For people at high risk of severe respiratory failure undergoing sedation, noninvasive positive pressure ventilation may be necessary.1 The high-flow nasal cannula (HFNC) exerts multiple physiological effects, including less inspiratory effort and improved lung volume and compliance.2 Hence, we report a case of an orthopnea patient who received subcutaneous venous port implantation with HFNC under monitored anesthesia care.
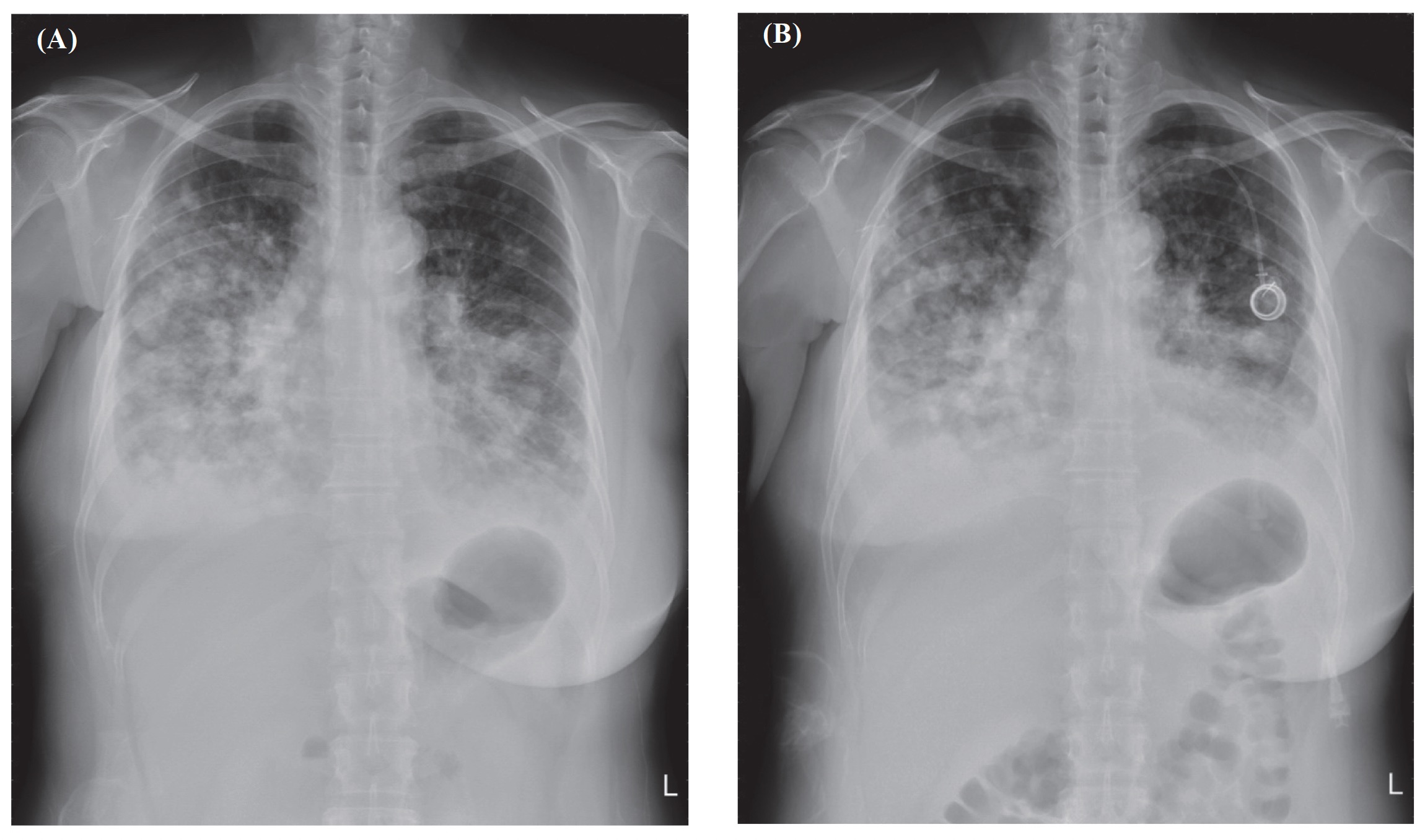
A 52-year-old woman (height, 160 cm; weight, 60 kg) had stage IV right invasive breast carcinoma with lung metastases. Chest X-ray (CXR) showed multiple metastases in both lungs and bilateral pleural effusion (Figure 1A). She presented dyspnea and orthopnea under a nasal cannula of 2–3 L/min; the pulse oximeter (SpO2) was 92% in the sitting position. However, she was unable to lie supine with local anesthesia alone for subcutaneous venous port implantation. Therefore, an HFNC (Optiflow THRIVE, Fisher and Paykel Healthcare Ltd, Auckland, New Zealand) with 30 L/min and fraction of inspiration O2 (FiO2) 60% was used to prevent hypoxia before anesthesia induction. Standard monitors and bispectral index (BIS) (BISTM, Covidien, Dublin, Ireland) were administered. Before anesthesia induction, SpO2 was elevated to 100%. Anesthesia was induced with fentanyl (25 µg), lidocaine (40 mg), target control infusion of propofol with effect-site concentration of 3 µg/mL and dexamethasone 5 mg. After induction, the patient could lie down and received local infiltration. Initially, we kept the patient at the depth of BIS 40–60, since the surgeon asked for movelessness of the patient while he was doing the puncture technique. After insertion of the guide wire, we kept the BIS values in the interval of 40–70 by adjusting the propofol concentration. The hemodynamics were stable, and the surgery was smoothly done. At the postanesthesia care unit, the HFNC was set to flow at 20 L/min, FiO2 60%, and her SpO2 was above 98%. One hour later, we replaced it with a nasal cannula at 3 L/min, and the SpO2 was above 95%. Thirty minutes later, she was transferred to the general ward with a semi-Fowler position. The patient tolerated the HFNC uneventfully, and both the patient and surgeon showed great satisfaction. The postoperative CXR showed bilateral atelectasis improved despite multiple lung metastases (Figure 1B). Alleviation of dyspnea was noted, and she finally completed two courses of chemotherapy.
Download full-size image
Atelectasis over bilateral lungs improved.
In a systematic review and meta-analysis, Rochwerg et al.1 reported that HFNC may reduce the need for tracheal intubation in patients with acute hypoxemic respiratory failure.
In general, HFNC is simple to use and highly acceptable for patients and anesthesiology practitioners; therefore, it is desirable for enhanced recovery in orthopnea patients undergoing short-duration procedures.
Future investigation of a larger sample to evaluate the effectiveness of HFNC is required.
References
| 1 |
Rochwerg B, Granton D, Wang DX, et al.
High flow nasal cannula compared with conventional oxygen therapy for acute
hypoxemic respiratory failure: a systematic review and meta-analysis.
Intensive Care Med. 2019;45(5):563-572.
|
| 2 |
Mauri T, Turrini C, Eronia N, et al.
Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory
failure.
Am J Respir Crit Care Med. 2017;195(9):1207-1215.
|