Abstract
Background
Advancing a tracheal tube over a tracheal tube exchanger into the trachea frequently causes difficulties because of the tube impingement on laryngeal structures. In the present study, we measured the resistance of tube advancement both objectively and subjectively with a variety of combinations of tube exchanger sizes and tracheal tubes using a manikin simulator.
Methods
Lubricated 7.5 mm ID standard and Parker Flex-Tip (PFT) tracheal tubes were railroaded over the tube exchangers (OD 1–6 mm) into the trachea through the oral route in a manikin. Consequently, 12 combinations of tracheal tube-exchanger tube assemblies were evaluated. Tube advancing resistance at the laryngeal inlet was subjectively evaluated. The objective tube advancing resistance (force) at the laryngeal inlet was evaluated using a digital force gauge. The execution of each tracheal tube-exchanger trial was conducted 10 times.
Results
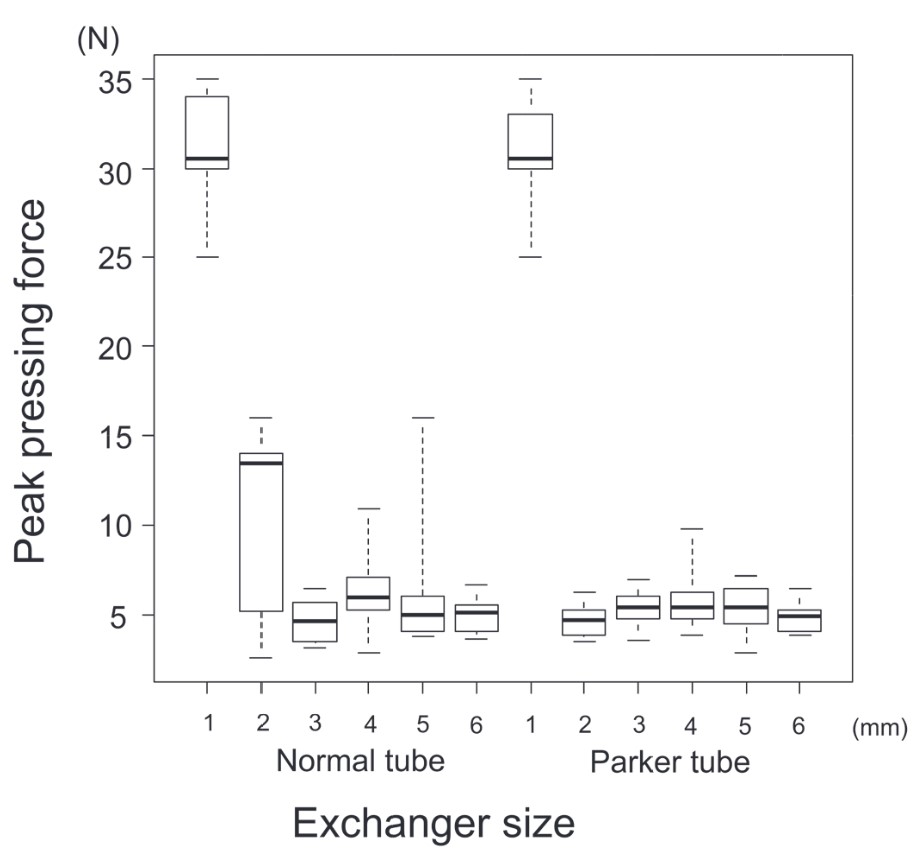
With a 1-mm tube exchanger, all intubation attempts with both standard and PFT tubes failed. Esophageal intubation or severe impingement at the right arytenoid accompanied with a bent tracheal tube was observed. With a 2-mm tube exchanger, during intubation with a standard tracheal tube, rotation of the tube was sometimes required; however, all other intubations were done without problems. When PFT tubes were used, all intubation attempts were performed without problems. The rest of the trials were successfully performed regardless of the combinations of tube exchangers and tracheal tubes; however, one attempt of intubation with a combination of a 5 mm tube exchanger and a standard tracheal tube required withdrawal and rotation of the tube because of impingement at the epiglottis. In cases where there was no gap resistance, which means tube advancing resistance generated by a gap between an introducer and a tracheal tube, the pressing force was approximately less than 10 N. However, in the cases requiring some interventions to overcome the gap, the pressing force reached around 15 N. When intubation failed, for example when the tube bent, or esophageal intubation, the pressing force reached around 30 N.
