Abstract
Introduction
Deep neuromuscular blockade (d-NMB) is an essential requirement for carboperitoneum during laparoscopy surgery. However, sustaining d-NMB till the completion of surgery delays the reversal of the residual block. Therefore, there is a merit in exploring the effect of synergistic vecuronium-atracurium combination on the duration-of-action of d-NMB during “laparoscopic” surgery when we compare intubating bolus non-depolarizers (atracurium, vecuronium) administered alone. This study aims to evaluate whether the synergistic effect atracurium-vecuronium combination increases duration-of-action of d-NMB “laparoscopic” surgery settings.
Methods
Forty-eight patients (18–60 years, American Society of Anesthesiologists physical status-II/III, either sex) undergoing laparoscopic cholecystectomy were randomly allocated to receive vecuronium (vecuronium group, n = 16) or atracurium (atracurium group, n = 16) or vecuronium-atracurium combination (vecuronium-atracurium combination group, n = 16) and analyzed for the effects on the duration-of-action (
Results
Duration-of-action of neuromuscular blockade was significantly longer in patients who received atracurium-vecuronium combination (53.9 ± 9.7 minutes) versus atracurium-alone (41.1 ± 3.8 minutes) or vecuronium-alone (43.5 ± 9.2 minutes) (
Conclusion
The synergistic effect of the atracurium-vecuronium combination leads to an increased duration-of-action of d-NMB during laparoscopic cholecystectomy without impacting onset-of-action, quality of intubating conditions, and reversal of muscle relaxant effect.
Keywords
atracurium, neuromuscular blockade, vecuronium
Introduction
Laparoscopic surgery requires adequate depth of general anesthesia (GA) and deep neuromuscular blockade (d-NMB-train-of-four [TOF]-0) to establish carbo-peritoneum and facilitate conduct of surgery good surgical working conditions, i.e., ease-of-access and adequate intraabdominal working space with safe/lower insufflation pressures.1-3 The only problematic caveat to the above is while d-NMB is necessary till the very end of the surgery, the wound closure takes no time and that there can be a delay in reversing the residual NMB. Duration-of-action and reversibility are two aspects of a d-NMB blockade that can be worked upon to respond to the above-stated issue. Since reversibility of NMB cannot be often facilitated, we aimed to evaluate whether synergism offered by combining atracurium and vecuronium increases the duration-of-action of the intubating bolus dose during short-to-moderate duration laparoscopic surgery.
Atracurium and vecuronium are well-profiled for the muscle relaxant effect in patient undergoing “open” surgery under GA. Further, though there is evidence that combined atracurium-vecuronium administration has a synergistic effect on the onset/duration of muscle relaxation during “open” surgery;4-7 the same is not adequately studied in “laparoscopic surgery” settings.
The present study worked on hypothesis that synergistic effect of combining vecuronium and atracurium would increase the duration of d-NMB during laparoscopic cholecystectomy following administration of the intubating bolus. This randomized study analyzed the effect of vecuronium-atracurium combination versus atracurium-alone or vecuronium-alone on duration-of-action (
Methods
After Institutional Ethics Committee approval (approval no. EC/10/17/1280, name of Ethics Committee: Institutional Ethics Committee; date of approval: 28/10/2017) and written informed consent, 48 participants aged 18–60 years, American Society of Anesthesiologists (ASA) physical status II/III, of either sex, who underwent elective laparoscopic cholecystectomy were included in this single center prospective, double-blinded, three-arm, and randomized controlled study.
Patients with uncompensated cardiovascular disease, pulmonary dysfunction (obstructive/restrictive lung disease), hepato-renal or endocrinology disorders; allergy/hypersensitivity to study drugs; and those with a history of substance abuse and psychiatric illness; were excluded from the study. The study was registered at clinicaltrials.gov protocol and results registration system (ID: NCT03371953; date of registration: 13/12/2017). All authors comply with the Declaration of Helsinki and relevant national laws and regulations.
The patients were randomly divided into one of the following three groups:
Group 1 (vecuronium group): The patients received an intubating bolus dose of vecuronium bromide (0.08 mg/kg) followed by a maintenance top-up dose (0.02 mg/kg, if required).
