Abstract
In critically ill patients undergoing laparotomy, both general anesthesia (GA) and central neuraxial block (CNB) may pose significant risks. Peripheral truncal blocks have been reported to provide effective postoperative analgesia following laparotomy. However, there are a limited number of reports describing this technique as surgical anesthesia for laparotomy. An 86-year-old man with non-specific interstitial pneumonia under home oxygen therapy and aortic valve stenosis was diagnosed with an incarcerated inguinal hernia. Because of these comorbidities, both GA and CNB were considered relatively contraindicated. Thus, we chose an ultrasound-guided transverse abdominis plane block and ilioinguinal/iliohypogastric block supplemented with neuroleptanesthesia as surgical anesthesia for emergency laparotomy. The surgery was uneventful using this technique. Truncal blocks supplemented with titrated intravenous sedatives/analgesics could be an alternative in high-risk patients undergoing laparotomy in whom both GA and CNB are considered relatively contraindicated.
Keywords
critically ill patients, emergency laparotomy, surgical anesthesia, truncal blocks
Central neuraxial block (CNB) and general anesthesia (GA) are most commonly used in laparotomy. In patients with respiratory complications, the usefulness of CNB alone in abdominal procedures has been reported.1,2 However, both GA and CNB sometimes pose significant risks in critically ill patients. Truncal blocks have been reported to provide effective postoperative analgesia after laparotomy.3-6 Theoretically, truncal blocks as surgical anesthesia for abdominal procedures may also be warranted in critically ill patients. However, there are a limited number of reports describing this issue.
Herein, we describe the case of a patient with non-specific interstitial pneumonia under home oxygen therapy (HOT) and aortic valve stenosis (AS) who underwent emergency laparotomy for incarcerated inguinal hernia safely under ultrasound-guided truncal blocks supplemented with titrated sedatives and analgesics. Written informed consent was obtained from the patient for this case report.
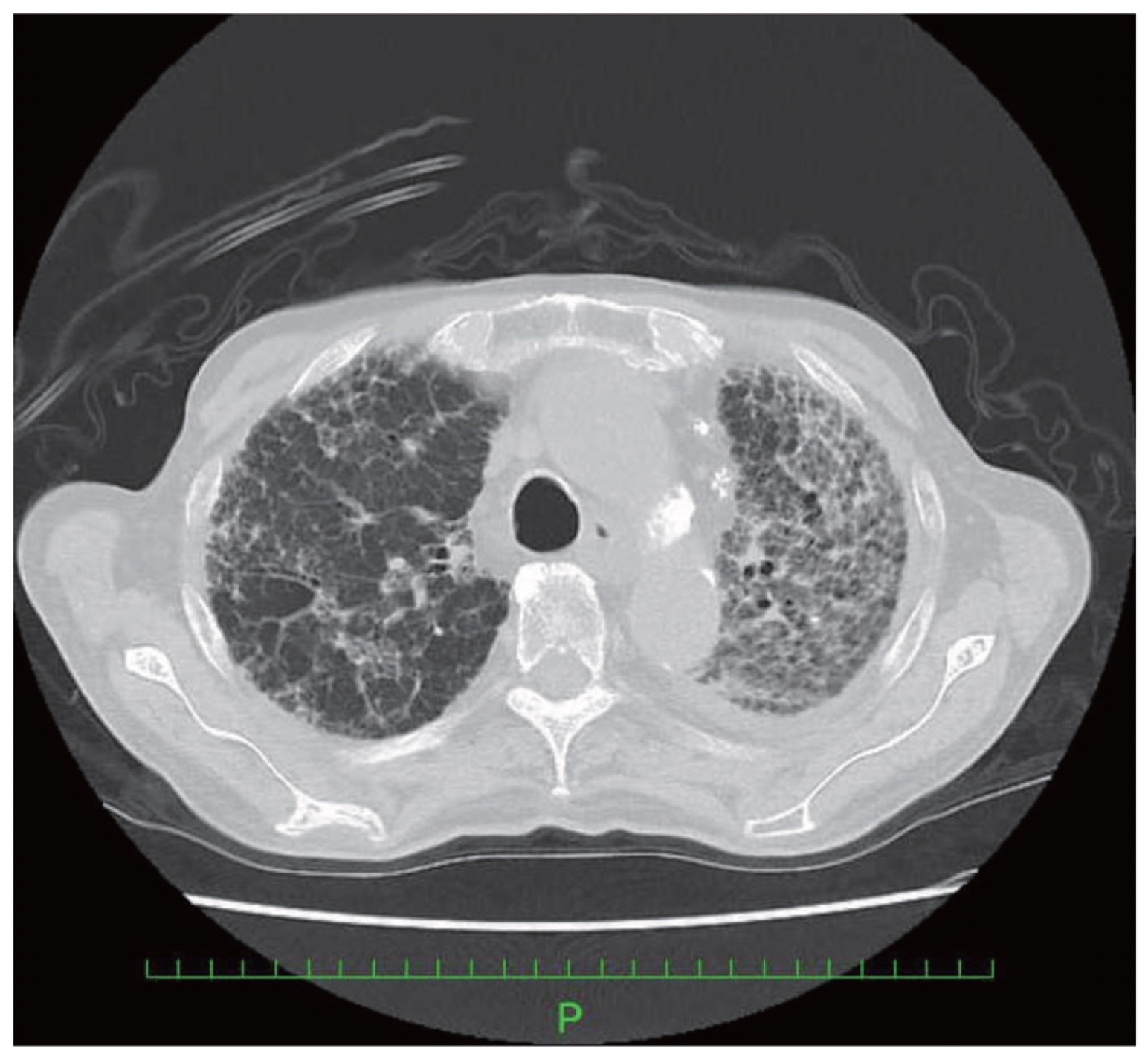
An 86-year-old man weighing 49 kg and 157 cm in height with non-specific interstitial pneumonia under HOT (2 L/min O2) presented to our emergency room with abdominal pain and swelling of the left groin region. Physical examination and enhanced computed tomography (CT) revealed a left-sided incarcerated inguinal hernia, and part of the small bowel could be ischemic. Preoperative echocardiography detected moderate AS with an aortic valve area of 0.94 cm2, aortic valve area index of 0.86 cm2/m2, and peak pressure gradient of 40 mmHg. Preoperative laboratory tests showed a white blood cell count of 13,010/µL, C-reactive protein of 4.37 mg/dL, and brain natriuretic peptide of 242.1 pg/mL. Preoperative blood gas analysis showed PaO2 of 79 mmHg, PaCO2 of 44 mmHg, and pH of 7.43 under HOT with 2 L/min O2. Preoperative chest CT scan showed typical honeycomb lungs (Figure 1). His