Conclusions
Impingement due to the gap between the tube exchanger and the tracheal tube is thought to occur in the PFT tube less frequently. Once an impingement occurs, we can feel approximately twice the amount of resistance as usual, which may be a chance to consider taking some interventions. When the impingement is not released, regardless of interventions, excessive force may result in esophageal intubation or tracheal injury.
Keywords
digital force gauge, impingement, tracheal tube exchanger
Introduction
Advancing a tracheal tube through a tracheal tube exchanger into the trachea frequently causes difficulties because of the tube impingement on laryngeal structures.1,2 The incidence of such difficulties may vary; however, it has been reported to be up to 90%.1 A review article of several studies has reported that the size of the fiberoptic scope as a tracheal tube introducer and the size of the tracheal tube itself affect the ease of advancing a tube over an introducer during fiberoptic intubation.1 Usually, a larger gap between the introducer and the tracheal tube can make it more difficult to advance the tube over the introducer. This is because, if the gap is large, the tube may deviate from the course of the introducer, and go into the outside of the laryngeal inlet, which may cause the tube impingement on laryngeal structures.1 However, it is still unclear how the difference between the sizes of the tube introducer and tracheal tube can affect advancing resistance. In the present study, we measured the resistance of tube advancement both objectively and subjectively with a variety of combinations of tube introducers (exchanger) of various sizes (OD 1–6 mm) and a standard tracheal tube (ID 7.5 mm) using a manikin simulator. In addition, we investigated whether the Parker Flex-Tip (PFT) tube (Parker Medical, Inc, Connecticut, USA), which has a tip pointing toward the center of the distal lumen of the tube and a smaller gap between the tube introducer and the inner wall of the tube than the standard tracheal tube, could reduce resistance to tube advancement.
Methods
To conduct this study, we created handmade tracheal tube exchangers. We purchased commercially available plastic round rods that were 40–50 cm in length (1–6 mm diameters in increments of 1 mm) and glued them together with strong glue gel to make a rod of at least 80 cm for each size so that we did not negate the flexibility of the exchanger. In addition, we were careful not to change the diameter at the joint. A CAE Apollo, which is an adult patient simulator (CAE Corporate, Québec, Canada), was used for orotracheal intubation by these hand-made tube exchangers. The laryngoscope blade (Macintosh size 3) was fixed into position using a retort stand and a clamp,3 so that the same fixed laryngeal exposure could be provided for each intubation. In addition, a laryngoscope is preferred because it is more effective at reducing tube impingement on airway structures when trachea tube exchange via a tube exchanger is performed.4 Another reason why a laryngoscope blade was fixed into position using a retort stand and a clamp was because the deviation between the course of the tracheal tube and that of the tube exchanger should be set equal for each intubation as much as possible.
