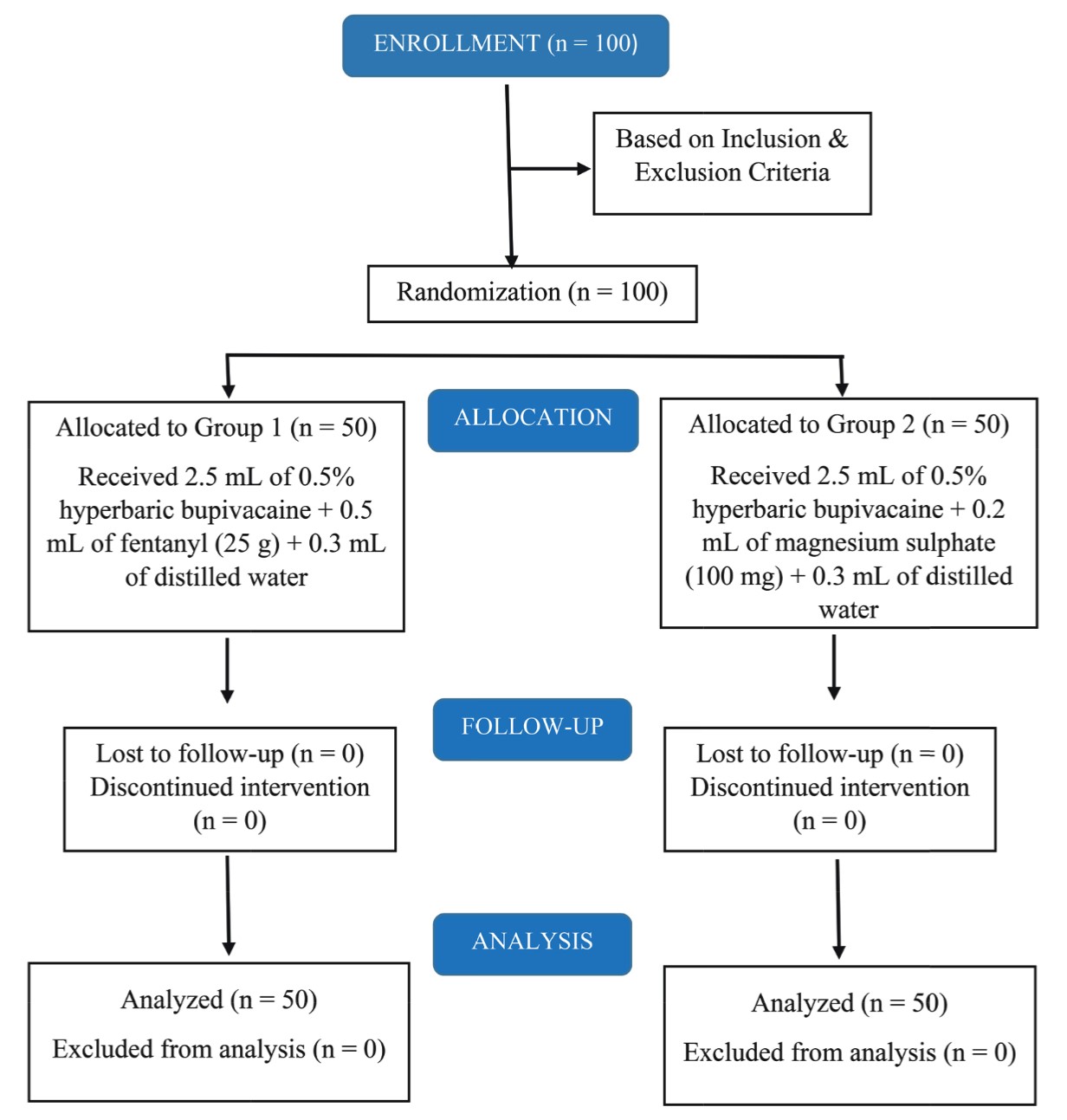
Abstract
Background
In pediatric patients due to shorter trachea suboptimal positioning of endotracheal tube (ETT) is seen in 20%–50% of patients triggering grave complications. We compared standard auscultation and ultrasound-guided lung sliding to confirm the position of ETT in children.
Methods
Seventy-five pediatric patients between 2–8 years of age, American Society of Anesthesiologists physical status classification I and II scheduled for surgery under general anesthesia with endotracheal intubation were studied. The position of ETT was confirmed by chest auscultation for the breath sounds bilaterally and by ultrasound on the same sites for lung-sliding signs. The data obtained were compared to findings on waveform capnography. Study outcomes included position of the ETT; tracheal or esophageal, accuracy of diagnosis and time taken till confirming the diagnosis.
