Abstract
The proportion of women taking up anesthesiology and critical care as their careers has increased considerably in the last decade. Currently, women constitute 35%–40% of the total anesthesia workforce in some countries. Most resident doctors and a significant proportion of practicing physicians in anesthesia are in the reproductive age group. They are or will become pregnant at some point in their training program or career. This review focuses on all work-related exposure risks for anesthesia professionals during pregnancy, like risks of infectious diseases, radiation, stress, violence against doctors, and even peer support that can have deleterious effects on the health of pregnant physicians and the health of their unborn fetus. An occupational work environment more compatible with pregnancy is the need of the hour.
Keywords
anesthesia professionals, health care workers, occupational risks, pregnancy, radiation exposure, teratogenesis, violence against doctors
Introduction
The proportion of women in the healthcare workforce has been continuously increasing worldwide. Approximately 75% of the global health workforce are women, and almost 90% of the proportion of these women are nursing and midwifery professions. The proportion of women taking up anesthesiology and critical care as their careers has increased considerably in the last decade. Currently, women constitute 35%–40% of the total anesthesia workforce in the United Kingdom and the United States of America.1,2 Most resident doctors and a significant proportion of practicing physicians in anesthesia are in the reproductive age group. They are or will become pregnant at some point in their training program or career. Many countries have implemented workplace regulations to protect pregnant women and their children from occupational risks and arduous activities. Still, these are mainly lacking in low- and middle-income countries like India.
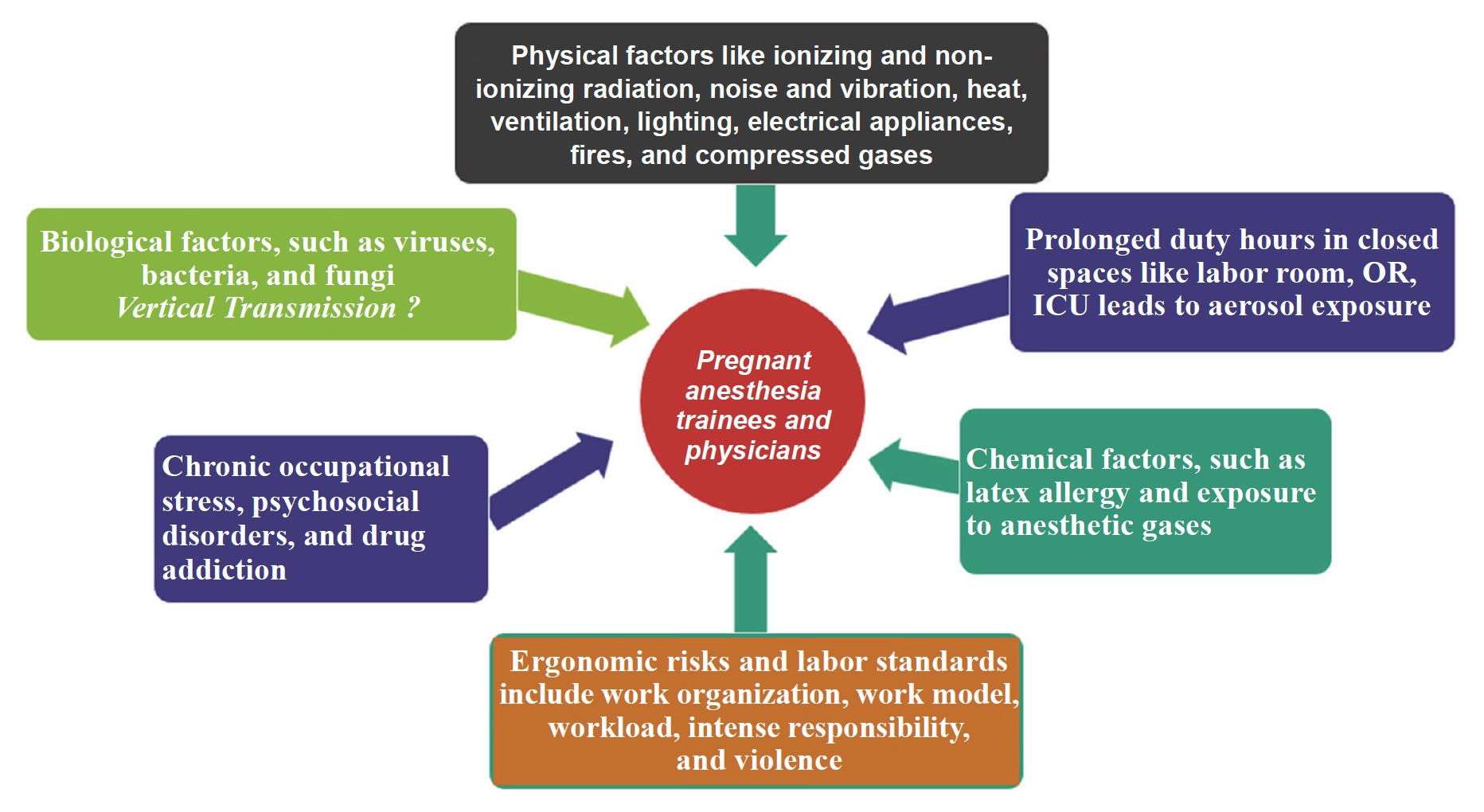
Pregnant healthcare workers, including anesthetists, face numerous challenges as they need to balance their health and the health of their unborn children along with their patients (Figure 1). Proper disposal of their duties may, at times, be a risk to their health. Although pregnant women are not more susceptible to the majority of diseases as compared to their non-pregnant counterparts, the consequences of even a mild infection can be far-reaching. Although mostly self-limiting rubella and chickenpox can lead to abortions and congenital abnormalities in the offspring if acquired during the first trimester of pregnancy. It is common for a female health care worker to feel torn between duties towards her patients and co-workers and her responsibilities towards her family and her unborn fetus. A pregnant trainee or even a consultant physician in anesthesia faces unique occupational challenges and hazards. Apart from the physically taxing nature of work in the operating room (OR), where each surgery needs continuous monitoring and vigilance for at least 6–8 hours, several other occupational risks are unique to the speciality, which probably at the time of pregnancy need a particular concern.
Download full-size image
Abbreviations: ICU, intensive care unit; OR, operating room.
Download full-size image
To the best of our knowledge, there is no comprehensive review that identifies occupational risks to pregnant anesthesia professionals. This review focuses on all work-related exposure risks, like risks of infectious diseases, radiation, stress, violence against doctors, and even peer support that can have deleterious effects on pregnant physicians’ health and their unborn fetuses’ health.