A lubricated 1-mm diameter tube exchanger was inserted into the manikin via the right corner of the mouth through the trachea, using a pair of Magill forceps. Unlike commercially available tube introducers, our handmade tube exchangers were straight shapes, which required the forceps for introduction to the trachea. The tracheal placement was confirmed using a fiberoptic scope (Ambu aScope 4 Regular, Ambu, Ballerup, Denmark) through the left nasal route. Then, a lubricated 7.5 mm ID standard tracheal tube (Shiley Endotracheal Tube, Medtronic, MN, USA) was railroaded over the exchanger into the trachea. Again, tracheal or esophageal placement was confirmed using a fiberoptic scope. During the procedures, manipulation of the laryngoscope, alteration of the head position, or application of external laryngeal pressure was not performed. When the tracheal tube was successfully placed into the trachea, the exchanger was removed and a lubricated 2-mm diameter exchanger was re-inserted through the intubated tube. When intubation using a 1-mm diameter tube exchanger was not done properly, both the tube and exchanger were removed, and a 2-mm diameter tube exchanger was inserted into the trachea. Then, a lubricated 7.5 mm ID standard tracheal tube was railroaded over the tube exchanger into the trachea. The same procedures were repeated until the procedure for a 6-mm diameter tube exchanger was completed. Next, the same procedures were repeated using a 7.5 mm ID PFT tube. As a result, 12 combinations of tracheal tube-exchanger tube assemblies were evaluated.
