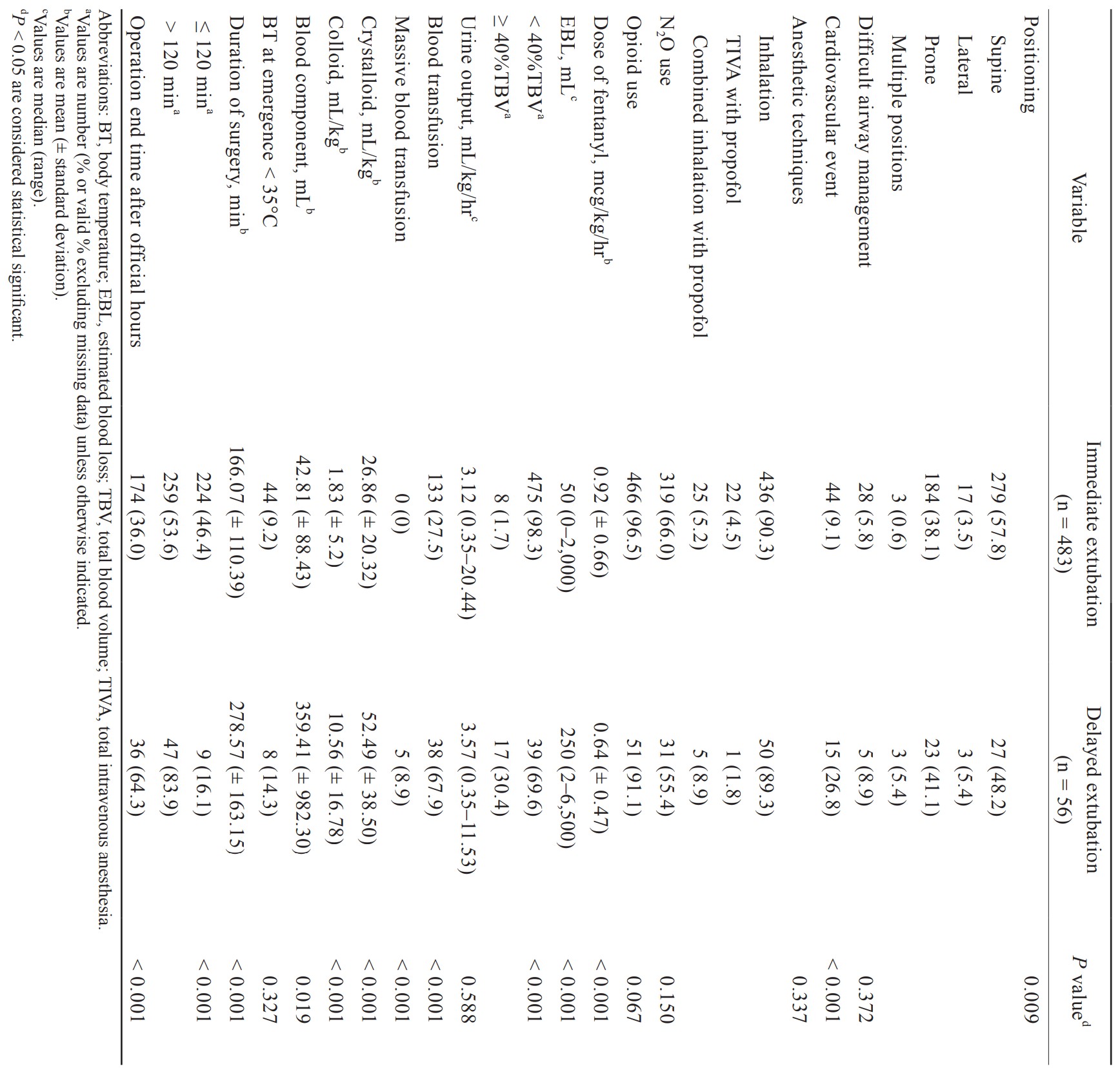
Download full-size image
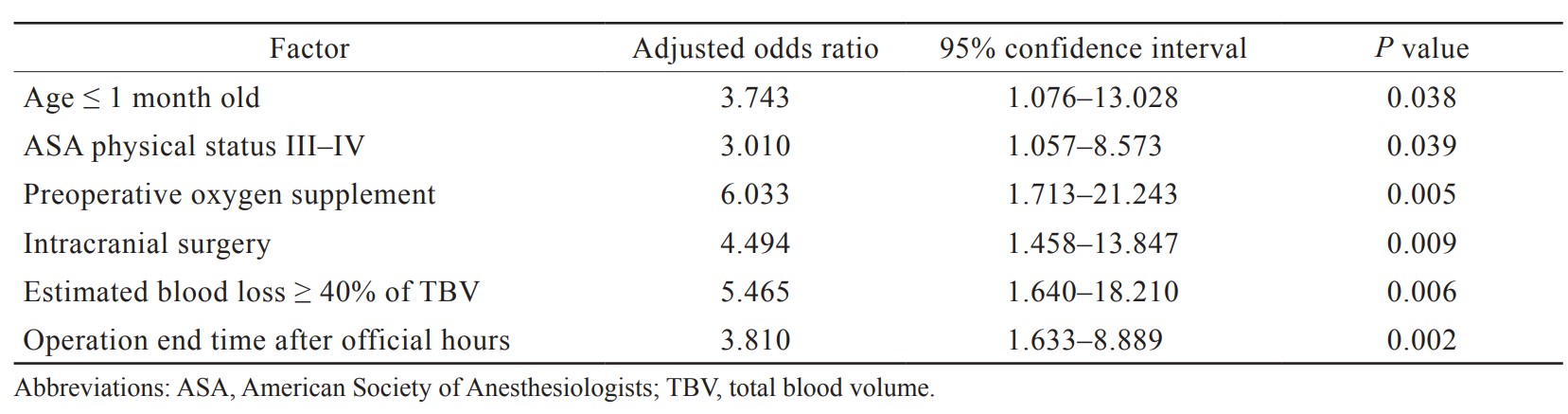
Download full-size image
Outcomes including length of ICU stay, length of hospital stay, discharge status, and airway status at discharge showed statistically significant differences between immediate and delayed extubation groups (Table 4).
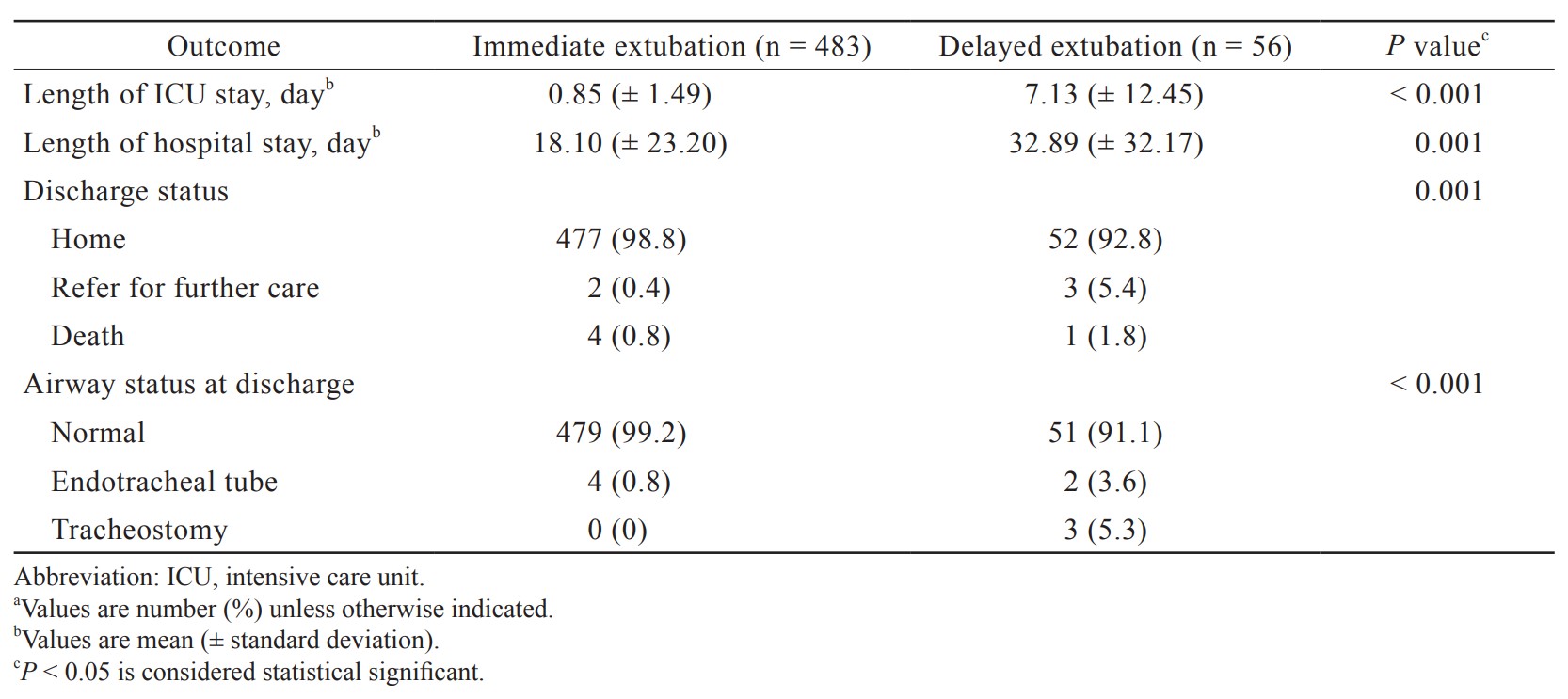
Download full-size image
The incidence of reintubation in the immediate extubation group was 1%. The causes of reintubation included opioid overdose, apnea due to brainstem swelling, seizure, and desaturation. In the delayed extubation group, the majority of cases were extubated successfully within 1 day after surgery (76.8%). The mean of time to extubation which excluded data from 1 patient who was extubated on day 21 after surgery and 3 patients who had tracheostomy or intubation on discharge was 25.0 ± 28.1 hours (range 0.5–164.1 hours).
Discussion