Results
Compared to waveform capnography findings, an ultrasound revealed a sensitivity of 94.31%, a specificity of 72.33%, and an accuracy of 90.7% while that for standard auscultation were 82.8%, 47.28%, and 74.67%, respectively. The mean time taken for confirmation of ETT position was significantly shorter with waveform capnography (10.29 ± 2.25 s) compared to auscultation (12.96 ± 2.23 s) and ultrasonography (USG) (14.28 ± 3.77 s).
Conclusion
Confirmation of ETT position using USG or waveform capnography is essential because of high false results using standard auscultation alone. Ultrasound-guided lung sliding method is a simple, fast, and a reliable method used for detecting tube malposition.
Keywords
endotracheal tube, lung sliding, standard auscultation, ultrasonography, waveform capnography
Introduction
Securing the airway in children by tracheal intubation requires skill and expertise. Endotracheal intubation is used as an emergency lifesaving procedure by anesthesiologists, emergency medicine physicians, and critical care physicians. Direct visualization of the glottis and passing the tracheal tube under direct vision is considered the gold standard but not a guarantee of correct placement, especially in the infant and young child. Pediatric patients carry a high propensity for adverse airway events because of their anatomic characteristics which include a prominent occiput, a large tongue relative to the oral cavity size, an anteriorly positioned larynx, a floppy epiglottis, and a shorter trachea than adults. Misplacement and malposition of the endotracheal tube (ETT) are associated with many serious complications like esophageal insertion, unplanned extubations, and improper mainstem bronchial intubations leading to atelectasis or air leak syndromes. Owing to the various complications, confirmation of the accurate ETT placement should be done rapidly using a reliable method.1-4
In clinical practice, the optimal position of the ETT is confirmed by lung auscultation, chest wall movement, capnography. Auscultation of 5 points on the chest and abdomen, 2 sites on each side of the chest, and 1 in the epigastric region area has been a traditional method of ETT positioning and confirmation. Current international guidelines recommend the use of capnography as the gold standard along with clinical signs for detecting the placement of ETTs. However, this is not a failsafe technique as severe airway obstruction may prevent sufficient carbon dioxide exhalation from being detected by capnometers. Small concentrations of carbon dioxide may be detected after an esophageal intubation, especially if bag and mask ventilation has insufflated previously exhaled air into the stomach. Moreover, capnography does not allow differentiation between tracheal and endobronchial intubation, and withdrawing the ETT blindly may have significant consequences.2,5-6
Point-of-care ultrasound (POCUS) has increasingly been used as a potential confirmatory tool for ETT confirmation. The 2015 Advanced Cardiac Life Support guidelines state that POCUS may be a useful adjunct for ETT confirmation. Previous studies have demonstrated the use of ultrasound for diaphragm ultrasound, ultrasound-guided pulmonary tree examination, and the ultrasound-guided lung sliding sign to confirm the optimal location of the tracheal tube. Among these, the ultrasound-guided lung sliding sign has been reported as easy with a high sensitivity and specificity. With its non-invasiveness, portability, potential to provide real-time assessments, and lack of radiation exposure, ultrasonography (USG) is an appealing tool for endotracheal intubation and ETT positioning.7-9
We hypothesized that ultrasound-guided lung sliding sign in children is advantageous to confirm the optimal location of the tracheal tube compared with auscultation only. We conducted this prospective study to compare the ETT placement using ultrasonographic determination of lung sliding sign and standard auscultation method in terms of accuracy and rapidity.
Methods
This prospective and comparative study was conducted in the Department of Anesthesiology and Critical Care, PGIMS, Rohtak from March 2019 to March 2020 after approval from the institutional ethical committee (No. IEC/Th/ 18/Anst32 dated Feb, 2019) was obtained.
Pediatric patients between the age group of 2–8 years belonging to American Society of Anesthesiologists physical status of 1 or 2 of either sex scheduled for elective surgery under general anesthesia and requiring endotracheal intubation with cuffed tubes were included in the study. Exclusion criteria were patients with an anticipated difficult airway, any lung pathology, upper respiratory tract infection symptoms, emergency surgery, unstable hemodynamic status, allergy to USG gel, and refusal to participate in the study.
After taking detailed clinical history, all the patients were subjected to a complete physical as well as systemic examination during the pre-operative visit a day prior to surgery for determination of demographic data, clinical assessment for assurance of inclusion and exclusion criteria. Routine investigations like hemoglobin, bleeding time, clotting time, or any other required investigation were carried out in all the patients. The purpose and protocol of the study were explained to all the parents/guardians of the patients and informed written consent to participate in the study was obtained from parents/guardians.