Group 2 (atracurium group): The patients received an intubating bolus dose of atracurium (0.6 mg/kg) followed by a maintenance top-up dose (0.15 mg/kg, if required).
Group 3 (atracurium + vecuronium group): The patients belonging to this group were administered a combination of vecuronium (0.04 mg/kg) + atracurium (0.3 mg/kg) as half of the respective intubating bolus dose followed by one-fourth of the combination intubating dose bolus as top-up, if required.
The enrolled patients were randomly allocated to one of the three groups in a 1:1:1 ratio using a computer-generated random number system (https://stattrek.com/statistics/random-number-generator.aspx), which generated a random allocation sequence. The randomization sequence was controlled by a single dedicated investigator who randomly assigned the random allocation to one of the three groups in the preoperative area. Randomization concealment was undertaken with a sealed opaque envelope technique wherein the generated sequence was listed on a piece of white paper, which was then placed in the envelope before supplying to the operation room (OR) area. In the OR, the envelope was opened and given to the independent anesthesiologist who then prepared the drug as per the allocation plan. After the allocated drug was administered, the sticker containing the patient’s details was pasted on the empty envelope and sent back to the randomization controller.
The patient, attending anesthesiologist, and the dedicated personnel recording the assessment parameters were blinded to the randomization sequence and to the drug supplied as a 5-mL clear solution in a 5-mL syringe. The study drug for the three-group allocation was contained in a similar 5-mL solution having the drug in 0.9% saline diluent.
A dedicated peripheral intravenous cannula was secured and standard ASA monitoring (SpO2, EKG, NIBP, and EtCO2) was applied before induction of anesthesia. In addition, neuromuscular monitor (TOF watch SX. Organon, Teknica BV, Boxtel, the Netherlands) was applied to monitor the muscle relaxation effect on adductor-pollicis muscle. Anesthesia was induced with fentanyl (2 µg/kg) and propofol (2.0–2.5 mg/kg). After induction, the TOF Watch SX was calibrated, and the muscle relaxant was administered as per the respective group allocation. The trachea was intubated once the TOF count was 0. Thereafter, GA was maintained with sevoflurane and nitrous oxide in oxygen.
During maintenance phase of GA, the top-up bolus dose of muscle relaxant was given in a one-fourth proportion of the intubating bolus in response to TOF count of 1. Anesthesia was discontinued at the point of completion of skin closure. The residual muscle relaxation was reversed with neostigmine (50 µg/kg) and glycopyrrolate (10 µg/kg) when the TOF count was > 3. The trachea was extubated once the TOF ratio was > 0.9, and the patients were wide awake and obeying commands. Hemodynamic parameters, like, heart rate, non-invasive blood pressure (systolic, diastolic, and mean) along with oxygen saturation were noted at 5-minute intervals for the first 15 minutes after induction of GA followed by 15-minute interval until 120 minutes or the end of the surgery, whichever was earlier.
The following parameters were assessed for profiling the muscle relaxation effect of the three study groups:
(1) Onset-of-action: The onset-of-action of the muscle relaxant was calculated (in seconds) from the time of administration of the drug to the point when the TOF count became “0”.
(2) Duration-of-action: Duration-of-action of the muscle relaxation effect was calculated (in minutes) from the point the TOF count of “0” to the point when TOF count was “1”.
(3) Reversibility of muscle relaxant effect: Reversal of the residual neuromuscular blockade (neostigmine 50 µg/kg + glycopyrrolate 10 µg/kg) was undertaken when the TOF count more than or equal to “3” was used as a reversal agent in all the participants. Reversibility or time for a complete reversal of the drug was calculated (in seconds) from the time of administration of the reversal agent to the point when the TOF ratio was 90%.