Our retrospective study found an incidence rate of delayed extubation after pediatric neurosurgery of 10.4%. Previous levels of incidence found in adult studies range from 10.9% to 44.0% and varied depending on procedure definitions and type of neurosurgery.7-9 We also found that the delayed extubation group was associated with a longer length of ICU and hospital stay, increased mortality and discharged with tracheostomy. The delayed extubation patients tended to need high-dependency care which is important information to relay to parents in preparation for post-discharge care.
From the present study, neonates, ASA physical status III–IV, preoperative oxygen supplement, intracranial surgery, EBL ≥ 40% of TBV, and operation end time after office hours were independent predictive factors of delayed extubation. All children who had massive blood transfusion remained intubated.
A number of studies have demonstrated that younger age was a determinant of time to extubate after cardiothoracic surgery and associated with postoperative reintubation, especially in neonates.4,12,13 Our study also showed that age ≤ 1 month old was a predictor for delayed extubation after neurosurgery. Several factors have been found associated with keeping the endotracheal tube in the neonate after surgery including immaturity of pulmonary system, risk of postoperative apnea in preterm infants, prolonged anesthetic effect due to the differences of pharmacokinetic and pharmacodynamics in neonate.13,14 Additionally, assessment of awakening from anesthesia might be difficult in neurosurgical procedures among this population.
Similarly, poorer ASA physical status (III–IV) was recognized as an independent predictor of delayed extubation in our study which was also found in a previous adult intracranial study.7 Cheon et al.13 reported that the risk of postoperative reintubation increased in patients with ASA physical status II–V.