All the patients enrolled in the study were kept fasting for 6 hours for solids and 2 hours for clear liquids prior to the scheduled time of surgery. Patients were premedicated with 0.5 mg/kg oral midazolam before separation from their parents. Upon arrival in the operating room, routine monitors like heart rate (HR), electrocardiography (ECG), EtCO2, and oxygen saturation (SpO2) were attached to Drager Primus monitor and an intravenous (IV) line was secured with an appropriately sized cannula. Ultrasound was performed with Sonosite M-Turbo ultrasound machine with a 6–13 MHz linear probe, two-dimensional M-mode modalities.
In all patients, a uniform anesthetic protocol was followed. All patients were pre oxygenated for 3 minutes and induction was done with injection (Inj). fentanyl 2 µg/kg followed by Inj. thiopentone sodium 5 mg/kg or graded concentration of sevoflurane in 50% oxygen and 50% nitrous oxide. Neuromuscular blocking agent IV vecuronium 0.08 mg/kg was given to facilitate intubation. Direct laryngoscopy and intubation were done with a cuffed ETT of appropriate size determined by the Khine’s formula [ID (mm) = 0.25 × (age in years) + 3].10 Patients were manually ventilated with the reservoir bag of the breathing circuit, and the appearance of EtCO2 waveform was looked for and was used to confirm the tracheal placement of the ETT.
After induction of anesthesia and intubation, one anesthesiologist was made responsible for auscultatory confirmation of the ETT placement by the presence of breath sounds sought on both sides in the infra-clavicular and infra-axillary areas and was classified into definite, doubtful, or absent.
Time taken for auscultatory confirmation was defined as time elapsed from the beginning to the end of auscultation and was noted by another anesthesiologist who was not involved in this study, and the same anesthesiologist was also made responsible for monitoring and recording the intraoperative parameters HR, SpO2, and EtCO2.
A third anesthesiologist was responsible for performing USG to ascertain the position of ETT by identifying the lung sliding sign within the same areas as auscultation using Sonosite M-Turbo ultrasound machine with a 6–13 mm linear probe kept ready by the side of the patient. The ultrasound probe was placed in the mid-clavicular line in the sagittal plane with the arrow mark just below the clavicle so that the upper part of the probe was over the second intercostal space. First, the ribs and then the pleural line were identified. Air entry to the lung field as indicated by lung sliding was sought (Figure 1) (Normally, the pleura moves for the ribs). The presence or absence of these signs was noticed and documented on both sides. Assessment by USG also consisted of demonstrating the lung sliding sign at the pleural interface—a “to and fro” movement of the pleura synchronized with ventilation, and the findings were measured as present or absent.
Download full-size image
Again, the time required to demonstrate the lung sliding by the USG was noted by the same anesthesiologist responsible for keeping the records. Time taken by USG was defined as the time taken from the placement of the USG probe till the position of the ETT was given by the anesthesiologist.
The obtained results were compared with the positive result of quantitative waveform capnography (WC). A positive result on WC was set as the detection of appropriate exhaled CO2 that was > 30 mmHg after at least 5 breaths with a typical CO2 waveform. Time used by WC to assure tracheal intubation was also determined. WC was considered the gold standard for confirmation of ETT position.
The primary study outcome included the detection of the position of ETT; tracheal, esophageal, or bronchial. The secondary outcome was firstly to determine the accuracy of diagnosis using either standard auscultatory method or ultrasound lung sliding sign in comparison to WC and secondly the time taken to confirm the diagnosis by either technique.