Assessment
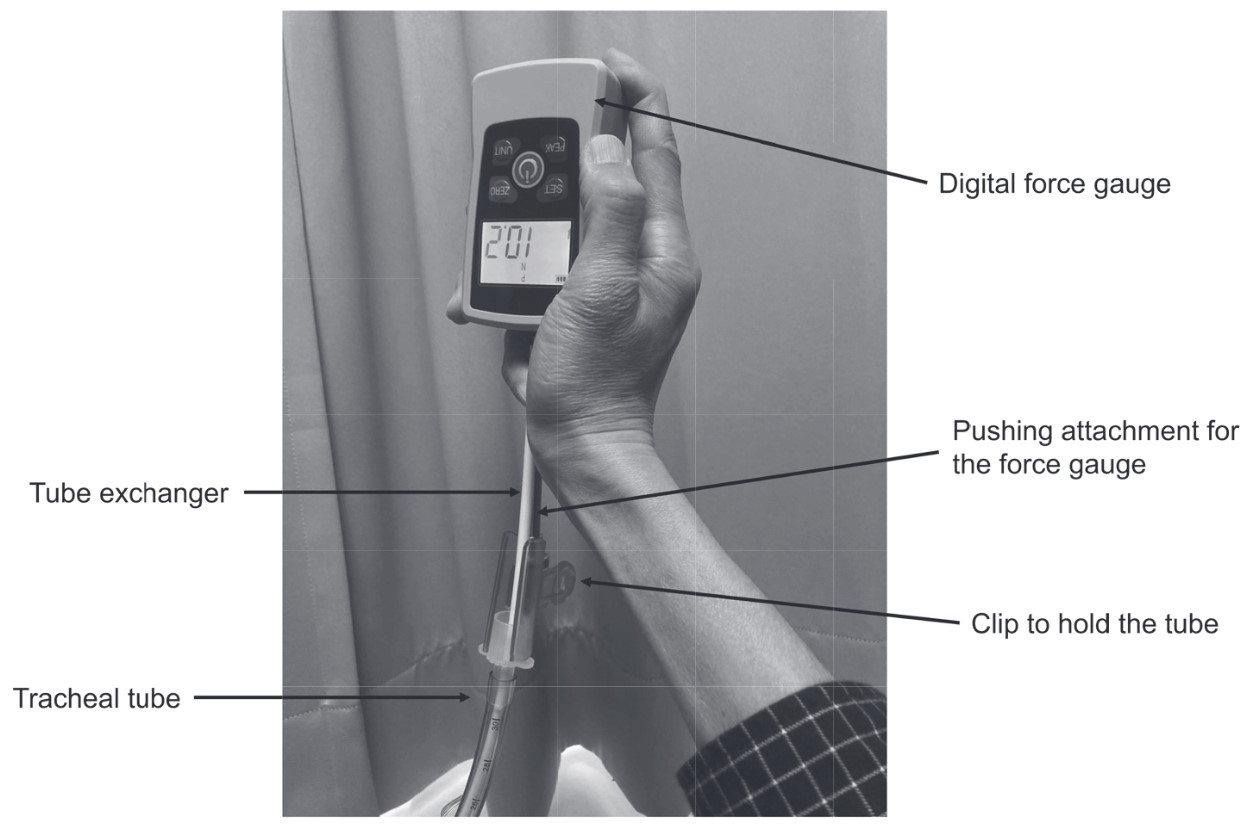
The subjective tube advancing resistance at the laryngeal inlet was evaluated as follows: (1) little-to-no gap resistance encountered; (2) smooth gap resistance encountered; (3) significant gap resistance encountered with rotation of the tube required; (4) very significant gap resistance encountered with withdrawal and rotation of the tube required; or (5) unsuccessful intubation. The objective tube advancing resistance (force) at the laryngeal inlet was evaluated by a digital force gauge (AMF-500, Beslands, China), which had 0.1 N of resolution. When a tracheal tube was railroaded over the tube exchanger, a clip was attached at the slip joint of the tracheal tube, which could mimic being held manually (Figure 1). Then, the clip was pushed using an attachment with the digital force gauge to advance the tube while the advancing pressure force was measured until the tip of the tube was advanced to the laryngeal inlet. Reaching the laryngeal inlet was confirmed when there was a certain amount of resistance felt and by the fiberoptic scope from the left nasal route. Next, the peak pressing force was measured when the tracheal tube was advanced over the gap at the laryngeal inlet. In cases where resistance was felt and there was difficulty advancing the tube, rotation, or withdrawal and rotation, of the tube was