The present study demonstrated a significant association between delayed extubation after pediatric neurosurgery and preoperative oxygen supplements such as oxygen box, cannula, and positive airway pressure devices (BiPAP, CPAP). The oxygen therapy was used for optimizing medical conditions such as respiratory diseases or neonatal status. The relationship between preoperative oxygen supplement and determinants of delayed extubation in pediatric patient is not well-defined. It may be related to impaired pulmonary function of patients or the inflammatory process from oxidative stress of oxygen therapy.15 Nevertheless, our study failed to show that preoperative coexisting respiratory disease was the factor associated with the time to extubate, even though it is well-known that patients with coexisting respiratory diseases increase the risk of perioperative respiratory complications.16
It was notable that the number of patients who had multiple operations in the same admission was higher in delayed extubation group compared to the immediate extubation group, although statistically significance was barely missed (
Not surprisingly, intracranial procedures were reported as a predictive factor for delayed extubation. The surgeries involving brainstem function and cranial nerve nuclei could be the cause of the respiratory drive depression and increased risk of aspiration. Most of these patients required intubation for postoperative mechanical ventilation.17 Some patients who undergo intracranial surgery might suffer from postoperative brain edema and need intubation in order to control ventilation. Our study also showed that cervical spinal surgery was more common in delayed extubation compared to thoraco-lumbo-sacral spinal surgery. The causes are airway edema from retraction during anterior cervical surgery, venous congestion from prone positioning and intravenous fluid administration during posterior cervical surgery.8 Moreover, upper cervical surgery might also cause diaphragm dysfunction.
The results of our study revealed that EBL ≥ 40% of TBV was a significant predictive factor for delayed extubation. It is the common practice of pediatric anesthesiologists to determine volume of intraoperative blood loss and volume of fluid and blood components administration for the time to extubate after surgery. Owing to these possible consequences, intraoperative cardiovascular instability, uncertainty of volume status, and postoperative fluid shifting were of concern. Anesthesiologists tend to keep the endotracheal tube in patients who have these intraoperative events. We raised the concern that how high of a threshold of EBL would impact the decision of anesthesiologists. We decided to study a threshold of 40% of TBV because physiological reserve in pediatric patients was good and they could maintain blood pressure even after a loss of 25%–40% of TBV.18 We assumed that bleeding beyond this level might affect the time to extubation. Moreover, the massive blood transfusion increases morbidity and mortality in pediatric patients from allergic reaction, metabolic derangements, and immunologic complications especially transfusion-related acute lung injury.18 All children who had massive blood transfusion had their intubation retained at the end of surgery. Delayed extubation in these patients might be reasonable, although we could not show the statistical significance in the multivariate logistic regression analysis.
Furthermore, the operation end time after official hours was found to be a significant predictor of delayed extubation in the present study similar to previous studies.8,9 During the night shift, there are several limitations such as fewer and less experienced providers, decreased resource availability, and more exhausted medical personals. These factors might affect an anesthesiologist’s decision to retain intubation particularly after prolonged surgery. Scheduling operations to finish during office hours might improve patient safety and effective resource utilization.
By comparison, some studies have suggested that anesthetic drugs and dosage levels might have an influence on determination of delayed extubation.4,5,7 Our study results found that anesthetic techniques (inhalation or total intravenous anesthesia), nitrous oxide uses, opioid uses were not associated with delayed extubation. Fentanyl did show statistical significance in the univariate model, but it did not retain significance in the multivariate analysis. We also hypothesized that prone position and large volume of crystalloid/colloid administration would be a predictor of delayed extubation because of the possibility of significant airway edema and postoperative airway obstruction.9,19 We failed to show this relationship in our data. Moreover, intraoperative adverse events such as difficult airway management, cardiovascular instability, and hypothermia were factors found in the literature.4,7 However, our results did not demonstrate any association. These might be due to the variety of patients’ age and the heterogeneity of procedures in the previous studies which are different from our population in this study.
We identified several limitations in our study. Firstly, this is a retrospective study which might be influenced by inherent bias. Secondly, the related factors were driven by decisions of individual anesthesiologists which may vary based on their experience. Thirdly, we did not specify the pathology of diseases such as tumor or vascular diseases or the location of intracranial surgery such as supratentorial or infratentorial regions. These factors might also influence extubation decisions. Analysis of a prospective case-controlled study may improve accuracy of the predictive factors associated with delayed extubation in pediatric neurosurgery.