Sample Size and Statistical Analysis
Sample size was determined based on the ability to detect the accuracy of ETT placement by comparing the two techniques. After the inclusion of 75 patients, there was 80% power at an alpha 0.05 two-sided to detect a 10% difference between the two techniques in determining the accuracy of ETT placement. We chose a 90% baseline ratio of ETT placement in standard auscultation technique based on a previous similar study.11
Statistical analysis was performed, and the data were coded and entered into Microsoft Excel spreadsheet. Analysis was done using SPSS version 20.0 (IBM Corp., Armonk, NY, USA) Windows software program. Descriptive statistics included computation of percentages, mean ± standard deviation. The unpaired
Results
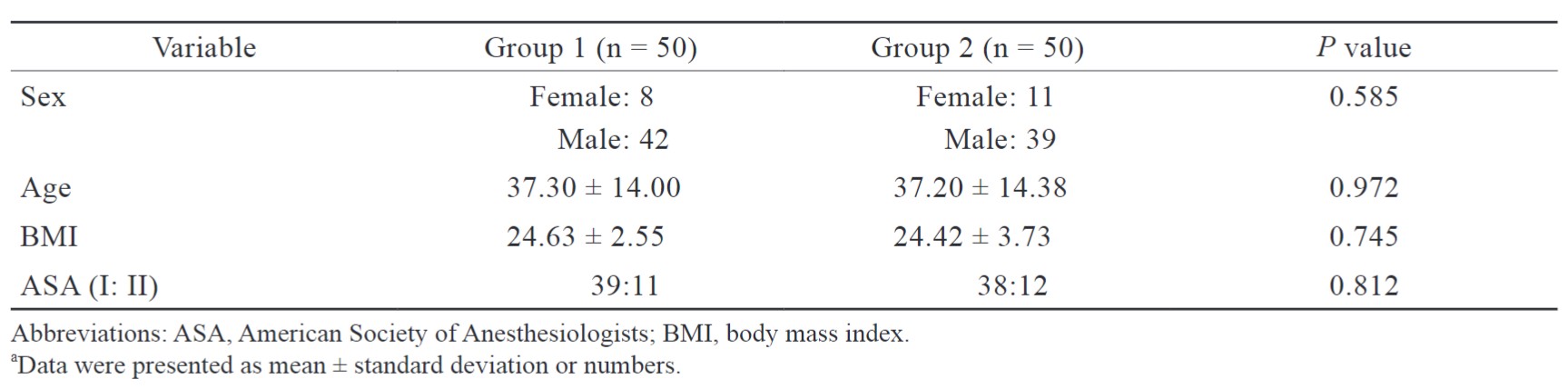
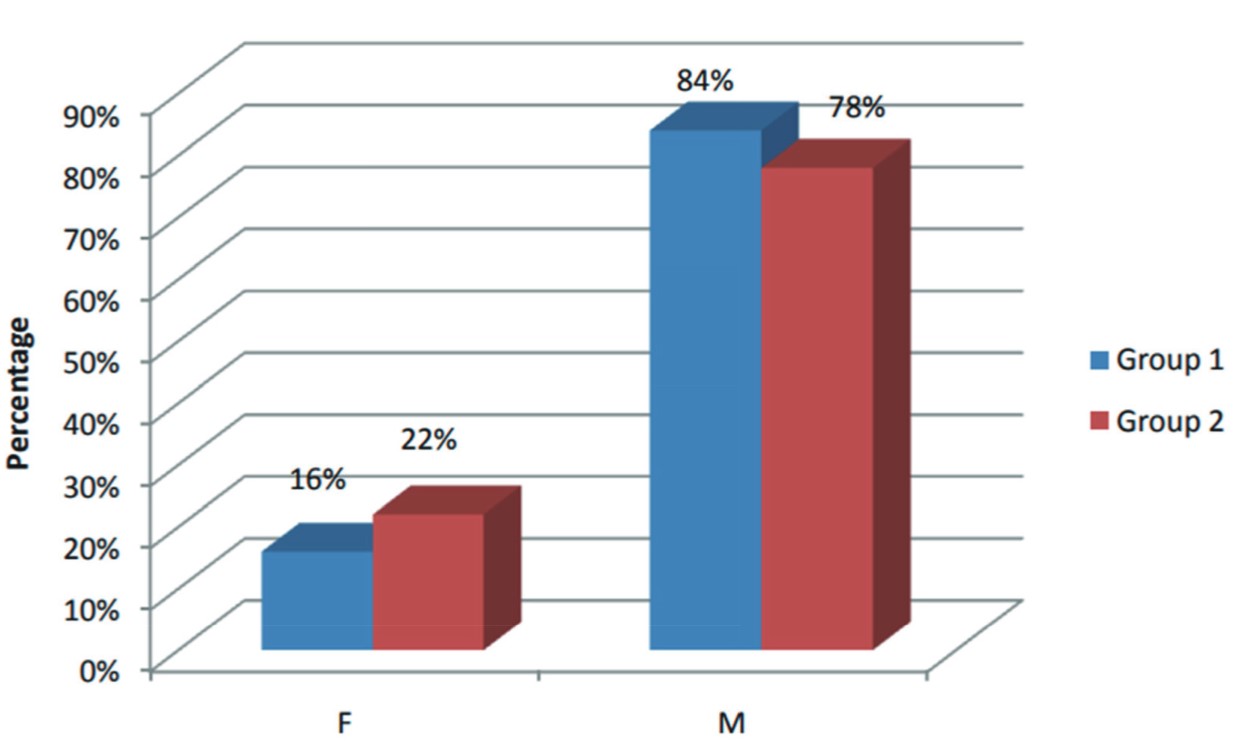
The study included 81 patients; 6 patients were excluded and 75 patients were enrolled in the study out of which 44 were males and 31 females. The demographic profile of the study population is shown in Table 1.