attempted. The peak pressing force during these interventions was recorded. Whenever there was little-to-no resistance, the peak pressing force during the whole intubating procedure was recorded. For each combination of the tracheal tube and the tube exchanger of various sizes, subjective and objective evaluations were each done ten times.
Download full-size image
Statistical Analysis
All measured values are described in a scatter diagram or box plots. For subjective and objective evaluations, comparisons between the combinations were analyzed by the Kruskal-Wallis test followed by the same test corrected using the Bonferroni-Holm method. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University), which is based on R (The R Foundation for Statistical Computing) and R commander,5 and
Results
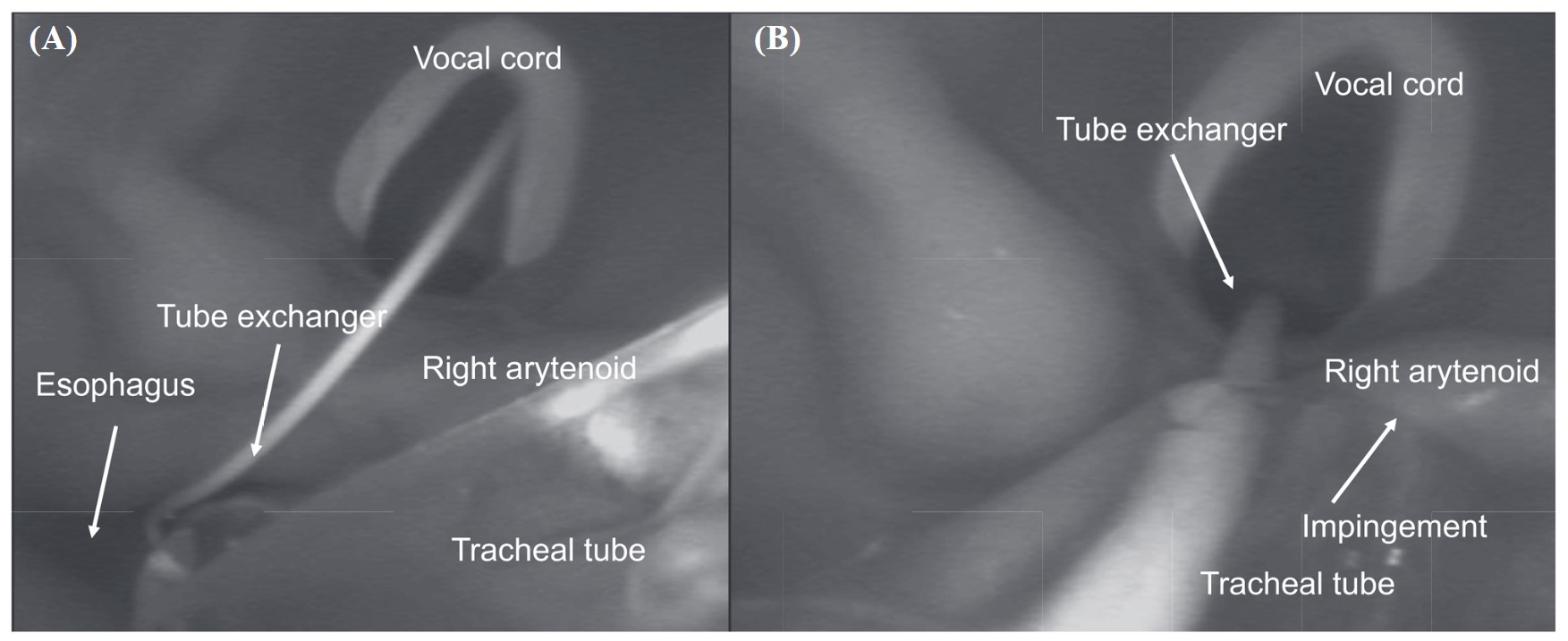
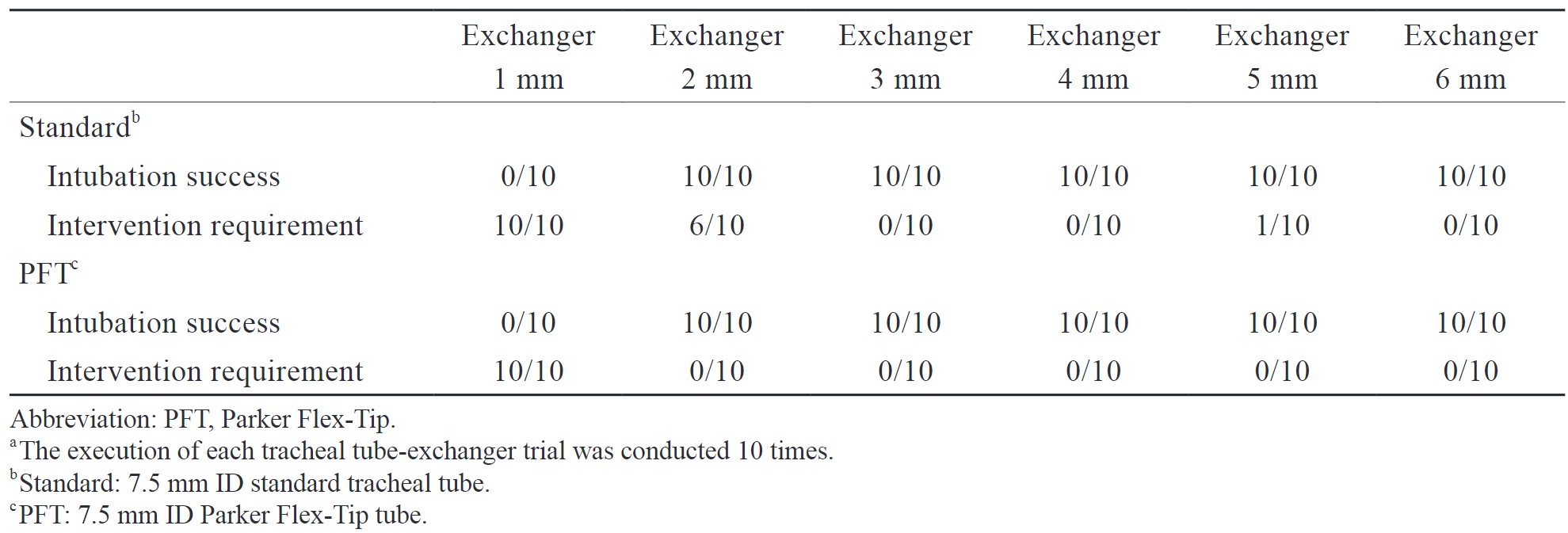
With the 1-mm tube exchanger, all intubation attempts with both standard and PFT tubes failed. Esophageal intubation was observed twice in the standard tube and three times in the PFT tube, respectively (Figure 2A shows a typical case of esophageal intubation with the tube exchanger bending by excessive pressing force). The others were severely impinged at the right arytenoid (Figure 2B shows a typical case of tracheal tube impingement at the right arytenoid), resulting in the bending of the tracheal tube by additional pressing force. When the 2-mm tube exchanger was used, intubation with