Abstract
We read with great interest the systematic review and meta-analysis by Sharapi et al.
1
comparing the safety and effectiveness of VivaSight double-lumen tubes (VS-DLTs) versus conventional double-lumen tubes (c-DLTs) for one-lung ventilation. The authors included 6 randomized controlled trials with a total of 364 patients and found that VS-DLT was associated with significantly shorter intubation time compared to c-DLT (mean difference = –90.01 seconds;
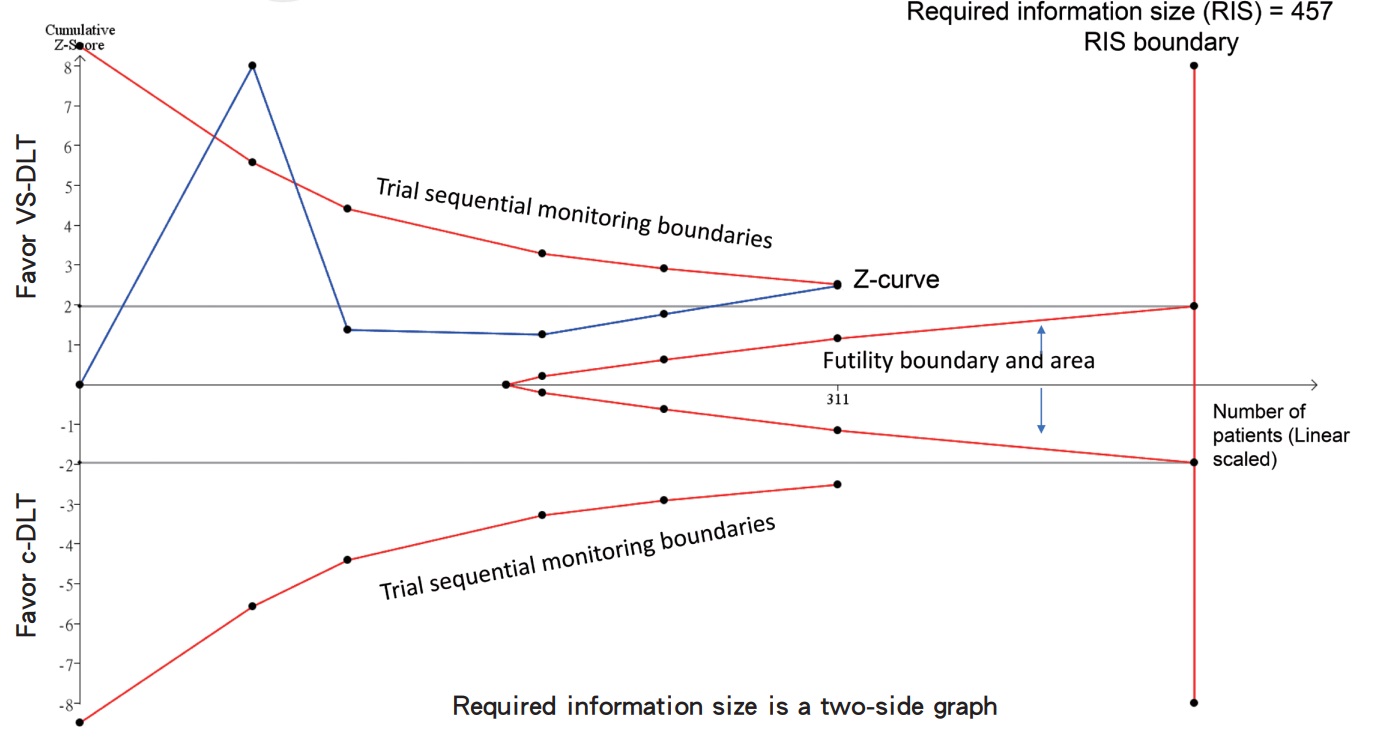
The finding of a shorter intubation time with VS-DLT is clinically important 1 , as patients requiring one-lung ventilation often have underlying lung disease and may not tolerate prolonged intubation well. However, given that the relatively small number of trials are included, we believe that applying trial sequential analysis (TSA) could help validate the reliability of this key finding. TSA is a methodology that combines an information size calculation (cumulated sample sizes of all included trials) with the threshold of statistical significance. 2-4 It helps determine whether the evidence of a meta-analysis is robust. Interpretations based on TSA are a sample. First, the required information size was calculated by the TSA software based on the anticipated intervention effect, variance of the outcome, acceptable risks of type I and type II errors, and heterogeneity adjustment. The required information size represents the minimum number of patients needed in a meta-analysis to detect or reject a certain intervention effect while minimizing the risks of type I and type II errors. However, even though the cumulative sample size in the original meta-analysis has not reached the required information size, the crossing of the monitoring boundary by the Z-curve suggests that the evidence may be sufficient to draw a reliable conclusion. In summary, if the cumulative Z-curve crosses the trial sequential monitoring boundary or the required information size, a sufficient level of evidence has been reached.
To address this, we collected raw intubation time data from the included studies and performed TSA using dedicated software (version 0.9.5.10 beta) (Copenhagen Trial Unit, Centre for Clinical Intervention Research, Rigshospitalet, Copenhagen, Denmark). As shown in Figure 1, although the total sample size (i.e., 364 patients) in the meta-analysis by Sharapi et al. 1 did not reach the required information size (i.e., 457 patients) as calculated by the TSA, the cumulative Z-curve crosses the trial sequential monitoring boundary, suggesting that the current evidence for shorter intubation times with VS-DLT is likely reliable. In conclusion, this well-conducted meta-analysis provides important insights into the potential advantages of VS-DLT over c-DLTs, especially regarding intubation time. Our TSA results support the reliability of this key finding.
Download full-size image
The risk of a type 1 error was maintained at 5% with 80% power. The variance was calculated from the data obtained from the included trials.
Acknowledgments
None.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
| 1 |
Sharapi M, El-Samahy M, Rizk MA, Gadallah A, Mouffokes A, Albakri K.
VivaSight double-lumen tube versus conventional double-lumen tube for one-lung ventilation: a systematic review and meta-analysis of randomized controlled trials.
Asian J Anesthesiol. 2023;61(2):46-60.
|
| 2 |
Clephas PRD, Kranke P, Heesen M.
How to perform and write a trial sequential analysis.
Anaesthesia. 2023;78(3):381-384.
|
| 3 |
Liu Q, Ding L, Qiu X, Meng F.
Updated evaluation of endoscopic submucosal dissection versus surgery for early gastric cancer: a systematic review and meta-analysis.
Int J Surg. 2020;73:28-41.
|
| 4 |
Hung KC, Wu SC, Chang PC, et al.
Impact of intraoperative ketamine on postoperative analgesic requirement following bariatric surgery: a meta-analysis of randomized controlled trials.
Obes Surg. 2021;31(12):5446-5457.
|