Download full-size image
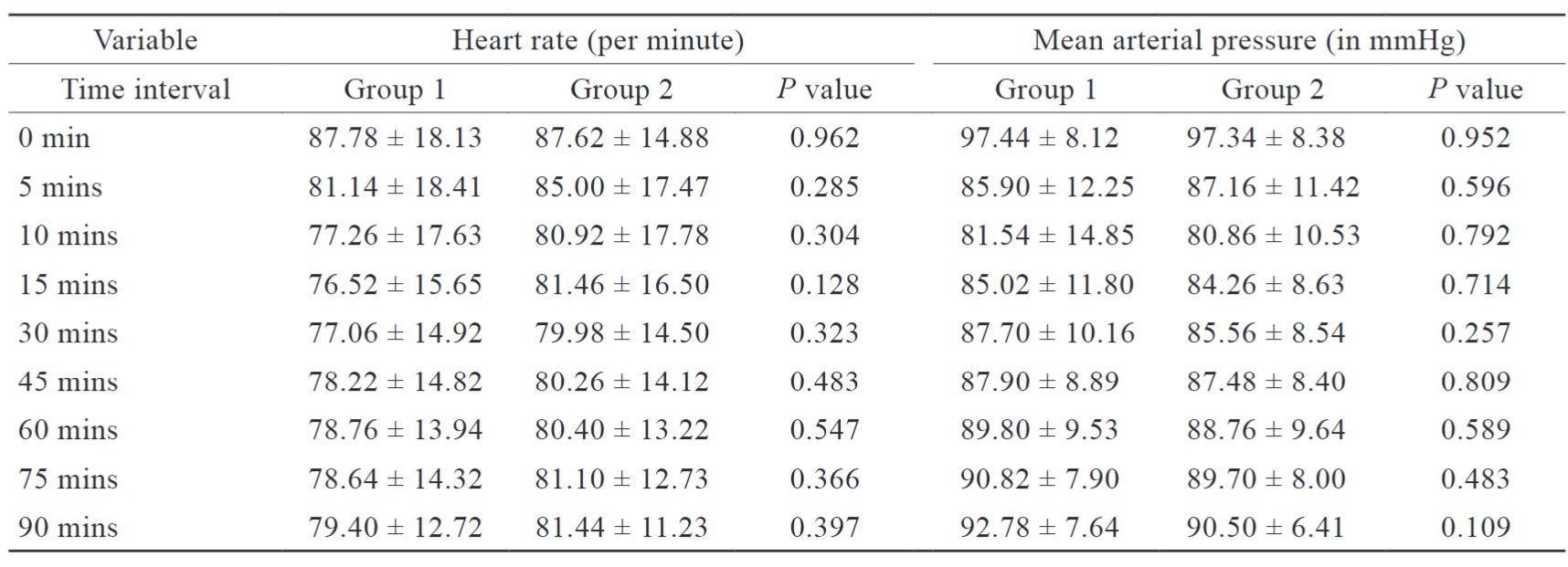
When we observed immediately after intubation, after 5 minutes of intubation, and after 15 minutes of intubation, HR and SpO2 showed a significant increase from baseline immediately after intubation. These levels returned to normal within 15 minutes of intubation.