a standard tracheal tube, rotation of the tube was required for six attempts; however, in the four remaining attempts, intubation was successfully done without problems. In cases with a PFT tube, all intubation attempts were successfully performed without problems. The rest of the trials were successfully performed regardless of combinations between exchangers and tubes; however, one attempt of intubation with a 5-mm tube exchanger and a standard tracheal tube required withdrawal and rotation of the tube because of impingement at the epiglottis. Combinations of the tracheal tube-exchanger tube assembly and the number of successful intubations and interventions required are summarized in Table 1. Except for the impingement at the epiglottis, all other impingements occurred at the right arytenoid.
Download full-size image
Download full-size image
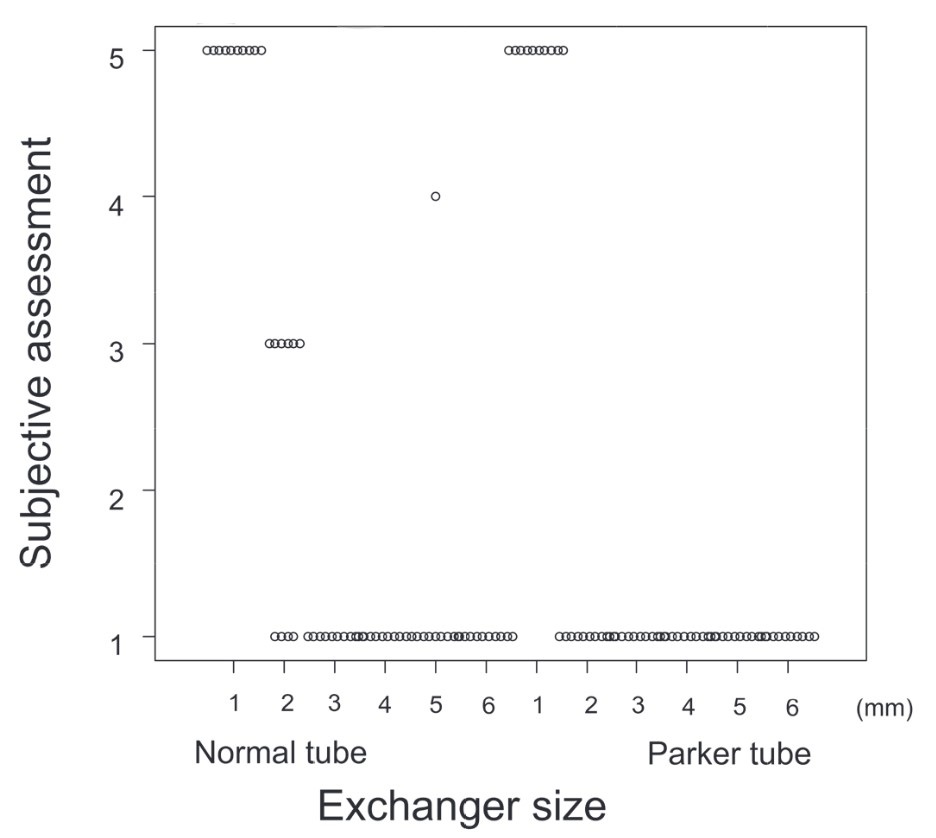
Regarding the subjective assessment, the scores with the 1-mm tube exchanger in both standard and PFT tubes were significantly higher than those with other tube exchangers (
Download full-size image
Regarding the measurement of peak pressing force, in the case of a lack of gap resistance, the pressing force was approximately less than 10 N. However, in the cases requiring interventions to overcome the gap, the pressing force reached around 15 N. In cases of failed intubation, which resulted in the tube bending, or esophageal intubation, the pressing force reached around 30 N.