Conclusions
The incidence of delayed extubation after pediatric neurosurgery was 10.4% in our university hospital. The independent predictive factors were neonates, ASA physical status III–IV, preoperative oxygen supplement, intracranial surgery, EBL ≥ 40% of TBV, and operation end time after official hours. These data might be useful for anesthesiologists in making decisions on the planning of extubation after neurosurgery in children, to inform parents about the possibility of the endotracheal tube remaining after surgery, and to prepare necessary postoperative equipment.
Acknowledgments
The manuscript was edited language by the English editing service, Research Affairs, Faculty of Medicine, Chulalongkorn University.
Conflict of Interest
The authors have no conflicts of interest to declare.
References
| 1 |
Bruder NJ.
Awakening management after neurosurgery for intracranial tumours.
Curr Opin Anaesthesiol. 2002;15(5):477-482.
|
| 2 |
Bruder N, Stordeur JM, Ravussin P, et al.
Metabolic and hemodynamic changes during recovery and tracheal extubation in neurosurgical patients: immediate versus delayed recovery.
Anesth Analg. 1999;89(3):674-678.
|
| 3 |
Rothaar RC, Epstein SK.
Extubation failure: magnitude of the problem, impact on outcome, and prevention.
Curr Opin Crit Care. 2003;9(1):59-66.
|
| 4 |
Tirotta CF, Alcos S, Lagueruela RG, et al.
Three-year experience with immediate extubation in pediatric patients after congenital cardiac surgery.
J Cardiothorac Surg. 2020;15(1):1.
|
| 5 |
Yu AL, Cai XZ, Gao XJ, et al.
Determinants of immediate extubation in the operating room after total thoracoscopic closure of congenital heart defects.
Med Princ Pract. 2013;22(3):234-238.
|
| 6 |
Varghese J, Kutty S, Abdullah I, Hall S, Shostrom V, Hammel JM.
Preoperative and intraoperative predictive factors of immediate extubation after neonatal cardiac surgery.
Ann Thorac Surg. 2016;102(5):1588-1595.
|
| 7 |
Nivatpumin P, Srisuriyarungrueng S, Saimuey P, Srirojanakul W.
Factors affecting delayed extubation after intracranial surgery in Siriraj Hospital.
Siriraj Med J. 2010;62(3):119-123.
|
| 8 |
Raksakietisak M, Keawsai T, Sirivanasandha B.
Factors related to delayed extubation in cervical spine surgery in an academic hospital: a retrospective study of 506 patients.
Asian J Anesthesiol. 2019;57(4):111-116.
|
| 9 |
Anastasian ZH, Gaudet JG, Levitt LC, Mergeche JL, Heyer EJ, Berman MF.
Factors that correlate with the decision to delay extubation after multilevel prone spine surgery.
J Neurosurg Anesthesiol. 2014;26(2):167-171.
|
| 10 | |
| 11 |
Deutsch N, Ohliger S, Motoyama EK, Cohen IT.
Induction, maintenance, and recovery.
|
| 12 |
Halimić M, Dinarević SM, Begić Z, Kadić A, Pandur S, Omerbašić E.
Early extubation after congenital heart surgery.
J Health Sci. 2014;4(3):156-161.
|
| 13 |
Cheon EC, Palac HL, Paik KH, et al.
Unplanned, postoperative intubation in pediatric surgical patients: development and validation of a multivariable prediction model.
Anesthesiology. 2016;125(5):914-928.
|
| 14 | |
| 15 |
Walsh BK, Smallwood CD.
Pediatric oxygen therapy: a review and update.
Respir Care. 2017;62(6):645-661.
|
| 16 |
Cladis FP, Davis PJ.
Preoperative preparation.
|
| 17 |
Rath GP, Dash HH.
Anaesthesia for neurosurgical procedures in paediatric patients.
Indian J Anaesth. 2012;56(5):502-510.
|
| 18 | |
| 19 |
Vavilala MS, Sariano SG, Krane EJ.
Anesthesia for neurosurgery.
In: David PJ, Cladis FP, eds. Smith’s Anesthesia for
|