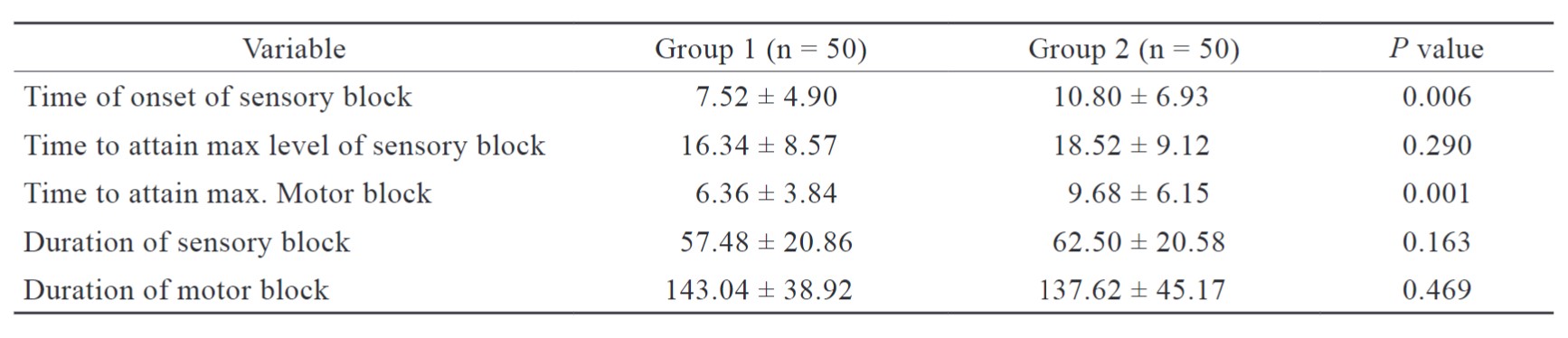
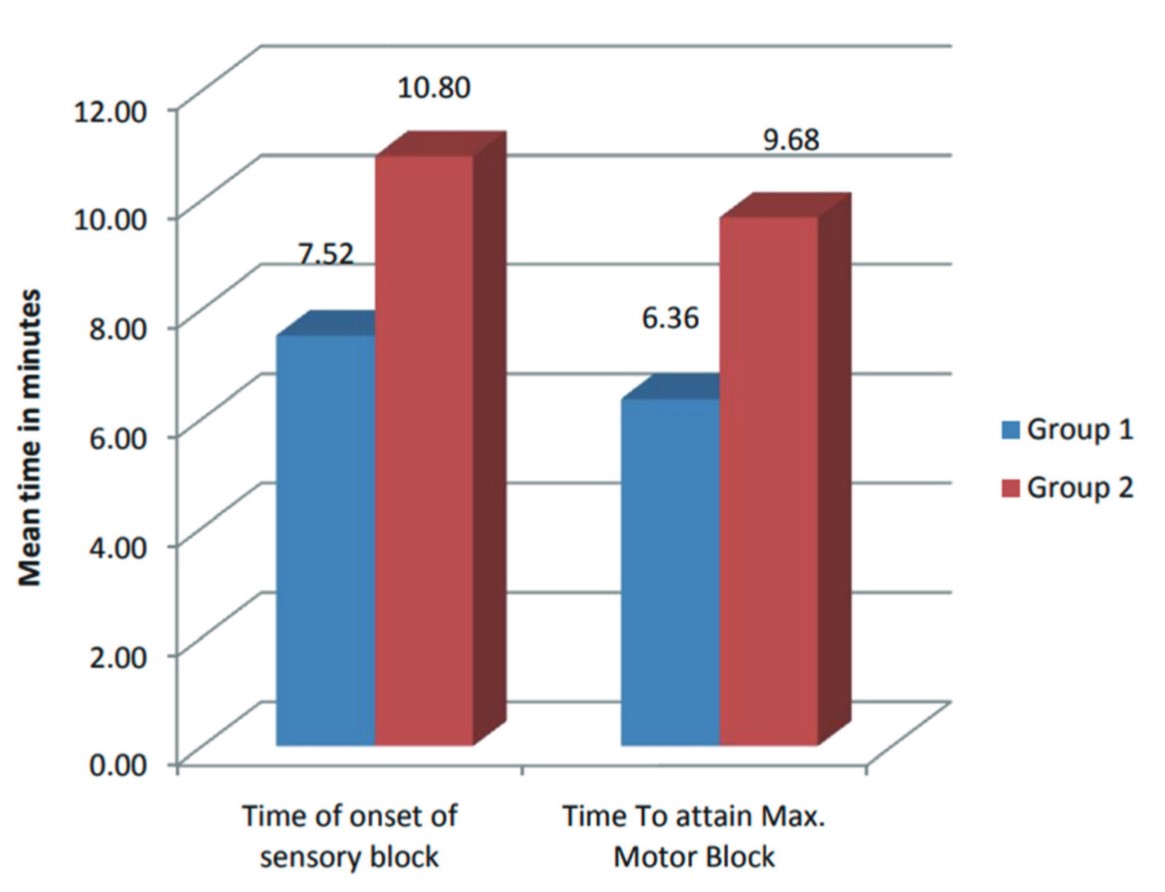
The mean time taken to confirm the ETT placement by auscultation was 12.96 ± 2.23 s while it was found to be 14.28 ± 3.77 s with USG. No significant difference was seen between the two methods (
Download full-size image
Confirmation of ETT position by auscultation showed proper tracheal location in 67 patients with definitely sought equal breath sounds bilaterally. It suspected aberrant location of the ETT in 8 patients as doubtfully sought breath sounds in 3 patients and absent breath sounds in 5 patients.