Regarding comparisons about the pressing force, the peak forces with the 1-mm tube exchanger in both standard and PFT tubes were significantly higher than those of the other tube exchangers (
Download full-size image
Discussion
In the present study, failed intubation due to impingement occurred only when using the thinnest and softest tube exchanger. The second thinnest exchanger caused some difficulties in advancing the tracheal tube in the case of a standard tube, but all intubations were completed. Conversely, when using the same second-thinnest tube exchanger, all intubations were completed without problems with the PFT tube. In addition, even with a relatively thick tube exchanger, severe impingement occurred in the standard tube. However, it may have occurred accidentally because this happened only once during 40 attempts with tube exchangers larger than 3 mm. However, it may deserve special consideration that the impingement in that instance occurred at the epiglottis while all other impingements occurred at the right arytenoid. It is worth noting that the presence of an impingement lets us feel roughly twice the amount of resistance as usual, and this may provide an opportunity to consider interventions such as rotation and/or withdrawal of the tube. When further resistance is present, even with intervention, failed intubation may occur, suggesting a mismatch between the tube exchanger and the tracheal tube.
Jackson et al.2 reported that impingement could occur at the right arytenoid, left arytenoid, epiglottis, interarytenoid tissue, and/or the left pyriform fossa. In this simulation study using a manikin, the impingement almost solely occurred at the right arytenoid, most likely because we used the equal condition for the relationship between the course of the tracheal tube and that of the tube exchanger. Conversely, Katsnelson et al.6 observed that the epiglottis was the main site of impingement during fiberoptic nasotracheal intubation in their study using manikins. It is likely that this discrepancy was due to the intubation route, resulting in a difference regarding the position of the epiglottis on the axis of intubation alignment. However, when 5-mm diameter tube exchangers were used for the conventional tracheal tube, impingement occurred at the epiglottis once. This may occur by chance; however, we need to keep in mind that the epiglottis is one of the main impingement sites of intubation through the tube exchanger.
When a 1-mm tube exchanger was used, the tracheal tube sometimes slipped into the esophagus when advanced to overcome any resistance. When the tube was advanced further to overcome the resistance, it was consequently inserted deeper into the esophagus, and then the tube exchanger was pulled out of the trachea into the esophagus or was completely bent (Figure 2B). Regarding this phenomenon, Asai and Shingu1 reported that this was also observed when fiberoptic intubation was performed with relatively thin and flexible fiberoptic scopes for the tracheal tubes. This phenomenon never occurred in our study when tube exchangers with diameters larger than 2 mm were used because the larger diameters of the tube exchangers remained in place due to their stiffness. Jackson et al.2 also reported that impingement in the pyriform fossa only occurred when a relatively thin and flexible intratracheal device was used. They confirmed that the tracheal tube and tube introducer were both displaced from the midline into the pyriform fossa. Therefore, attempting to advance the tracheal tube into the trachea from this position was impossible.2 In the case of a failed intubation without esophageal insertion, the tracheal tube was bent and not advanced. In those instances, the pressure gauge showed around 30 N. It is unclear whether that much pressure can be applied in a real clinical practice; it is reasonable to think that using enough pressure to bend the tracheal tube can injure the tracheal inlet. For example, an arytenoid cartilage dislocation or a tracheal tear may occur.