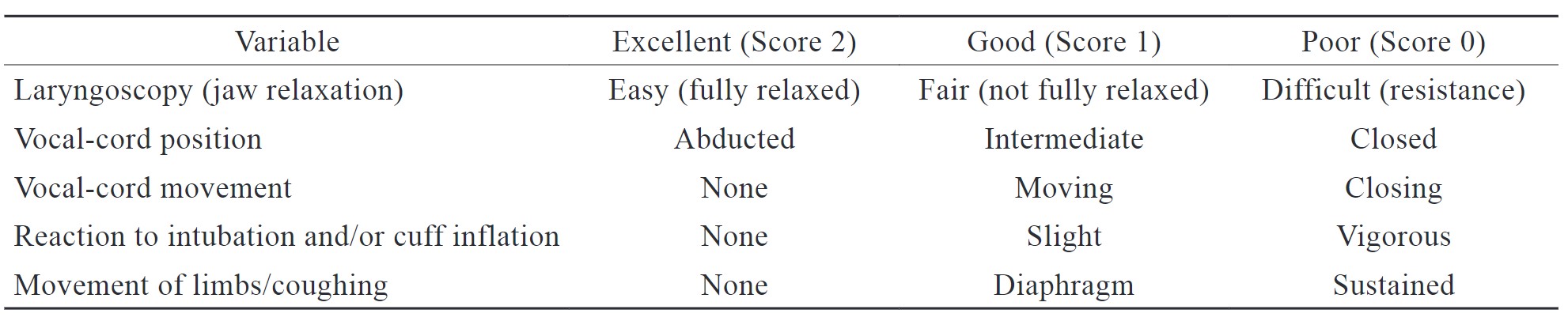
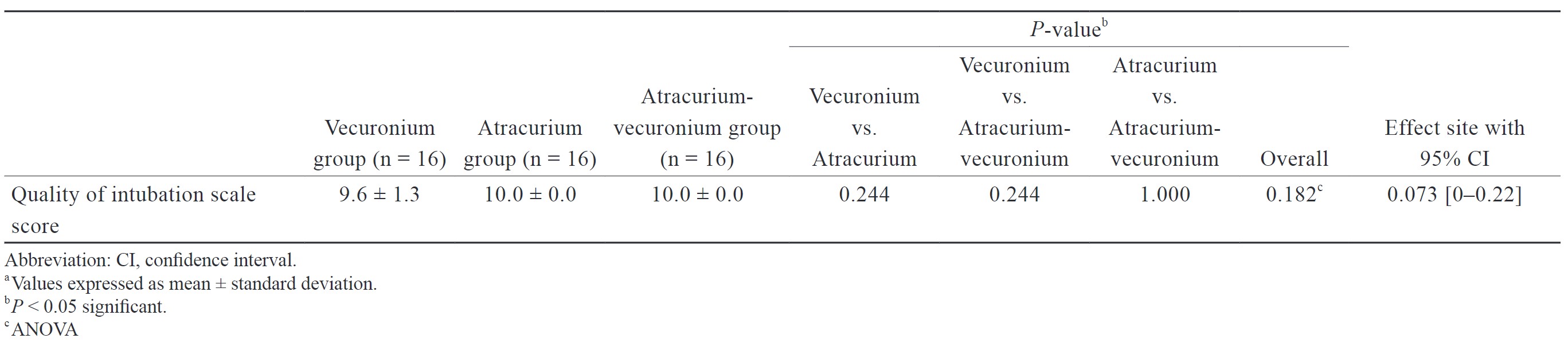
(4) The quality of intubating condition was assessed according to the consensus conference on good clinical research practice in pharmacodynamic studies of neuromuscular blocking agents using a 5-variable quality of intubation scale accounting to a maximum score of 10 and minimum score of “0” (Table 1). 8
Download full-size image
Statistical Analysis
Statistical analysis was performed by the SPSS program for Windows, version 28.0 (SPSS, Chicago, Illinois) and included the comparison of baseline, primary, and secondary outcome variables between the three groups, namely, vecuronium group, atracurium group, and atracurium-plus-vecuronium group. Continuous variables are presented as mean ± standard deviation (SD) and categorical variables as absolute numbers and percentages. Data was checked for normality before statistical analysis. The comparison of normally distributed continuous variables which included demographic parameters (age, weight, height, duration of surgery, and duration of anesthesia), duration of action of muscle relaxant, onset of action of neuromuscular blockade, time to the reversibility of neuromuscular blockade and quality of intubation conditions were all analyzed using the analysis of variance (ANOVA) and appropriate post hoc tests. Nominal categorical data (sex distribution and ASA grading) between the groups was compared using a Chi-square test. Estimated effect site with a 95% confidence interval (95% CI) is reported for both primary (duration of action of muscle relaxant) and secondary outcome variables (onset of action of neuromuscular blockade, time to reversibility of neuromuscular blockade, and quality of intubation conditions). For all statistical tests, a
The sample size was calculated using G*Power software (version 3.0.10). For each pair of neuromuscular blockers to detect at least a 20% increase in mean duration-of-action over the vecuronium and atracurium groups based on means (duration) and standard error of means as given in a study by Gibbs et al., 5 the sample size was estimated to be 14 patients in each group with a statistical power of 90% and at a significance level of 5%. A total sample size of 42, i.e., 14 patients/group was required. We enrolled 48 patients (16 per group) to account for unanticipated losses following enrolment into the study.