Methods
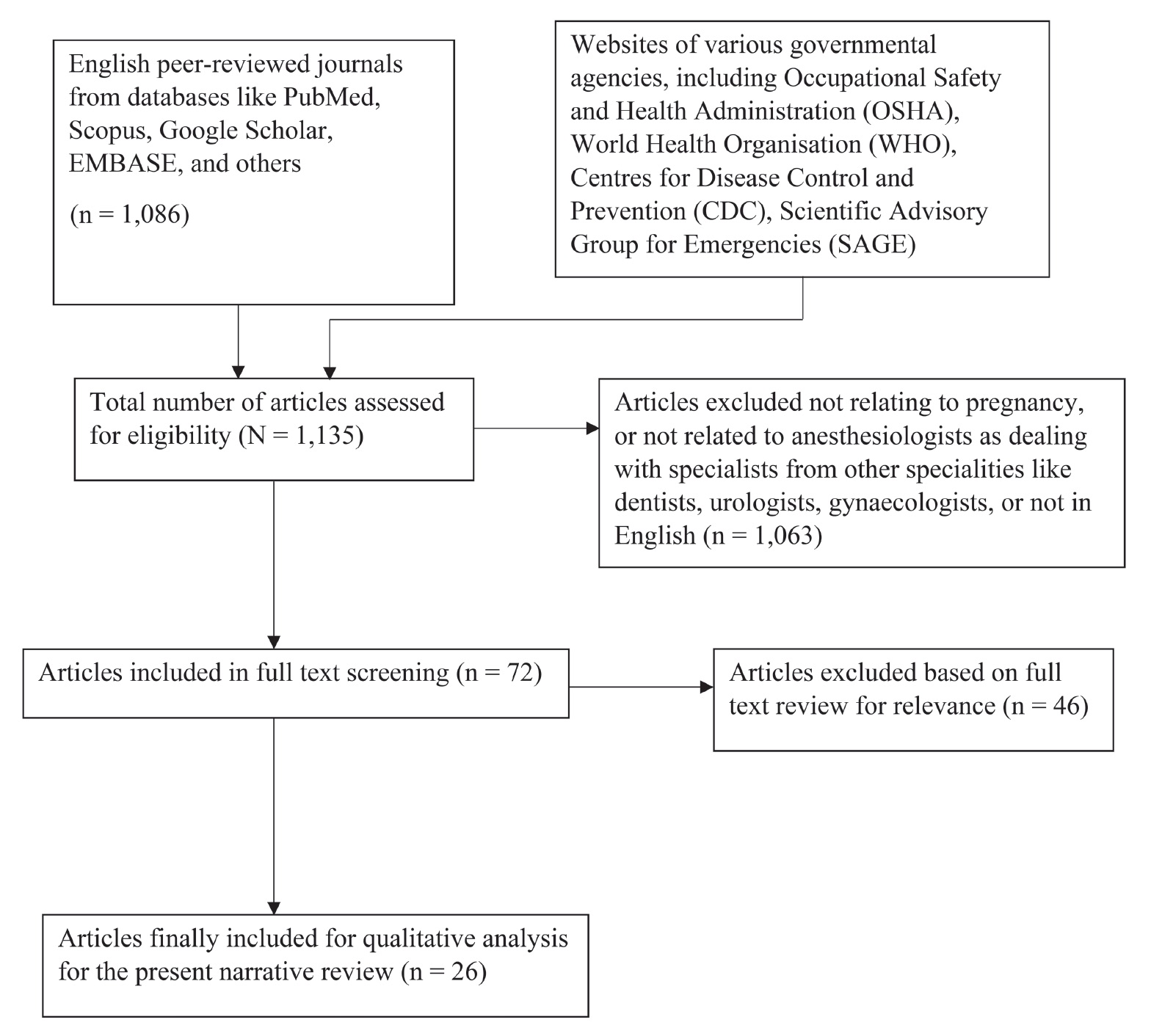
The recent literature related to the pregnant health care worker and occupational risks was searched from the websites of various governmental agencies, including Occupational Safety and Health Administration (OSHA), World Health Organisation (WHO), Centers for Disease Control and Prevention (CDC), Scientific Advisory Group for Emergencies, and English peer-reviewed journals from databases like PubMed, Scopus, Google Scholar, EMBASE, and others. The literature regarding workplace regulations for pregnant health care staff was also reviewed. The search terms used were: “pregnant health care worker” AND “occupational risks”; OR “radiation exposure”; OR “violence against doctors”; OR “infectious diseases” OR “physician burnout or stress”; OR “anaesthetic gases”. The articles referring to anesthesia trainees and physicians were studied in detail to identify the occupational risks that they face during pregnancy. The reference lists of all articles discovered in these searches were also examined for additional references. The flowchart for articles selected for the present narrative review is given in Figure 2.