On the other hand, USG detected the proper tracheal position of the ETT in 59 patients and in 11 patients the ETT location was confirmed in the bronchus. In 5 patients esophageal insertion of ETT was observed evidenced by the absence of lung sliding sign.
When observed by WC which was taken as the gold standard for comparison, tracheal position was observed in 70 patients and esophageal in 5 patients (Table 3).
Download full-size image
Evaluating the diagnostic validity of auscultatory confirmation of ETT position versus WC findings showed a sensitivity and specificity of 82.8% and 47.28%, respectively, with an accuracy rate of 74.67% which was significantly lower as compared to USG which had an accuracy rate of 90.67% (Figures 2 and 3).
Download full-size image
Download full-size image
Discussion
All of 75 patients who were included in the study underwent both auscultation and point of care USG after direct laryngoscopy and orotracheal intubation. Out of 75 patients, 5 patients had accidental esophageal intubation which was subsequently corrected and placed into a trachea. Since the majority of the patients were free from any comorbidities and did not have difficult intubation, the chances of misplacement of the tube were relatively low. However, due to numerous anatomical variations in pediatric patient’s airway, it is challenging to place the tracheal tube correctly.12
The present study observed that the location of the ETT can be detected using the standard 5-point auscultation technique.13 Auscultatory confirmation of ETT position in all the 75 patients assured proper tracheal intubation in 89.33% of patients and suspected aberrant ETT position in approximately 4.00% of patients which was sought as endobronchial in location. The absence of bilateral breath sounds in 6.67% of patients was interpreted as esophageal intubation. Ultrasonographic determination of lung sliding sign detected tracheal position of ETT in 78.67% of patients, endobronchial position in 14.67% of patients, and esophageal intubation in 6.67% of patients.
The sensitivity of the auscultatory technique was 82.8% with a specificity of 47.28%. The diagnostic accuracy of this technique was 74.67%. Using USG for the confirmation of proper ETT position versus WC findings showed sensitivity and specificity of 94.3% and 72.3%, respectively. The diagnostic accuracy of this technique was 90.7%. WC on the other hand failed to detect endobronchial tube location in 11 patients which was detected by USG.
The reported superiority of USG over auscultatory confirmation of ETT was in agreement with the study of Ramsingh et al.14 who reported a higher sensitivity, specificity, and accuracy of 93%, 96%, and 95% versus 66%, 59%, and 62% for differentiating tracheal and bronchial intubations. They reported that pleural lung sliding examination showed an improved ability to detect both right and left bronchial intubation over auscultation. Zadel et al.15 also drew similar inferences from their study wherein a sensitivity and specificity of 100% and 90% respectively for auscultation and a specificity and specificity of 100% both for POCUS alone and for a combination of auscultation and POCUS was observed. Since auscultation is highly dependent upon the clinical experience of the anesthesiologists, there are high chances of missing endobronchial intubation, and therefore it may be attributed to more clinical experience of the physician. Also, due to interobserver variability, there are high chances of undiagnosed endobronchial intubations which may lead to serious complications. In line with the reported figures, Adi et al.16 concluded bedside upper airway USG is in concordance with Lin et al.17 reported similar results.
The average time taken for determining the ETT placement using standard auscultation was 12.96 ± 2.23 s whereas for USG was 14.28 ± 3.77 s. No clinical as well as statistical difference was seen in either modality. The accuracy of USG in detecting the correct location of ETT was found to be 90.76% which was far more superior to standard auscultation with the accuracy of 74.67%. These findings also followed a study by Rajan et al.18 who concluded that ultrasound directed confirmation of ETT placement in overweight and obese patients is superior in speed and accuracy in comparison to the standard auscultatory method.
The findings of the two modalities were compared with the study of Arafa et al.11 who conducted a study to estimate the accuracy and rapidity of bedside upper airway USG versus standard auscultation for confirmation of ETT position in 107 adult patients. In comparison to WC, findings in upper airway USG revealed significantly higher sensitivity, specificity, and accuracy rates as compared with standard auscultation. Also, the time required for confirmation of ETT position was significantly faster in upper airway USG when compared with standard auscultation.
A very recent study conducted by Ahn et al.3 in pediatric patients aged 0–24 months also concluded that lung sliding was more accurate than auscultation for optimal positioning of the ETT.
This prospective study shows that the ultrasonographic lung sliding sign is a highly accurate method for determining the location of ETT after an endotracheal intubation by interpretation of lung sliding sign. It appears to be easily interpretable and can be performed with a high degree of sensitivity and specificity when compared to the standard method of auscultation.