preoperative blood pressure, heart rate, and respiratory rate were 98/60 mmHg, 108 bpm, and 22 per min, respectively. His Glasgow Coma Scale score was E3V5M6. Therefore, we suspected that he was in the septic shock according to the quick Sequential (Sepsis-related) Organ Failure Assessment.7 Considering his comorbidities and septic shock status, we judged that both GA and CNB could cause significant risks, and regional anesthesia would cause less hemodynamic and respiratory disturbance than GA and CNB. Therefore, we chose ultrasound-guided transverse abdominis plane (TAP) block and ilioinguinal/iliohypogastric (II/IH) block with intravenous droperidol and fentanyl for the emergency surgery while conserving appropriate spontaneous breathing and verbal response.
Download full-size image
Standard monitoring was applied in the operating room. Oxygen was administered at a rate of 2 L/min via a nasal cannula. Before the truncal blocks were administered, the patient was premedicated with intravenous fentanyl (50 µg) and droperidol (2.5 mg). In the operating room, regional anesthesia was administered under sterile conditions using a Sonosite S-Nerve ultrasound machine with a 6–13 MHz linear ultrasound probe (Sonosite, Bothwell, WA, USA) to provide real-time ultrasound guidance. A 100-mm B Braun Simplex peripheral block needle (B. Braun Medical, Bethlehem, PA, USA) was used. The following blocks were administered on the left side of the abdomen: (1) II/IH block with 15 mL of 0.25% ropivacaine was performed by inserting a needle 3 cm from the anterior superior iliac spine (ASIS) in-plane technique under the probe positioned between the ASIS and umbilicus, as described by Gofeld and Christakis,8 and (2) TAP block with 15 mL of 0.25% ropivacaine was performed in-plane under the probe positioned halfway along the mid-axillary line between the lower costal margin and iliac crest. After confirmation of the sensory block between T10 and L1 on the left abdominal wall using the pinprick test, surgery was commenced. During surgery, the surgeon infiltrated 0.5% lidocaine into the muscular fasciae and parietal peritoneum when accessing the abdominal cavity. In addition to local anesthetic (LA) infiltration by the surgeon, visceral pain caused by intra-abdominal manipulation was pre-emptively treated with an intermittent bolus of 50 µg fentanyl. After careful observation of the whole small bowel by the surgeons, no ischemic change was detected; thus, only inguinal hernia repair with a mesh graft was performed. Intravenous medications were titrated carefully to minimize the risks of respiratory and hemodynamic depression, and the patient maintained appropriate spontaneous breathing, verbal responsiveness, and hemodynamic stability without any vasopressor agent throughout the procedure. During the procedure, the patient did not experience pain or visceral discomfort. The surgery lasted 78 minutes and was completed uneventfully. The total amount of 0.5% lidocaine infiltrated into the surgical site and intravenous fentanyl was 9 mL and 200 µg, respectively.