Results
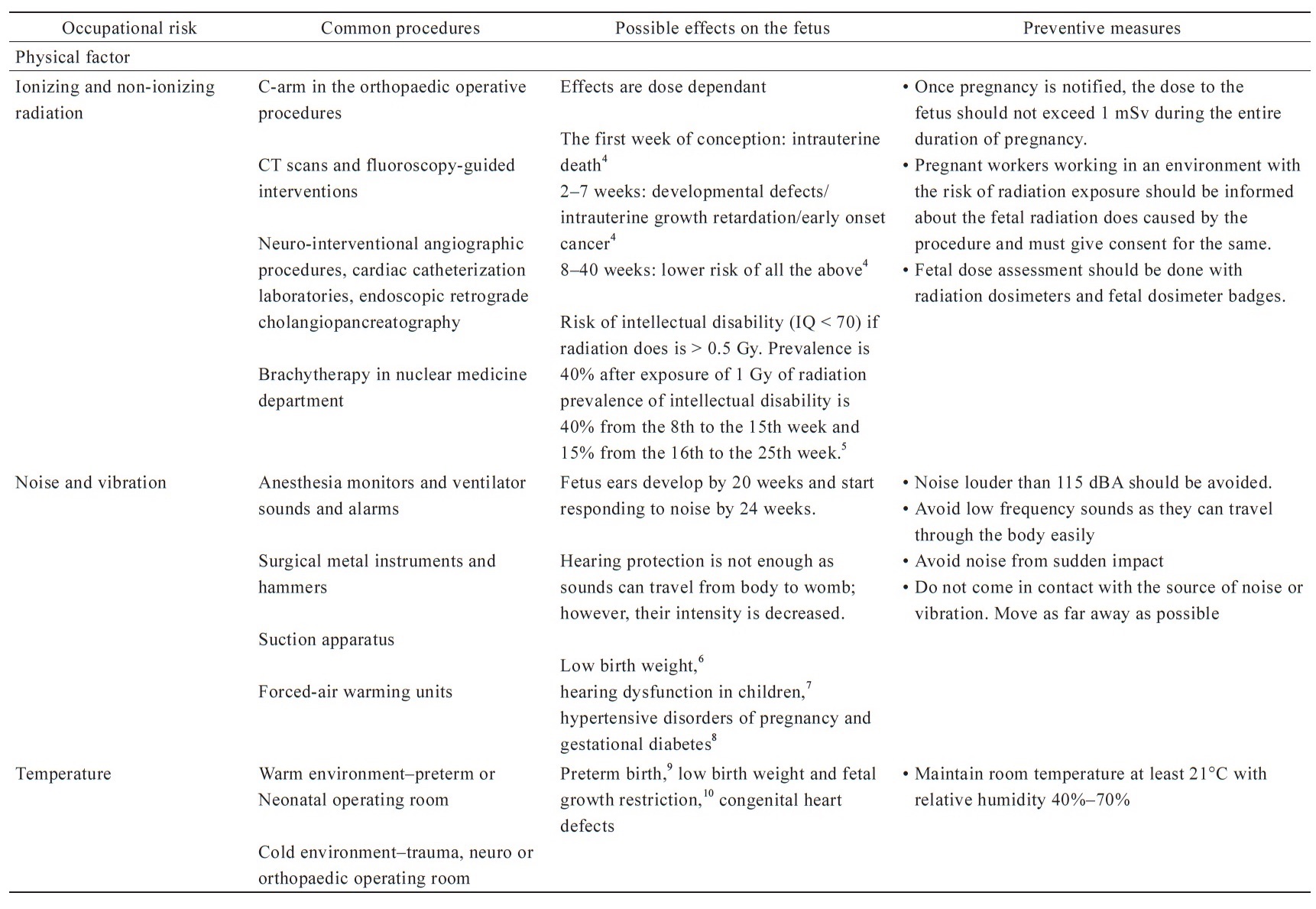
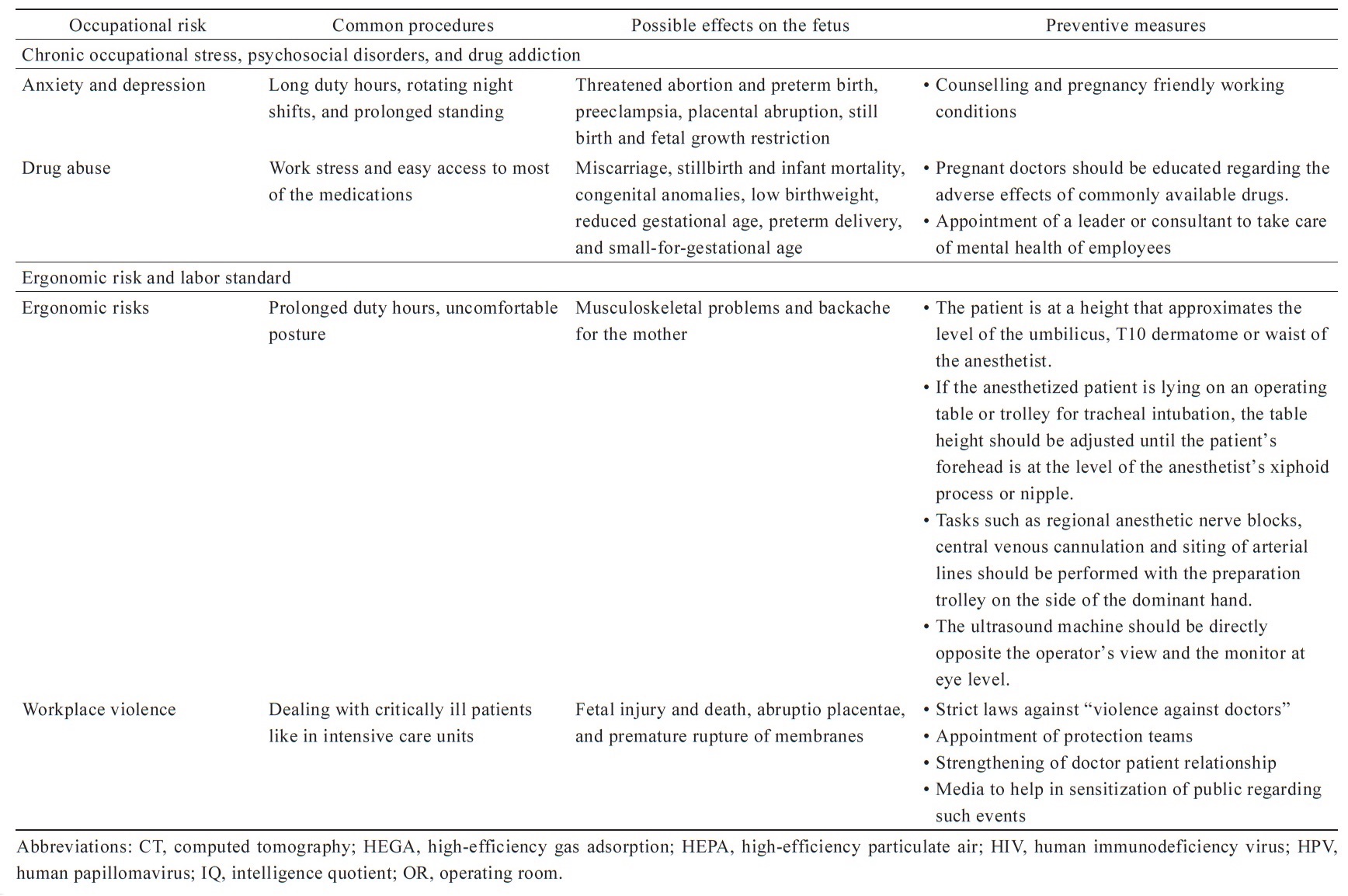
Occupational risks to anesthesia professionals have been classified into various types by different agencies.3 People in the World Federation Societies of Anesthesiologists have classified the risks into the following five principal categories, mentioned below and summarized in Table 1.4-12
Download full-size image
Download full-size image
Download full-size image
1. Physical factors and safety, such as ionizing and non-ionizing radiation, noise and vibration, heat, ventilation, lighting, electrical appliances, fires, and compressed gases
2. Chemical factors, such as latex allergy and exposure to anesthetic gases
3. Biological factors, such as viruses, bacteria, and fungi
4. Anesthesia practices, such as chronic occupational stress, psychosocial disorders, and drug addiction
5. Ergonomic risks and labor standards, including work organization, work model, workload, intense responsibility, and violence.