Results
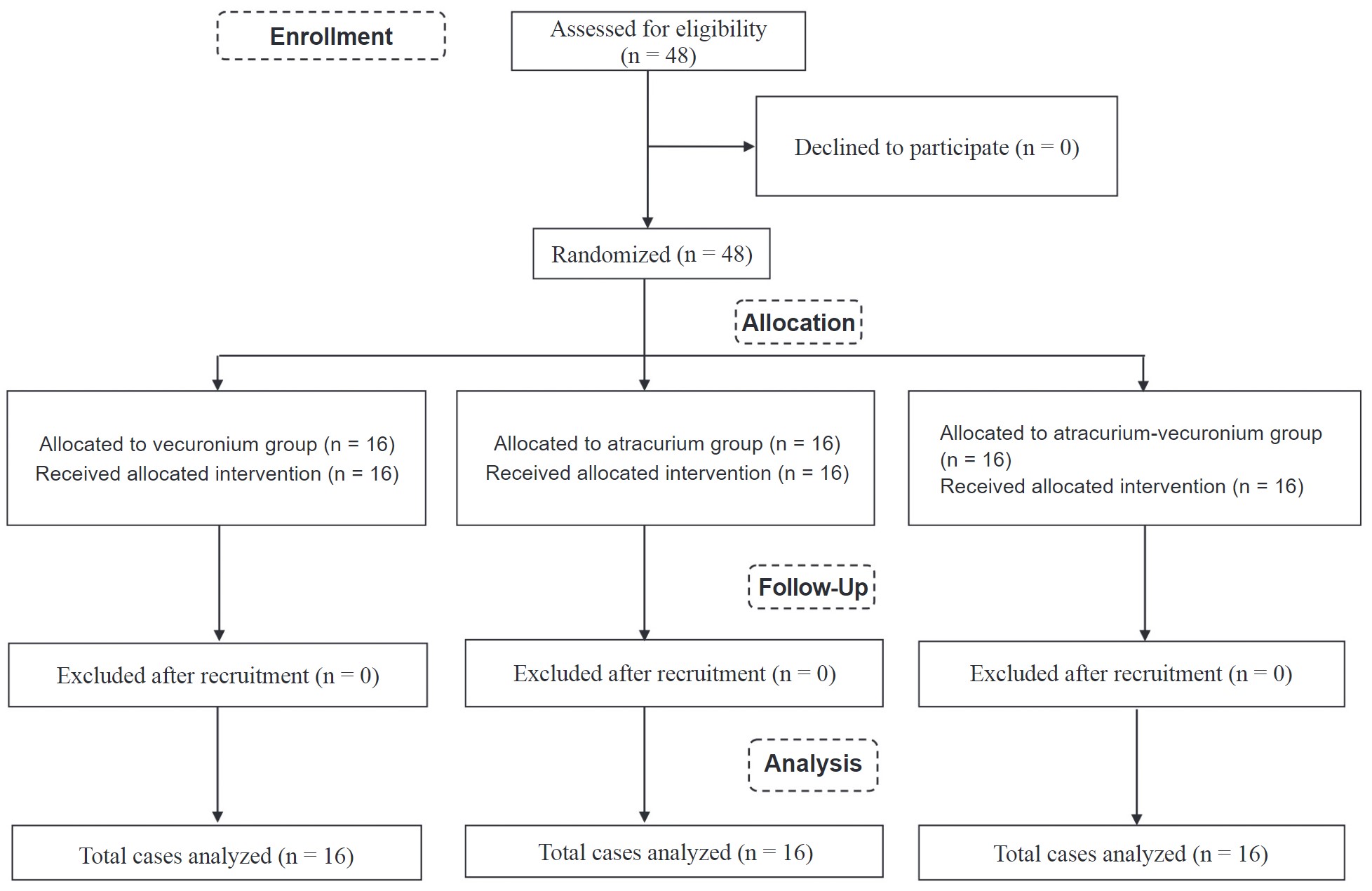
All the 48 patients enrolled in the study completed the study endpoints. The study was conducted from 20th December 2017 to 25th October 2018. This manuscript adheres to the applicable CONSORT guidelines (Figure 1).