In the present case, GA and CNB were avoided because of the need to avoid postoperative acute exacerbation of non-specific interstitial pneumonia and intraoperative cardiovascular collapse, potentially leading to cardiac arrest. CNB has been well-documented to significantly decrease systemic vascular resistance, resulting in hypotension due to the blockade of preganglionic sympathetic fibers.9,10 This hemodynamic mechanism can cause cardiac arrest in patients with AS. Furthermore, GA with tracheal intubation is a possible risk factor for acute exacerbation of non-specific interstitial pneumonia, irrespective of non-pulmonary or pulmonary surgery.11 Accordingly, we considered that the benefits of avoiding both GA and CNB outweighed any potential risks of regional anesthesia and thus performed truncal blocks as the main surgical anesthesia.
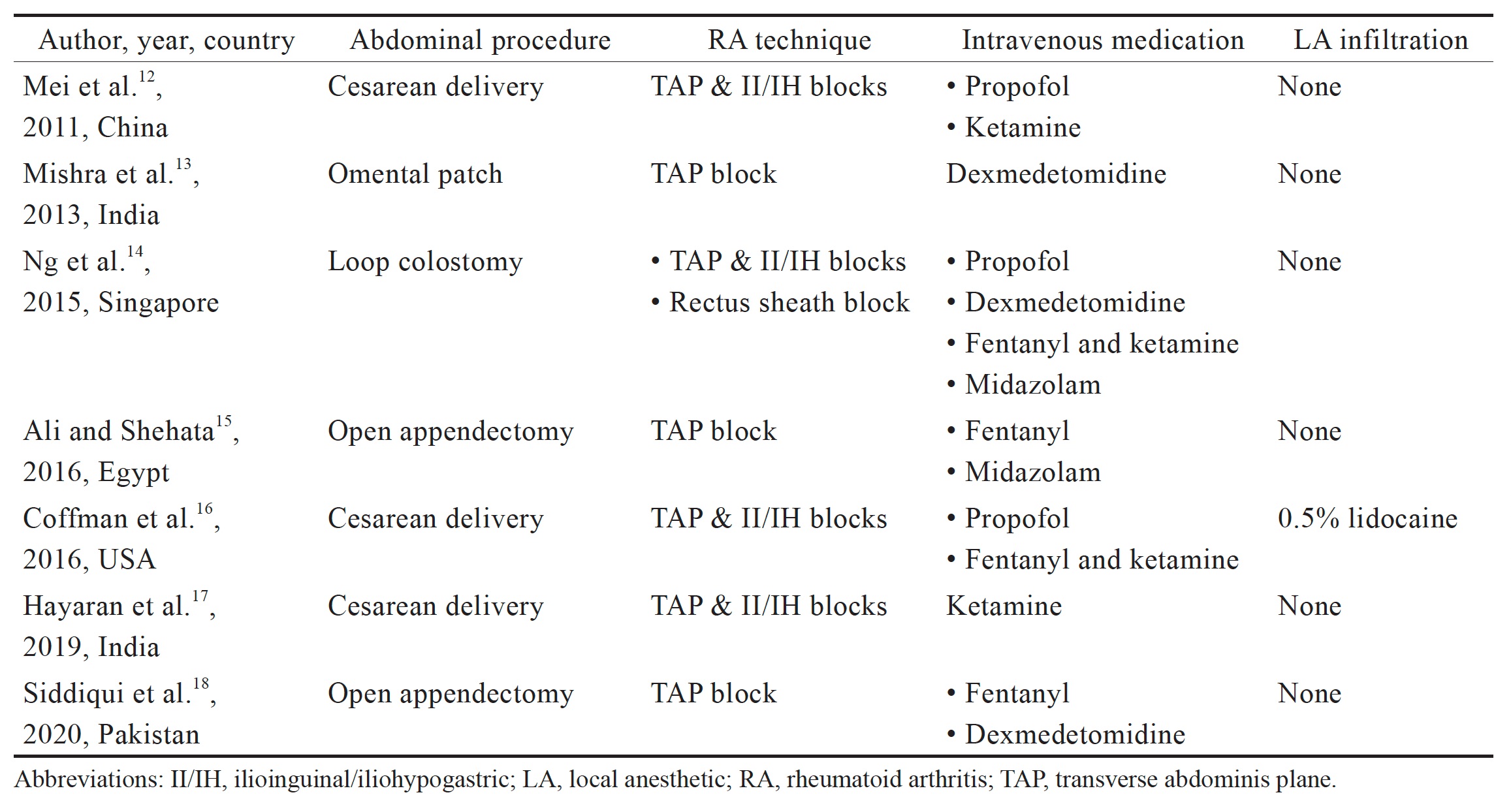
The efficacy of regional anesthesia techniques for postoperative analgesia in the trunk region has been well-documented.3-6 However, there are a limited number of reports describing these regional techniques for surgical anesthesia in laparotomy. To the best of our knowledge, seven reports have addressed this issue (Table 1).12-18 Of these, three described regional anesthesia techniques for cesarean delivery and four for laparotomy because of acute abdomen. In these reports, all surgeries were performed with truncal blocks with intravenous sedatives/analgesics under spontaneous breathing.12-18 The skin, muscles, and parietal peritoneum of the anterior abdominal wall are innervated by the lower six thoracic nerves and the first lumbar nerve. The TAP block supplemented with the II/IH block covers the cutaneous sensation of the lower anterior abdominal wall (T10–L1).14,17 However, unlike CNB, truncal blocks do not cover visceral pain caused by intra-abdominal manipulation. Complete denervation of visceral pain requires celiac plexus block to block vagal afferents.19 In this regard, these reports discussed intravenous sedatives/analgesics and LA infiltration at the surgical site to relieve visceral pain and retching sensation during bowel handling. For the same reason, gentle surgical manipulation is also mandatory under this regional technique. Various opioids and sedatives were used in each case, including fentanyl, ketamine, propofol, midazolam, and