Physical Factors and Safety, Such as Ionizing and Non-Ionizing Radiation, Noise and Vibration, Heat, Ventilation, Lighting, Electrical Appliances, Fires, and Compressed Gases
Radiation exposure in early pregnancy is known to be associated with teratogenic effects in the fetus. Although the risk is usually overestimated, the consequences can be significant in cumulative doses. Threshold radiation effects, also called deterministic effects of radiation, occur over a dose threshold and result in cellular injury. Stochastic effects of radiation are incremental, appearing in a dose-response function without a threshold, and are thought to be the primary mechanism of increased risk of cancers in exposed individuals.13 Various agencies have given thresholds that should be referred to once the pregnancy is confirmed to minimize the effects on the fetus, mainly during the critical period of organogenesis. The International Commission on Radiological Protection recommends that after a worker declares her pregnancy, the occupational radiation dose should not exceed one mSv during the remainder of the pregnancy. The National Council on Radiation Protection and Measurements in the United States (US) recommends a radiation dose limit of 0.5 mSv per month once pregnancy is confirmed to ensure a low exposure during susceptible periods of gestation.14 The US Environmental Protection Agency recommends a limit of 5 mSv for the entire gestational period.14
An anesthesiologist is involved in numerous procedures that require ionizing radiation. Neuro-interventional angiographic procedures, cardiac catheterization laboratories, endoscopic retrograde cholangiopancreatography, and C-arm in the orthopaedic operative procedures3 are a few to mention. The radiation exposure during these procedures may be up to 6 times higher than other professionals. Computed tomography scans and fluoroscopy-guided interventions are increasingly used in diagnosis and management owing to the logical drive toward minimally invasive and safe methods.15 Although most anesthesia personnel take all due precautions because of the fear of discrimination by their peers or senior consultants, some trainees or resident doctors prefer not to disclose their pregnant status till late. If unaware of the risks during such procedures, they may expose themselves to ionizing radiation, causing inadvertent self-harm. There is a need for a cordial work environment where the resident doctors can declare their pregnant status, free from the fear of discrimination.
A pregnant anesthetist should preferably be posted in an area free from the effects of radiation. Proper protective measures should be required for pregnant anesthesia professionals handling radiation. Protective leather jackets and thyroid protective collars should be made mandatory. Radiation dosimeters and fetal dosimeter badges should be compulsory for all anesthetists and should be reviewed regularly, at least monthly.3 They should maintain a safe distance of at least 90 cm from the primary radiation source, as the amount of radiation exposure is inversely proportional to the square of the distance; therefore, doubling the distance from the radiation source can reduce the radiation exposure, not to half but one-fourth.16,17
Noise and vibrations are often ignored as occupational risks in medical care settings. In the OR, noise levels may rise to 75–90 dB, with sporadic sounds reaching 100–120 dB.18 The main contributors to these intermittent noises are the clanging or dropping metal instruments, hammers, suction apparatus, anesthesia monitors, and alarms. Forced-air warming units may add 84 dBA to the background noise. Noise causes stress, irritability, hypertension, negatively affects one’s productivity, and predisposes an individual to noise-induced hearing loss.19 Substantial hearing loss has been demonstrated among anesthesiologists,20 with a study reporting that 66% of anesthesiologists had abnormal audiograms and hearing acuity significantly worse than the general population. Occupational exposure to noise in pregnancy has also been found to be associated with low birth weight,6 hearing dysfunction in children,7 hypertensive disorders of pregnancy, and gestational diabetes.8
For pregnant anesthetists, the recommendations for safe noise exposure should be firmly adhered to. The National Institute for Occupational Safety and Health (NIOSH) recommends a time-weighted average of 85 dB for continuous exposure for an 8-hour workday and uses a 3-dBA time/intensity exchange rate in which the permissible time of exposure is halved for each 3 dBA increase in sound (the “3 dBA rule”) The limits established by the OSHA begin at 90 dBA for an 8-hour workday and use a 5-dBA exchange rate in recognition of the fact that in most workplaces interruptions in noise exposure occur throughout the day. An average noise level of 45 dBA or less within hospitals is recommended.21
The temperature in the OR needs to be modified per the patients’ requirements, thereby varying from hot to cold. The temperature may be kept in the warm range in paediatric surgery cases to prevent hypothermia in the susceptible neonate. It may be cold in cases where deliberate hypothermia is required, such as cases with traumatic brain injuries. The effects of these varying temperatures have not been studied in detail. Still, thermoregulation in a pregnant woman is disturbed because of increased weight gain and metabolic requirements of a growing foetus. A hot OR causes significantly higher core body temperature, heart rate, thermal sensation, and sweat loss,22 resulting in dehydration. This in late pregnancy could start uterine contractions resulting in premature delivery.23 Exposure to extremes of temperature, especially heat, has been well known to be associated with preterm birth,9 low birth weight, and fetal growth restriction.10 Studies have also reported an association between heat exposure and the risk of congenital heart defects.24,25 Ideally, Room temperature should be at least 21°C, and the relative humidity should be 40%–70%.26
Personnel working long hours in the OR are exposed to artificial lights. This affects their circadian rhythm and working efficiency. Continuous light exposure has been found to negatively impact uterine physiology, causing hormonal imbalance and leading to pregnancy complications.27 Fixed or rotating night shifts disturb an individual’s circadian rhythm and have been associated with adverse pregnancy outcomes.28
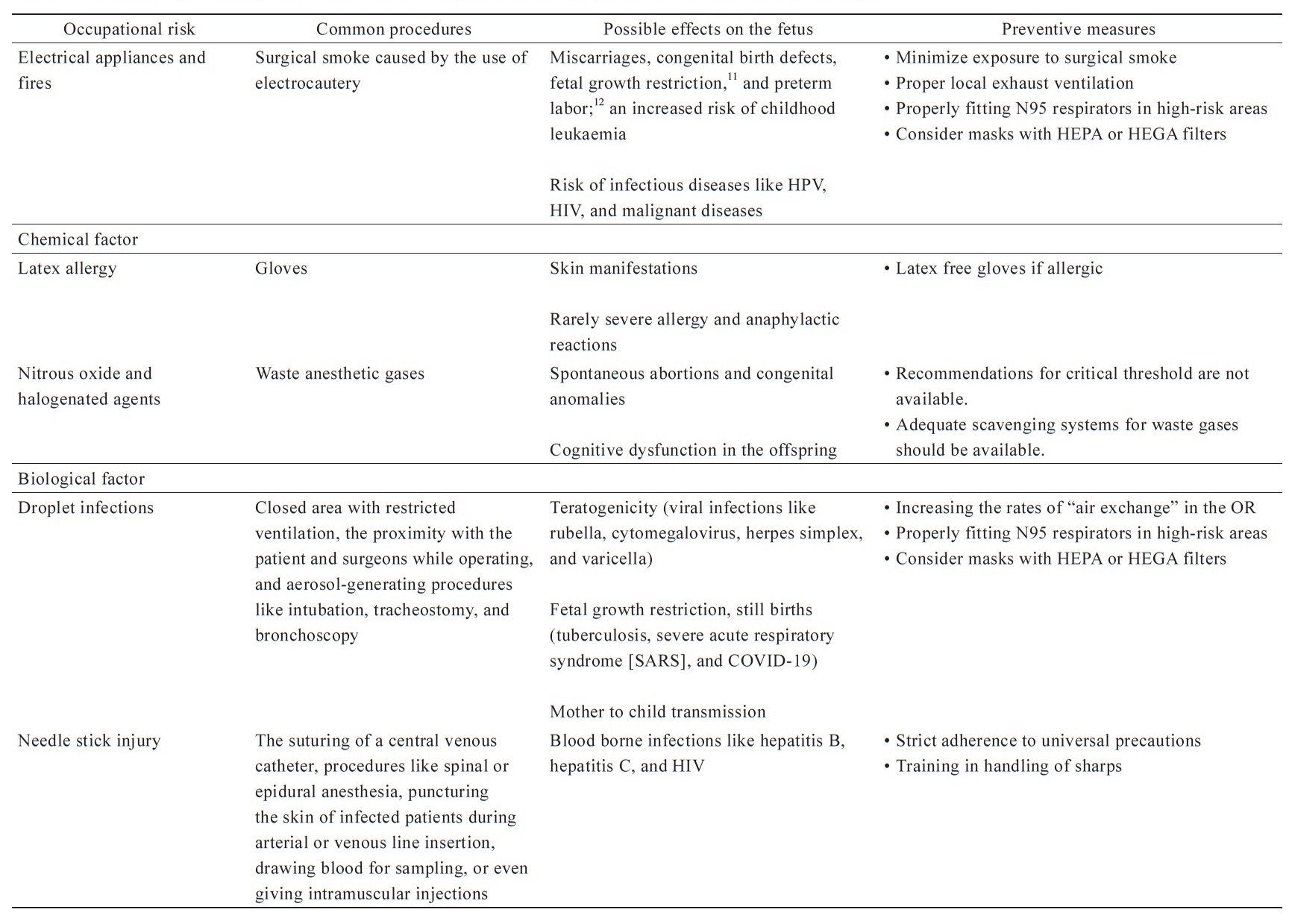