Other common modalities available for the detection of correct ETT placement within trachea have various limitations. The use of standard sizing for the tube based on height and weight is prone to error, and chest X-ray poses an exposure hazard especially in pediatric age group. Despite the technology being widely available, the use of USG for the airway is not widespread. This can be attributed to the challenge faced during the training of perioperative physicians. This study highlights the utility of airway ultrasound as an emerging diagnostic tool. With various evidence available in studies conducted in adult age groups suggesting the use of USG to accurately and quickly determine the ETT location, its use in pediatric airway management can result in better and favorable outcomes and fewer complications.
Conclusion
Although USG is a valuable tool for confirmation of ETT placement, it is dependent on the provider’s ability to detect and interpret images. Consequently, it is imperative that anesthesiologists receive adequate training before this technique is practiced routinely.
Based on the existing evidence, USG appears to be highly sensitive and specific for guiding and verifying ETT placement. It is easily available, rapid, and noninvasive and does not depend on ventilation for confirmation. Therefore, with proper training, inclusion of USG can be made as an essential theatre equipment.
References
| 1 |
Salem MR, Baraka A.
Confirmation of tracheal intubation.
|
| 2 |
Itoh T, Gorga S, Hashikawa A, et al.
Point-of-Care ultrasound for pediatric endotracheal tube placement confirmation by advanced practice transport nurses.
Air Med J. 2020;39(6):448-453.
|
| 3 |
Ahn JH, Kwon E, Lee SY, Hahm TS, Jeong JS.
Ultrasound-guided lung sliding sign to confirm optimal depth of tracheal tube insertion in young children.
Br J Anaesth. 2019;123(3):309-315.
|
| 4 |
Sugiyama K, Yokoyama K, Satoh KI, Nishihara M, Yoshitomi T.
Does the murphy eye reduce the reliability of chest auscultation in detecting endobronchial intubation?
Anesth Analg. 1999;88(6):1380-1383.
|
| 5 |
Verghese ST, Hannallah RS, Slack MC, Cross RR, Patel KM.
Auscultation of bilateral breath sounds does not rule out endobronchial intubation in children.
Anesth Analg. 2004;99(1):56-58.
|
| 6 |
Schmölzer GM, O’Reilly M, Davis PG, Cheung PY, Roehr CC.
Confirmation of correct tracheal tube placement in newborn infants.
Resuscitation. 2013;84(6):731-737.
|
| 7 |
Long B, Koyfman A, Gottlieb M.
Diagnostic accuracy of ultrasound for confirmation of endotracheal tube placement.
Acad Emerg Med. 2019;26(9):1096-1098.
|
| 8 | |
| 9 |
International Liaison Committee on Resuscitation.
2005 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations.
Resuscitation. 2005;67(2-3):187-201.
|
| 10 |
Motoyama EK, Davis PJ.
Smith’s Anesthesia for Infants and Children.
|
| 11 |
Arafa S, Abouzkry A, Mohamady A.
Accuracy of bedside upper airway ultrasonography vs.
J Anesth Clin Res. 2018;9(2):1000804.
|
| 12 |
Knapp S, Kofler J, Stoiser B, et al.
The assessment of four different methods to verify tracheal tube placement in the critical care setting.
Anesth Analg. 1999;88(4):766-770.
|
| 13 |
Howells TH, Riethmuller RJ.
Signs of endotracheal intubation.
Anaesthesia. 1980;35(10):984-986.
|
| 14 |
Ramsingh D, Frank E, Haughton R, et al.
Auscultation versus point-of-care ultrasound to determine endotracheal versus bronchial intubation: a diagnostic accuracy study.
Anesthesiology. 2016;124(5):1012-1020.
|
| 15 |
Zadel S, Strnad M, Prosen G, Mekiš D.
Point of care ultrasound for orotracheal tube placement assessment in out-of hospital setting.
|
| 16 |
Adi O, Chuan TW, Rishya M.
A feasibility study on bedside upper airway ultrasonography compared to waveform capnography for verifying endotracheal tube location after intubation.
Crit Ultrasound J. 2013;5(1):7.
|
| 17 |
Lin MJ, Gurley K, Hoffmann B.
Bedside ultrasound for tracheal tube verification in pediatric emergency department and ICU patients: a systematic review.
Pediatr Crit Care Med. 2016;17(10):e469-e476.
|
| 18 |
Rajan S, Surendran J, Paul J, Kumar L.
Rapidity and efficacy of ultrasonographic sliding lung sign and auscultation in confirming endotracheal intubation in overweight and obese patients.
Indian J Anaesth. 2017;61(3):230-234.
|