dexmedetomidine. Intravenous anesthetics acting at different sites generally exhibit synergy. Additionally, life-threatening respiratory depression due to central apnea may occur in susceptible patients after balanced anesthesia with opioids and dexmedetomidine.20 These issues should be addressed. Accordingly, the choice of opioids and sedatives should depend on the patient’s comorbidities and general condition. Most importantly, such intravenous agents should be strictly titrated to maintain appropriate respiratory and hemodynamic stability, while sufficiently inhibiting visceral stimulation. Additionally, to ensure the safety margin in inhibiting visceral pain, LA infiltration at the surgical site should be considered. Coffman et al.16 reported that LA infiltration into the visceral peritoneum of the uterus helped minimize visceral discomfort during intra-abdominal manipulation.
Download full-size image
Regarding the systemic toxic effects of LA, attention should be paid to the total amount of LA used for regional anesthesia. In the present case, the total dose of 75 mg ropivacaine (1.5 mg/kg) was far less than the recommended maximum dose of 3 mg/kg.21 The total amount of lidocaine used for the LA infiltration was minimal.
In conclusion, the efficacy of truncal blocks for surgical anesthesia remains controversial. However, truncal blocks supplemented with strictly titrated intravenous sedatives/analgesics and LA infiltration at the surgical site could be an alternative in high-risk patients undergoing laparotomy in whom both GA and CNB are considered relatively contraindicated.
Author Contributions
Yukihide Koyama helped conceive the structure of the case report and write the manuscript. Kei Morita helped conceive the structure of the case report. Yoriko Murase helped conceive the structure of the case report. Haruko Nishikawa collected the data and supervised the draft writing. Koichi Tsuzaki helped conceive the structure of the case report and revised the whole body of manuscript.
Conflicts of Interest
There are no conflicts of interest.
References
| 1 |
Savas JF, Litwack R, Davis K, Miller TA.
Regional anesthesia as an alternative to general anesthesia for abdominal
surgery in patients with severe pulmonary impairment.
Am J Surg. 2004;188(5):603-605.
|
| 2 |
England RJ, Blues C, Amin SN.