Electrical energy-based devices, such as electrocautery, are routinely used in surgical procedures in the OR. Surgical smoke refers to waste gases emitted in ORs owing to burning tissues with energy sources like electrocautery. The content of surgical smoke includes water, gases containing chemicals like benzene, 1,2-dichloroethane, and toluene, which are associated with miscarriages, congenital birth defects, fetal growth restriction,11 and preterm labor.12 Besides the harmful chemicals, surgical smoke has also been shown to harbour viable and contagious malignant cells, infectious live bacteria and viruses, including human papilloma virus (HPV) and human immunodeficiency virus (HIV).29-31 Exposure to benzene has also been associated with an increased risk of childhood leukaemia in animal and human studies.32 Many studies had found a very high concentration of fine and ultrafine particulate matter when surgical smoke was released, especially during laparoscopic procedures. Although these particles and chemicals have not been studied in detail, the effects that these particles and chemicals have on the unborn fetus could be significantly grave. The risks to pregnant anesthetists could potentially be manifold because of cumulative doses owing to prolonged exposure. The recommendations of NIOSH and OSHA regarding maintaining proper exhaust ventilation and measures to reduce exposure to surgical smoke should be strictly adhered to. A properly fitting facepiece respirator, like N95 mask instead of surgical or laser mask should be used when one works with known transmissible diseases like HPV, HIV or tuberculosis, especially in areas where local exhaust ventilation is lacking or not properly functioning.33 Masks with high-efficiency particulate air (HEPA) filters or a combination of HEPA filters with activated carbon, commonly called “high-efficiency gas adsorption” filters, can also be considered.33
Chemical Factors, Such as Latex Allergy and Exposure to Anesthetic Gases
Latex allergy is known to be quite common, and more so in health care workers as they need to wear gloves most of the time. Strangely, the risk is three times higher in pregnant females compared to their non-pregnant counterparts.34 The effects are usually mild, limited to skin manifestations in most cases, but a few cases of severe allergy and even anaphylactic reactions have been reported in pregnancy.35 Pregnant health care workers with such allergies should take special precautions and use latex-free gloves.
Nitrous oxide and halogenated agents constitute the predominant inhalational agents used for anesthesia in ORs. When inhalational agents are used for induction, predominantly for daycare procedures or minor surgeries, some waste gases are inadvertently released into the OR and inhaled by anesthetists, surgeons, and other supporting staff. These gases have been associated with adverse pregnancy outcomes like spontaneous abortions and congenital anomalies in the fetus when inhaled by pregnant women, especially during earlier gestations.36 Maternal sevoflurane exposure has also been known to be associated with cognitive dysfunction in the offspring through abnormal development of the prefrontal cortex.37 Therefore, adequate scavenging systems should be necessary for all ORs to minimize exposure.38
The NIOSH has a recommended exposure limit for nitrous oxide of 25 ppm as a time-weighted average for halogenated agents, with a ceiling concentration of 2 ppm over 1 hour. This recommendation was made in 1977 but is based predominantly on preventing decreased mental performance and dexterity rather than adverse pregnancy outcomes. These guidelines need to be updated, considering both the newly available anesthesia gases and the pregnancy considerations.39
Biological Factors, Such as Viruses, Bacteria, and Fungi
ORs have been recognized as ideal for spreading droplet-borne infections because of the closed area with restricted ventilation, the proximity with the patient and surgeons while operating, and the aerosol-generating procedures like intubation, tracheostomy, and bronchoscopy. Anesthetists work in close proximity to the patient and spread for prolonged periods near the airways of infected patients. Patients with severe diseases are more likely to require invasive ventilation and other airway procedures by the anesthetist. These are the patients with high viral load and, therefore, highly infectious. A recent study reported that 10.7% of the staff involved in tracheal intubation either tested positive for SARS-CoV-2 antigen (3.1%) or developed symptoms consistent with COVID-19 (8.4%), or were hospitalized with the disease (0.1%).40 Increasing the rates of “air exchange” in the OR should be strongly considered to mitigate the risks. Each “air exchange” removes approximately 63% of the potential virus-bearing aerosols in the environment. Thus, after five air exchanges, < 1% of the initial aerosol load is left in the room.41
Women during pregnancy are more susceptible to certain viral infections owing to impaired pathogen clearance and hormonal and immunological alterations of pregnancy. The risk for health care workers, including doctors, is increased manifold mainly owing to the prolonged contact with infected patients in closed and poorly ventilated areas such as ORs, birthing suites, high dependency units, and intensive care units. Viral infections like rubella, cytomegalovirus, herpes simplex, and varicella can be devastating, particularly during organogenesis. CDC recognizes health care workers, including doctors, nurses, dentists, paramedics, emergency medical technicians, laboratory personnel collecting and handling samples from infected persons, and morgue workers performing autopsies as the group at the highest risk of acquiring Coronavirus.42 Among the health care professionals, some professionals like anesthesiologists, otorhinolaryngologists, dentists, and ophthalmologists are at exceptionally high risk because their work demands proximity to the patient’s respiratory tract, which is the site where this virus resides and multiplies. CDC and WHO recommend using N95 masks for healthcare workers, especially when treating patients with diseases that involve droplet transmissions, such as tuberculosis, SARS, and COVID-19.43 Even after complying with proper protection and preventive measures and using personal protective equipment to protect themselves, health care workers have been affected by the disease. The disease in health care workers is usually severe owing to the high viral load.