Download full-size image
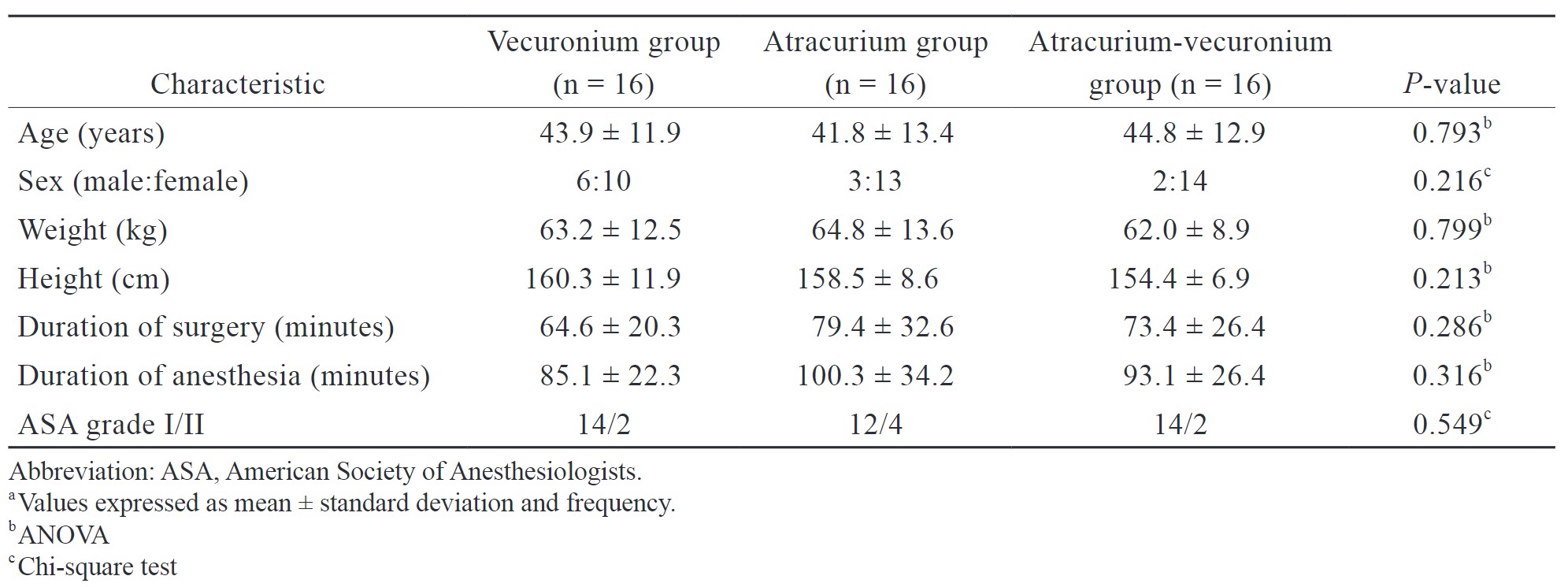
No difference was found in demographic parameters and surgical profiles between the three groups (Table 2).