Reversal of loop ileostomy under spinal anaesthesia.
Int J Colorectal Dis. 2005;20(4):349-352.
|
| 3 |
Mishriky BM, George RB, Habib AS.
Transversus abdominis plane block for analgesia after Cesarean delivery: a
systematic review and meta-analysis.
Can J Anaesth. 2012;59(8):766-778.
|
| 4 |
Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG.
The transversus abdominis plane block provides effective postoperative
analgesia in patients undergoing total abdominal hysterectomy.
Anesth Analg. 2008;107(6):2056-2060.
|
| 5 |
O’Donnell BD, McDonnell JG, McShane AJ.
The transversus abdominis plane (TAP) block in open retropubic prostatectomy.
Reg Anesth Pain Med. 2006;31(1):91.
|
| 6 |
Bell EA, Jones BP, Olufolabi AJ, et al; Duke Women’s Anesthesia Research Group.
Iliohypogastric-ilioinguinal peripheral nerve block for post-Cesarean delivery
analgesia decreases morphine use but not opioid-related side effects.
Can J Anaesth. 2002;49(7):694-700.
|
| 7 |
Singer M, Deutschman CS, Seymour CW, et al.
The third international consensus definitions for sepsis and septic shock
(Sepsis-3).
JAMA. 2016;315(8):801-810.
|
| 8 |
Gofeld M, Christakis M.
Sonographically guided ilioinguinal nerve block.
J Ultrasound Med. 2006;25(12):1571-1575.
|
| 9 |
Critchley LA.
Hypotension, subarachnoid block and the elderly patient.
Anaesthesia. 1996;51(12):1139-1143.
|
| 10 |
Hanss R, Bein B, Weseloh H, et al.
Heart rate variability predicts severe hypotension after spinal anesthesia.
Anesthesiology. 2006;104(3):537-545.
|
| 11 |
Furuya K, Sakamoto S, Takai Y, Sato N, Matsumoto K, Homma S.
Acute exacerbation of idiopathic interstitial pneumonia after nonpulmonary
surgery under general anesthesia: a retrospective study.
Sarcoidosis Vasc Diffuse Lung Dis. 2017;34(2):156-164.
|
| 12 |
Mei W, Jin C, Feng L, et al.
Bilateral ultrasound-guided transversus abdominis plane block combined with
ilioinguinal-iliohypogastric nerve block for cesarean delivery anesthesia.
Anesth Analg. 2011;113(1):134-137.
|
| 13 |
Mishra L, Pani N, Mishra D, Patel N.
Bilateral transversus abdominis plane block as a sole anesthetic technique in
emergency surgery for perforative peritonitis in a high risk patient.
J Anaesthesiol Clin Pharmacol. 2013;29(4):540-542.
|
| 14 |
Ng O, Thong SY, Chia CS, Teo MCC.
Revision of loop colostomy under regional anaesthesia and sedation.
Singapore Med J. 2015;56(5):e89-e91.
|
| 15 |
Ali HM, Shehata AH.
Open appendectomy using ultrasound guided transversus abdominis plane block: a
case report.
Anesth Pain Med. 2016;7(2):e38118.
|
| 16 |
Coffman JC, Fiorini K, Ristev G, Beeston W, Small RH.
Transversus abdominis plane and ilioinguinal/iliohypogastric blocks for
cesarean delivery in a patient with type II spinal muscular atrophy.
Int J Obstet Anesth. 2016;25:79-81.
|
| 17 |
Hayaran N, Malhotra R, Tyagi S, Jain A.
Transversus abdominis plane block with ilioinguinal-iliohypogastric nerve a
viable alternative to provide surgical anesthesia for cesarean delivery: a case
report.
A A Pract. 2019;12(6):185-186.
|
| 18 |
Siddiqui KM, Ali MA, Salim B.
Transversus abdominis plane block as a sole anesthetic technique for open
appendectomy in patient with Treacher Collins syndrome: a case report.
J Surg Case Rep. 2020;2020(12):rjaa431.
|
| 19 | |
| 20 |
Ho AMH, Chen S, Karmakar MK.
Central apnoea after balanced general anaesthesia that included
dexmedetomidine.
Br J Anaesth. 2005;95(6):773-775.
|
| 21 |
Williams DJ, Walker JD.
A nomogram for calculating the maximum dose of local anaesthetic.
Anaesthesia. 2014;69(8):847-853.
|