Using personal protective equipment in pregnancy is also not an easy task. Oxygen consumption increases from the first trimester of pregnancy by around 30% per term owing to maternal metabolic processes and fetal demands.44 Increased estrogen causes hyperaemia, oedema, hypersecretion, and friability of the mucosa of the respiratory tract.45 There is an increase in the number and sensitivity of hypothalamic and medullary progesterone receptors in pregnancy, leading to a rise in the sensitivity of peripheral chemoreceptors to hypoxic conditions.46 Progesterone decreases the threshold and increases respiratory centre sensitivity to carbon dioxide. These physiological changes increase the load on the respiratory system in pregnancy. Pregnant women may be unable to maintain their required minute ventilation while breathing through N95 respirators. The workload on breathing increases significantly, leading to decreased oxygen uptake and increased carbon dioxide concentration.47 Hypoxia and hypercarbia owing to re-breathing caused by retained carbon dioxide in the mask’s dead space occur on prolonged mask usage.48 Some studies suggest that it affects fetal cerebral development , which may be caused by increasing the cerebral blood flow and intracranial pressure.48 The literature on the above subject is deficient, and more studies need to be done to assess its effects on pregnancy and prolonged usage, as it is required in most ORs or intensive care units.
All health care professionals have a very high risk of needle stick injury, and anesthesiology as a speciality is no different. Anesthetists are not as well trained in handling sutures and needle holders as the surgeons, as it is predominantly a medical branch. The suturing of a central venous catheter, procedures like spinal or epidural anesthesia, puncturing the skin of infected patients during arterial or venous line insertion, drawing blood for sampling, or even giving intramuscular injections predispose them to needle stick injuries. Resident doctors are at an exceptionally high risk as they are not trained in personal protection measures, and most of them are learning to hold and manipulate the instruments for the first time. A survey of around 700 resident doctors found that almost 99% had experienced a sharps injury.49 The probability of acquiring infection from large-bore needlestick injury may be as high as 40% in workers not vaccinated against hepatitis B virus, 1.8% for hepatitis C virus, and 0.3% for HIV.50 The effects in pregnancy are more bothersome because of the risk of the fetus being born with the disease by transplacental transmission.
Anesthesia Practices, Such as Chronic Occu-pational Stress, Psychosocial Disorders, and Drug Addiction
Pregnancy during “residency” is challenging both mentally as well as physically. The residency period, especially in clinical specialities like anesthesia and critical care, is marked by long duty hours, rotating night shifts, and prolonged standing. Long duty hours are well known to be associated with pregnancy complications, most notably threatened abortion and preterm birth.51 The risk of preeclampsia, placental abruption, still birth and fetal growth restriction is increased, too.52 Some authors have even suggested that pregnancy in doctors should be considered high risk because of the increased risk of complications.53,54 A written policy regarding the avoidance of long duty hours, prolonged standing and intermittent periods of rest during pregnancy should be made and put into practice in health care settings. A proper balance between workload and staffing, night shifts, environment of the workplace, and providing relaxation time can be helpful in this regard.
Anesthetists are often involved in the care of high-risk patients and medical emergencies. The current pandemic of coronavirus disease has made the situation even more demanding. Anxiety and depression, much higher in incidence than the general population and even fellow health care workers have been found among anesthesia professionals.55 Pregnancy and post-partum period by itself are known to be associated with psychosocial issues, and a few studies report the incidence to be as high as one in every five pregnant women.56 The risk would definitely be compounded by both the factors co-existing in the same individual, i.e., pregnancy in anesthesia personnel. Anesthesia professionals are also prone to drug abuse mainly because of the work stress and easy access to most of the medications.57 The secondary exposure to aerosolized intravenous anesthetics like propofol and fentanyl has been proposed to cause sensitization and subsequent opiate addiction among anesthesiologists.58 The effects on the fetus can be disastrous.
Ergonomic Risks and Labor Standards Include Work Organization, Work Model, Workload, Intense Responsibility, and Violence
Ergonomics, or the interplay between anesthetists and their workspace environment to promote safety, performance, and well-being, is often neglected in almost all hospital settings. Pregnant anesthetists are prone to develop musculoskeletal problems if attention to patient positioning and posture while handling the patients is not taken care of. A few recommendations to improve the ergonomics suggest that the patient is at a height that approximates the level of the umbilicus, T10 dermatome or waist of the anesthetist, if the anesthetized patient is lying on an operating table or trolley for tracheal intubation, the table height should be adjusted until the patient’s forehead is at the level of the anesthetist’s xiphoid process or nipple, and that tasks such as regional anesthetic nerve blocks, central venous cannulation and siting of arterial lines should be performed with the preparation trolley on the side of the dominant hand, the ultrasound machine directly opposite the operator’s view and the monitor at eye level.26
WHO defines workplace violence as “incidents where staff is abused, threatened or assaulted in the circumstances related to their work, including commuting to and from work, involving an explicit or implicit challenge to their safety, well-being or health.”59 Workplace violence is a significant concern in health care settings. Women, predominantly of the reproductive age group, represent nearly 80% of the health care workforce.60 The effects of direct physical violence are well known in fetal injury and death, abruptio placentae, and premature rupture of membranes. The indirect effects of verbal, physical, and even sexual abuse include psychological stress and anxiety, which is well known to cause adverse pregnancy outcomes.61 Doctors dealing with critically ill patients, such as the anesthetist and critical care specialist, are still more vulnerable because of high expectations from them.
Peer-Support
Anesthesia is one of the busiest specialities of medicine. A pregnant trainee or a physician is bound to feel discrimination from her colleagues as they may not be able to fulfil all of their duties owing to limitations imposed by pregnancy. Inadequate co-doctor support is expected because they are engrossed in their heavy duties. Several studies in the past have stressed that most residents felt inconvenienced by the presence of pregnant or lactating colleagues as they were forced to cover their responsibilities during their frequent absence.62 This workplace discrimination by colleagues and seniors sometimes forces the pregnant trainee or physician not to disclose her pregnancy till the late stages and thereby expose herself to inadvertent risks.
The Path Ahead
Pregnant health care workers need special care and consideration. A workplace environment which is more comfortable and friendly is the need of the hour. All institutions should have written policies to safeguard the health and rights of their pregnant employees. Occupational risk assessment models, which incorporate all possible risk factors,63 should be implemented. A health care worker, especially during the training and residency program, may not be well versed in assessing all the risks to her or her unborn fetus. Occupational risk management training programs should be made available and mandatory for all health care professionals. Anesthesia professionals during pregnancy should not be posted in areas exposed to ionizing radiation and harmful chemicals. They should preferably not be involved in the care of patients with infectious diseases, at least in the first trimester. Pregnant employees should have flexible working policies, including the avoidance of night shifts and long shifts, especially during the trimesters that involve the highest risk to the fetus, which should be framed.
Conclusion
Pregnant anesthesia trainees and physicians are faced with several occupational risks that can compromise their health and the health of their unborn fetuses. An occupational environment more compatible with pregnancy is the need of the hour.
Conflict of Interest
The author declares no conflict of interest.
References
| 1 |
Boer C, Moonesinghe SR.
Women empowerment in anaesthesia research and clinical practice: meeting report
from the British Journal of Anaesthesia Women in Anaesthesia Research
symposium.