Download full-size image
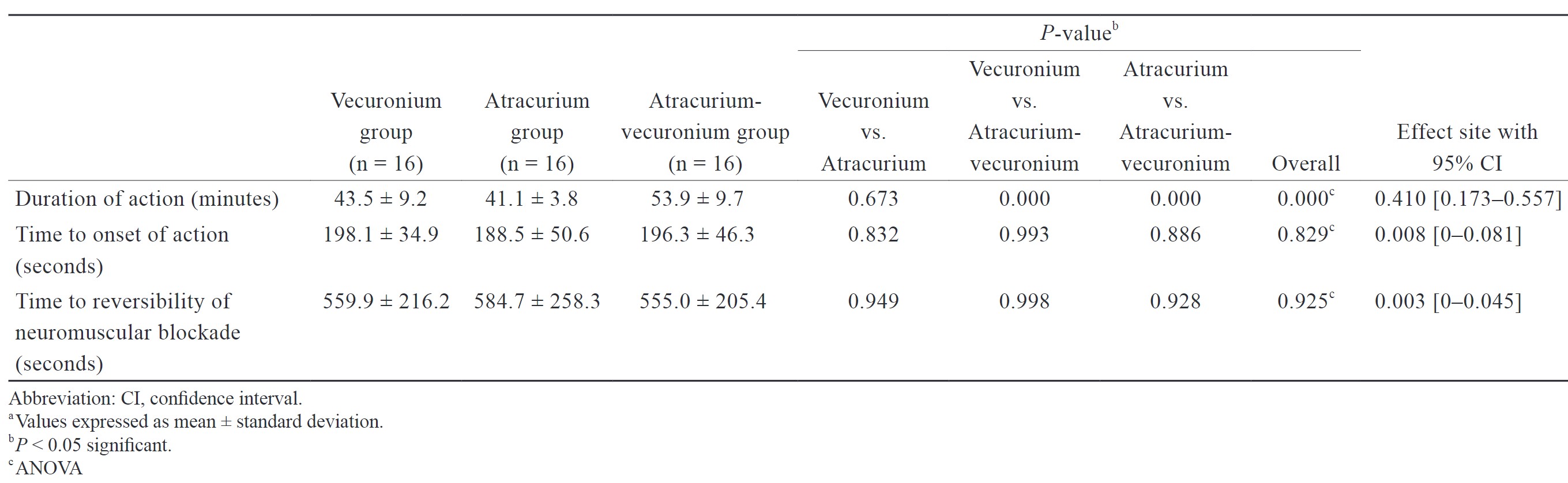
The duration-of-action of neuromuscular blockade was significantly longer in the patients who received atracurium-vecuronium combination (53.9 ± 9.7 minutes) versus those who received atracurium (41.1 ± 3.8 minutes) or vecuronium (43.5 ± 9.2 minutes) (
No difference was found in the time to onset-of-action for the three groups: vecuronium (198.1 ± 34.9 seconds), atracurium (188.5 ± 50.6 seconds), or atracurium-vecuronium combination (196.3 ± 46.3 seconds) (
No difference was found in the time taken for the reversal of muscle relaxation effect for vecuronium (559.9 ± 216.2 seconds), atracurium (584.7 ± 258.3 seconds), and atracurium-vecuronium combination (555.0 ± 205.4 seconds) (
Download full-size image
No difference was observed in the quality-of-intubating conditions as assessed on a 5-point variable scale across the three groups (vecuronium group: 9.6 ± 1.3; atracurium group: 10.0 ± 0.0; atracurium-vecuronium group: 10.0 ± 0.0) (
Download full-size image
Discussion
Laparoscopy is the go-to surgical technique for routine abdominal procedures. Of the many anesthetic considerations that the carboperitoneum situates, the requirement of d-NMB subsumes critical importance in order to provide a still operating field through the duration of surgery.9,10 Interestingly, the need for providing muscle relaxation to the very end of carboperitoneum induces a queer paradox: the intense muscle relaxation up to the termination of pneumoperitoneum leads to a considerable wait-time for reversing the residual relaxation effect, as the time to wound (trocar ports) closure takes almost no time. This paradox is more apparent during short-duration laparoscopic surgery where any additional top-up dose towards the end of surgery threatens to delay recovery from d-NMB. Contextually, to respond to the above-stated clinical paradox, either the duration of the initial intubating bolus can be increased or the reversibility of the d-NMB can be facilitated. Since, both the aspects are practically unachievable: the former (because of the ceiling effect of NMB) and the latter (lack of widespread availability of sugammadex); this randomized study explored the possibility of extending the duration of d-NMB by utilizing the evidence on synergistic effect of atracurium-vecuronium combination for increasing the duration of muscle relaxation effect in “open” surgery,5 and this randomized study was conducted to evaluate the effect of synergism on the duration of muscle relaxation effect in patients undergoing short-duration laparoscopic surgery.