This was an experimental study using a manikin simulator. Therefore, it is not certain whether the obtained results can be applied to clinical settings. The alignments of the oral, pharyngeal, and laryngeal axes may be different from person to person. Therefore, the gap formation between the tracheal tube and tube exchanger may vary depending on each person. In addition, we measured the pressing force needed to advance the tracheal tube; it is still unclear whether these measured values are similar to real-world values. However, the perception of around twice as much resistance as usual when advancing a tracheal tube in the presence of an impingement may not be so different between a simulation and a real world situation. In addition, we reconfirmed that the PFT tube was superior to the conventional tube regarding the advancement of a tracheal tube through a tube exchanger.1,7,8 It is reasonable to say that our experiment was appropriately conducted and reliable. Lastly, a laryngoscope blade with a fixed position was used, as described previously, to make intubation easier.4 Without laryngoscopic assistance, we might have felt gap resistance more frequently even with exchangers with larger diameters. Even in that case, we think that we would have felt the same gap resistance, which would have required some interventions or resulted in failed intubation like some cases in this study. Moreover, we think that tube exchange without laryngoscopic assistance is quite unrealistic because it is evident that trachea tube exchange via a tube exchanger makes intubation easier.4
In conclusion, impingement due to the gap between the tube exchanger and tracheal tube likely occurs less frequently when using a PFT tube compared with the standard tracheal tube. Whenever larger sizes of tube exchangers are used, it is less likely that impingement will occur. Once impingement occurs, we feel roughly twice the amount of resistance as usual, which may be an opportunity to consider taking some interventions. When the impingement is not released regardless of interventions, excessive force may result in esophageal intubation or tracheal injury.
Acknowledgments
The authors acknowledge the Scientific English Editing Section of Fukushima Medical University for their proofreading.
Conflict of Interest
None of the authors declare any conflict of interest, financial or otherwise, in the results of the study.
References
| 1 |
Asai T, Shingu K.
Difficulty in advancing a tracheal tube over a fibreoptic bronchoscope: incidence, causes and solutions.
Br J Anaesth. 2004;92(6):870-881.
|
| 2 |
Jackson AH, Orr B, Yeo C, Parker C, Craven R, Greenberg SL.
Multiple sites of impingement of a tracheal tube as it is advanced over a fibreoptic bronchoscope or tracheal tube introducer in anaesthetized, paralysed patients.
Anaesth Intensive Care. 2006;34(4):444-449.
|
| 3 |
Annamaneni R, Hodzovic I, Wilkes AR, Latto IP.
A comparison of simulated difficult intubation with multiple-use and single-use bougies in a manikin.
Anaesthesia. 2003;58(1):45-49.
|
| 4 |
Mort TC.
Tracheal tube exchange: feasibility of continuous glottic viewing with advanced laryngoscopy assistance.
Anesth Analg. 2009;108(4):1228-1231.
|
| 5 |
Kanda Y.
Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics.
Bone Marrow Transplant. 2013;48(3):452-458.
|
| 6 |
Katsnelson T, Frost EAM, Farcon E, Goldiner PL.
When the endotracheal tube will not pass over the flexible fiberoptic bronchoscope.
Anesthesiology. 1992;76(1):151-152.
|
| 7 |
Kristensen MS.
The Parker Flex-Tip tube versus a standard tube for fiberoptic orotracheal intubation: a randomized double-blind study.
Anesthesiology. 2003;98(2):354-358.
|
| 8 |
Makino H, Katoh T, Kobayashi S, Bito H, Sato S.
The effects of tracheal tube tip design and tube thickness on laryngeal pass ability during oral tube exchange with an introducer.
Anesth Analg. 2003;97(1):285-288.
|