Br J Anaesth. 2020;124(3):e59-e62.
|
| 2 |
Bissing MA, Lange EMS, Davila WF, et al.
Status of women in academic anesthesiology: a 10-year update.
|
| 3 |
Bajwa SJS, Kaur J.
Risk and safety concerns in anesthesiology practice: the present perspective.
Anesth Essays Res. 2012;6(1):14-20.
|
| 4 |
Taylor J, Chandramohan M, Simpson KH.
Radiation safety for anaesthetists.
Continuing Education in Anaesthesia Critical Care & Pain. 2013;13(2):59-62.
|
| 5 |
National Center for Environmental Health Agency for Toxic Substances and Disease
Registry.
Radiation and Pregnancy: Information for Clinicians.
https://www.cdc.gov/nceh/radiation/emergencies/pdf/303779-A_2019_Radiation-and-Pregnancy_508.pdf... Published April 29, 2019. Accessed July 15, 2022.
|
| 6 |
Selander J, Rylander L, Albin M, Rosenhall U, Lewné M, Gustavsson P.
Full-time exposure to occupational noise during pregnancy was associated with
reduced birth weight in a nationwide cohort study of Swedish women.
Sci Total Environ. 2019;651(Pt 1):1137-1143.
|
| 7 |
Selander J, Albin M, Rosenhall U, Rylander L, Lewné M, Gustavsson P.
Maternal occupational exposure to noise during pregnancy and hearing
dysfunction in children: a nationwide prospective cohort study in Sweden.
Environ Health Perspect. 2016;124(6):855-860.
|
| 8 |
Lissåker CT, Gustavsson P, Albin M, et al.
Occupational exposure to noise in relation to pregnancy-related hypertensive
disorders and diabetes.
Scand J Work Environ Health. 2021;47(1):33-41.
|
| 9 |
Li S, Wang J, Xu Z, et al.
Exploring associations of maternal exposure to ambient temperature with
duration of gestation and birth weight: a prospective study.
BMC Pregnancy Childbirth. 2018;18(1):513.
|
| 10 |
Basagaña X, Michael Y, Lensky IM, et al.
Low and high ambient temperatures during pregnancy and birth weight among
624,940 singleton term births in Israel (2010–2014): an investigation of
potential windows of susceptibility.
Environ Health Perspect. 2021;129(10):107001.
|
| 11 |
Sheng Z, Wang S, Zhang X, Li X, Li B, Zhang Z.
Long-term exposure to low-dose lead induced deterioration in bone
microstructure of male mice.
Biol Trace Elem Res. 2020;195(2):491-498.
|
| 12 |
U.S.
Environmental Protection Agency.
https://iris.epa.gov/static/pdfs/0118tr.pdf... Published September 2005. Accessed July 15, 2022.
|
| 13 |
Dauer LT, Miller DL, Schueler B, et al.
Occupational radiation protection of pregnant or potentially pregnant workers
in IR: a joint guideline of the Society of Interventional Radiology and the
Cardiovascular and Interventional Radiological Society of Europe.
J Vasc Interv Radiol. 2015;26(2):171-181.
|
| 14 |
Jibiri NN, Akintunde TO, Dambele MY, Olowookere CJ.
Occupational radiation exposure to the extremities of medical staff during
hysterosalpingography and radionuclide bone scan procedures in several Nigerian
hospitals.
Mol Imaging Radionucl Ther. 2016;25(3):114-120.
|
| 15 |
Fehrenbach U, Thiel R, Bady PD, et al.
CT fluoroscopy-guided pancreas transplant biopsies: a retrospective evaluation
of predictors of complications and success rates.
Transpl Int. 2021;34(5):855-864.
|
| 16 |
Park PE, Park JM, Kang JE, et al.
Radiation safety and education in the applicants of the final test for the
expert of pain medicine.
Korean J Pain. 2012;25(1):16-21.
|
| 17 |
Chang YJ, Kim AN, Oh IS, Woo NS, Kim HK, Kim JH.
The radiation exposure of radiographer related to the location in C-arm
fluoroscopy-guided pain interventions.
Korean J Pain. 2014;27(2):162-167.
|
| 18 |
Ayoğlu H, Ayoğlu FN.
Occupational risks for anaesthesiologists and precautions.
Turk J Anaesthesiol Reanim. 2021;49(2):93-99.
|
| 19 |
Seidman MD, Standring RT.
Noise and quality of life.
Int J Environ Res Public Health. 2010;7(10):3730-3738.
|
| 20 |
Wallace MS, Ashman MN, Matjasko MJ.
Hearing acuity of anesthesiologists and alarm detection.
Anesthesiology. 1994;81(1):13-28.
|
| 21 | |
| 22 |
Palejwala Z, Wallman K, Ward MK, et al.
Effects of a hot ambient operating theatre on manual dexterity, psychological
and physiological parameters in staff during a simulated burn surgery.
PLoS One. 2019;14(10):e0222923.
|
| 23 |
Konkel L.
Taking the heat: potential fetal health effects of hot temperatures.
Environ Health Perspect. 2019;127(10):102002.
|
| 24 |
Auger N, Fraser WD, Sauve R, Bilodeau-Bertrand M, Kosatsky T.
Risk of congenital heart defects after ambient heat exposure early in
pregnancy.
Environ Health Perspect. 2017;125(1):8-14.
|
| 25 |
Lin S, Lin Z, Ou Y, et al.
Maternal ambient heat exposure during early pregnancy in summer and spring and
congenital heart defects—a large US population-based, case-control study.
Environ Int. 2018;118:211-221.
|
| 26 |
Bailey CR, Radhakrishna S, Asanati K, et al.
Ergonomics in the anaesthetic workplace: guideline from the Association of
Anaesthetists.
Anaesthesia. 2021;76(12):1635-1647.
|
| 27 |
Das M, Minocha T, Kumar D, Yadav SK, Haldar C.
Continuous artificial light potentially disrupts central and peripheral
reproductive clocks leading to altered uterine physiology and reduced pregnancy
success in albino mice.
Photochem Photobiol Sci. 2022;21(7):1217-1232.
|
| 28 |
Fernandez RC, Marino JL, Varcoe TJ, et al.
Fixed or rotating night shift work undertaken by women: implications for
fertility and miscarriage.
Semin Reprod Med. 2016;34(2):74-82.
|
| 29 |
Baggish MS, Poiesz BJ, Joret D, Williamson P, Refai A.
Presence of human immunodeficiency virus DNA in laser smoke.
Lasers Surg Med. 1991;11(3):197-203.
|
| 30 |
Sood AK, Bahrani-Mostafavi Z, Stoerker J, Stone IK.
Human papillomavirus DNA in LEEP plume.
Infect Dis Obstet Gynecol. 1994;2(4):167-170.
|
| 31 |
Fletcher JN, Mew D, DesCôteaux JG.
Dissemination of melanoma cells within electrocautery plume.
Am J Surg. 1999;178(1):57-59.
|
| 32 |
Zhou Y, Zhang S, Li Z, et al.