The study results showed that the duration-of-action of the loading intubating bolus was significantly greater in the atracurium-vecuronium combination group (130% greater than atracurium group and 122% longer than vecuronium). The gain in the duration-of-action of atracurium –vecuronium combination (over vecuronium and atracurium alone) has greater relevance given that no difference was observed with respect to other relatable parameters of muscle relaxant effect, including the mean time to onset-of-action, quality of intubating conditions, and reversibility (reversal of neuromuscular blockade: time taken from administration of the reversal agent to recovery of TOF ratio to 0.9).
Though there is evidence on atracurium-vecuronium synergism leading to an increase in the duration-of-action of non-depolarizer muscle relaxant effect,4-7 it is largely limited to patients undergoing surgery by “open” technique. The prolongation of duration-of-action actuated by synergistic effect of atracurium-vecuronium combination in the study was similar to Black et al.11 (supra-additive neuromuscular blockade with combination of equipotent doses of atracurium and vecuronium), and Gibbs et al.5 (increased duration-of-action with half and full-dose combinations of atracurium and vecuronium). Further, while Rautoma et al.7 noted that the slopes of the dose-response curves of atracurium, vecuronium, and atracurium-vecuronium combination (in equipotent doses) were not significantly different, a significant potentiation was present with both the bolus and incremental doses. That is, the potentiation of effect gained with atracurium-vecuronium combination initial bolus was also maintained with the incremental top-up doses during the course of anesthesia. Further, they summarized that atracurium-vecuronium combination had an effect like one intermediate-acting agent and that the maximal reduction of drug consumption would be approximately 30%. However, the onset time and duration of the neuromuscular block effect of equi-dose atracurium-vecuronium combination were different when the results of Gibbs et al.’s study were compared to the present study. Gibbs et al.5’s study involved adults undergoing elective surgery under GA differed from the results of the present study on account of “onset time of neuromuscular blockade” (seconds) (atracurium alone: 170 ± 19 vs. 188.5 ± 50.6; vecuronium alone: 175 ± 22 vs. 198.1 ± 34.9; and ½ dose atracurium-vecuronium combination: 150 ± 7 vs. 196.3 ± 46.3) and “duration of neuromuscular blockade” (minutes) (atracurium alone: 36 ± 2 vs. 41.1 ± 3.8; vecuronium alone: 39 ± 3 vs. 43.5 ± 9.2; and ½ dose atracurium-vecuronium combination: 51 ± 2 vs. 53.9 ± 9.7). The “onset time” and “duration of effect” were greater in the present study for all three groups (atracurium alone, vecuronium alone, and ½ dose atracurium-vecuronium combination). The reason for the above may be accounted for by the method used to evaluate neuromuscular block effect (Gibbs et al.5 evoked electromyographic response of the adductor digiti minimi muscle versus the present study: TOF response) and genetic variability of the enrolled participants12 (Gibbs et al.5: Caucasians versus the present study: South Asians).
Although previous studies highlighted synergistic interaction between atracurium and vecuronium and studied the duration-of-action of combination muscle relaxants in various fractions of their intubating doses;5,6,11,13 they pertained to the “open” surgery context. At present, evidence on the effects of combining non-depolarizer muscle relaxants in patients undergoing “laparoscopic” surgery, though more relevant, remains limited.1,14 In light of the above, the results of the present study, i.e., increased duration-of-action of the intubating bolus of atracurium-vecuronium combination over individual drugs; reiterated the previous evidence in patients undergoing laparoscopic surgery.
Per se, the reason for this observed synergism is not clearly known. Stirt6 and Sloan et al.13 in their respective studies, concluded that the synergistic effect of atracurium and vecuronium combination could be attributed to the theory of multiple receptor sites and the intrinsic activity of different neuromuscular blocking agents.
While administration of atracurium-vecuronium combination as a single intubating bolus for a host of relevant parameters (quality of intubating conditions, increased duration-of-action, reversibility) during laparoscopic cholecystectomy was studied in detail; one of the limitations of the study was that we did not evaluate the duration-of-action of the incremental top-up dose.
To conclude, the synergistic effect of an intubating dose of atracurium-vecuronium combination brings about significantly increased duration-of-action of neuromuscular blockade, which in the face of the unaltered other relevant aspects (onset-of-action, quality of intubating conditions, reversibility); subsumes critical importance in adults undergoing short-duration laparoscopic surgery in terms of the efficacy of d-NMB and recovery from relaxant effect.
The bearing of the effects (increased duration-of-action) of the vecuronium-atracurium synergism on the frequency and duration-of-action of “top-up” dose(s) required for moderate-/long-duration laparoscopic surgery, and its overall impact on the drug consumption economics and the OR turnover rate, warrant further exploration.
Acknowledgments
None.
Conflicts of Interest
None.
Financial Support and Sponsorship
This work was supported by the Institute of Anaesthesiology, Pain & Perioperative Medicine, Sir Ganga Ram Hospital, New Delhi-110060, India
References
| 1 |
Martini CH, Boon M, Bevers RF, Aarts LP, Dahan A.
Evaluation of surgical conditions during laparoscopic surgery in patients with moderate vs deep neuromuscular block.
Br J Anaesth. 2014;112(3):498-505.
|
| 2 |
Van Wijk RM, Watts RW, Ledowski T, Troschler M, Moran JL, Arenas GW.
Deep neuromuscular block reduces intra-abdominal pressure requirements during laparoscopic cholecystectomy: a prospective observational study.
Acta Anaesthesiol Scand. 2015;59(4):434-440.
|
| 3 |
Bruintjes MH, van Helden EV, Braat AE, et al.
Deep neuromuscular block to optimize surgical space conditions during laparoscopic surgery: a systematic review and meta-analysis.
Br J Anaesth. 2017;118(6):834-842.
|
| 4 |
Van Der Spek AF, Zupan JT, Pollard BJ, Schork MA.
Interactions of vecuronium and atracurium in an in vitro nerve-muscle preparation.
|
| 5 |
Gibbs NM, Rung GW, Braunegg PW, Martin DE.
The onset and duration of neuromuscular blockade using combinations of atracurium and vecuronium.
Anaesth Intensive Care. 1991;19(1):96-100.
|
| 6 |
Stirt JA.
Accelerated recovery from combined atracurium—vecuronium neuromuscular block.
Br J Anaesth. 1989;62(6):697-699.
|
| 7 |
Rautoma P, Erkola O, Meretoja OA.
Potency and maintenance requirement of atracurium and vecuronium given alone or together.
Acta Anaesthesiol Scand. 1995;39(2):220-223.
|
| 8 |
Viby-Mogensen J, Engbaek J, Eriksson LI, et al.
Good clinical research practice (GCRP) in pharmacodynamic studies of neuromuscular blocking agents.
Acta Anaesthesiol Scand. 1996;40(1):59-74.
|
| 9 |
Koo BW, Oh AY, Seo KS, Han JW, Han HS, Yoon YS.
Randomized clinical trial of moderate versus deep neuromuscular block for low-pressure pneumoperitoneum during laparoscopic cholecystectomy.
World J Surg. 2016;40(12):2898-2903.
|
| 10 |
Raval A, Deshpande S, Rabar S, et al.
Does deep neuromuscular blockade during laparoscopy procedures change patient, surgical, and healthcare resource outcomes?
PLoS ONE. 2020;15(4):e0231452.
|
| 11 |
Black TE, Healy TE, Pugh ND, et al.
Neuromuscular block: atracurium and vecuronium compared and combined.
Eur J Anaesthesiol. 1985;2(1):29-37.
|
| 12 |
Sun Y, Zhu H, Esmaeili E, Tang X, Wu Z.
Mechanisms and implications in gene polymorphism mediated diverse responses to sedatives, analgesics and muscle relaxants.
Korean J Anaesthesiol. 2023;76(2):89-98.
|
| 13 |
Sloan MH, Bissonnette B, Lerman J.
Interaction of vecuronium and atracurium during halothane anaesthesia in children.
Anaesthesia. 1998;53(1):36-40.
|
| 14 |
Park WY, Lee KH, Lee YB, Kim MH, Lim HK, Choi JB.
Effects of combined rocuronium and cisatracurium in laparoscopic cholecystectomy.
J Lifestyle Med. 2017;7(1):35-40.
|