Maternal benzene exposure during pregnancy and risk of childhood acute
lymphoblastic leukemia: a meta-analysis of epidemiologic studies.
PLoS One. 2014;9(10):e110466.
|
| 33 |
Liu Y, Song Y, Hu X, Yan L, Zhu X.
Awareness of surgical smoke hazards and enhancement of surgical smoke
prevention among the gynecologists.
J Cancer. 2019;10(12):2788-2799.
|
| 34 |
Draisci G, Zanfini BA, Nucera E, et al.
Latex sensitization: a special risk for the obstetric population?
Anesthesiology. 2011;114(3):565-569.
|
| 35 |
Shingai Y, Nakagawa K, Kato T, et al.
Severe allergy in a pregnant woman after vaginal examination with a latex
glove.
Gynecol Obstet Invest. 2002;54(3):183-184.
|
| 36 |
National Institute for Occupational Safety and Health.
Waste Anesthetic Gases—Occupational Hazards In Hospitals.
|
| 37 |
Song R, Ling X, Peng M, Xue Z, Cang J, Fang F.
Maternal sevoflurane exposure causes abnormal development of fetal prefrontal
cortex and induces cognitive dysfunction in offspring.
Stem Cells Int. 2017;2017:6158468.
|
| 38 |
Boivin JF.
Risk of spontaneous abortion in women occupationally exposed to anaesthetic
gases: a meta-analysis.
Occup Environ Med. 1997;54(8):541-548.
|
| 39 |
Occupational Safety and Health Administration.
Anesthetic Gases: Guidelines for Workplace Exposures.
https://www.osha.gov/waste-anesthetic-gases/workplace-exposures-guidelines... Revised May 18, 2000. Accessed May 12, 2022.
|
| 40 |
El-Boghdadly K, Wong DJN, Owen R, et al.
Risks to healthcare workers following tracheal intubation of patients with
COVID-19: a prospective international multicentre cohort study.
Anaesthesia. 2020;75(11):1437-1447.
|
| 41 |
Myatra SN, Gupta S, Pai PS.
Anesthesia for oral surgeries during the COVID-19 pandemic.
J Anaesthesiol Clin Pharmacol. 2020;36(Suppl 1):S96-S104.
|
| 42 |
Centers for Disease Control and Prevention (U.S.).
Investigating the impact of COVID-19 during pregnancy.
|
| 43 |
Lee DW, Li DW.
N-95 respirator: gain in protection, pain in the face?
Occup Environ Med. 2020;77(8):583.
|
| 44 |
Shah NM, Lai PF, Imami N, Johnson MR.
Progesterone-related immune modulation of pregnancy and labor.
Front Endocrinol (Lausanne). 2019;10:198.
|
| 45 |
Koehler KF, Helguero LA, Haldosén LA, Warner M, Gustafsson JA.
Reflections on the discovery and significance of estrogen receptor beta.
Endocr Rev. 2005;26(3):465-478.
|
| 46 |
Bayliss DA, Millhorn DE.
Central neural mechanisms of progesterone action: application to the
respiratory system.
J Appl Physiol (1985). 1992;73(2):393-404.
|
| 47 |
Tomimatsu T, Kakigano A, Mimura K, et al.
Maternal carbon dioxide level during labor and its possible effect on fetal
cerebral oxygenation: mini review.
J Obstet Gynaecol Res. 2013;39(1):1-6.
|
| 48 |
Toprak E, Bulut AN.
The effect of mask use on maternal oxygen saturation in term pregnancies during
the COVID-19 process.
J Perinat Med. 2020;49(2):148-152.
|
| 49 |
Makary MA, Al-Attar A, Holzmueller CG, et al.
Needlestick injuries among surgeons in training.
N Engl J Med. 2007;356(26):2693-2699.
|
| 50 |
Waljee JF, Malay S, Chung KC.
Sharps injuries: the risks and relevance to plastic surgeons.
Plast Reconstr Surg. 2013;131(4):784-791.
|
| 51 |
Takeuchi M, Rahman M, Ishiguro A, Nomura K.
Long working hours and pregnancy complications: women physicians survey in
Japan.
BMC Pregnancy Childbirth. 2014;14:245.
|
| 52 |
Gabbe SG, Morgan MA, Power ML, Schulkin J, Williams SB.
Duty hours and pregnancy outcome among residents in obstetrics and
gynecology.
Obstet Gynecol. 2003;102(5 Pt 1):948-951.
|
| 53 |
Katz VL, Miller NH, Bowes WA Jr.
Pregnancy complications of physicians.
West J Med. 1988;149(6):704-707.
|
| 54 | |
| 55 |
Li XY, Wang J, Zhang RX, et al.
Psychological status among anesthesiologists and operating room nurses during
the outbreak period of COVID-19 in Wuhan, China.
Front Psychiatry. 2020;11:574143.
|
| 56 |
Seth S, Lewis AJ, Galbally M.
Perinatal maternal depression and cortisol function in pregnancy and the
postpartum period: a systematic literature review.
BMC Pregnancy Childbirth. 2016;16(1):124.
|
| 57 |
Jungerman FS, Palhares-Alves HN, Carmona MJ, Conti NB, Malbergier A.
Anesthetic drug abuse by anesthesiologists.
Rev Bras Anestesiol. 2012;62(3):375-386.
|
| 58 |
McAuliffe PF, Gold MS, Bajpai L, et al.
Second-hand exposure to aerosolized intravenous anesthetics propofol and
fentanyl may cause sensitization and subsequent opiate addiction among
anesthesiologists and surgeons.
Med Hypotheses. 2006;66(5):874-882.
|
| 59 |
Hahn S, Hantikainen V, Needham I, Kok G, Dassen T, Halfens RJG.
Patient and visitor violence in the general hospital, occurrence, staff
interventions and consequences: a cross-sectional survey.
J Adv Nurs. 2012;68(12):2685-2699.
|
| 60 |
World Health Organization.
Joint Programme on Workplace Violence in the Health Sector Country Case
Study—Questionnaire.
https://cdn.who.int/media/docs/default-source/documents/violence-against-health-workers/wvquestionnaire.pdf?sfvrsn=9f6810a5_2&download=true... Published 2003. Accessed July 16, 2022.
|
| 61 |
Berenson AB, Wiemann CM, Wilkinson GS, Jones WA, Anderson GD.
Perinatal morbidity associated with violence experienced by pregnant women.
Am J Obstet Gynecol. 1994;170(6):1760-1769.
|
| 62 |
Rangel EL, Smink DS, Castillo-Angeles M, et al.
Pregnancy and motherhood during surgical training.
JAMA Surg. 2018;153(7):644-652.
|
| 63 |
Lellis NBM, Azevedo V, de Lucca SR, Pustiglione M, Bandini MC.
Occupational risk perceived by pregnant workers: proposal for an assessment
tool for health professionals.
Rev Bras Med Trab. 2020;18(2):169-176.
|