Abstract
Objective
Sepsis-related systemic inflammation resulted in microcirculatory dysfunction. However, information of normal ranges of microcirculatory parameters in the healthy population remain limited. The primary aim of this study was to investigate the differences in microcirculatory parameters between healthy volunteers and patients with sepsis.
Methods
This observational study enrolled 45 healthy female and 45 healthy male volunteers, and divided them equally into three age groups: young (20−39 years), middle-age (40−59 years), and elderly (60−79 years). In addition, we enrolled 32 patients with sepsis. Images of sublingual microcirculation were obtained through sidestream dark field videomicroscopy and were analyzed using automated analysis software. Microcirculation parameters, namely the total small vessel density (TSVD), perfused small vessel density (PSVD), proportion of perfused vessel (PPV), microvascular flow index (MFI) score, and heterogeneity index (HI), were evaluated. One-to-one matching between the septic patients and the healthy volunteers was performed on the basis of demographic data including age and gender.
Results
The elderly group had lower MFI scores and a higher HI. Age was positively correlated with the HI (r = 0.38, p < 0.001) and negatively correlated with the PPV and MFI scores (r=-0.26, p=0.014 and r=-0.37, p < 0.001, respectively). TSVD was higher in female participants than in male participants. Body mass index (BMI) was negatively correlated with TSVD. In multivariate regression analysis, the independent factors associated with PPV are age and sex, however age is the only independent factor associated with MFI and HI. In patients with sepsis, TSVD (17.5 [3.3] vs. 21.7 [3.0]; p=0.002), PSVD (15.0 [3.0] vs. 21.1 [2.5]; p < 0.001), and MFI score (2.0 [1.6−2.5] vs. 2.9 [2.5−3.0]; p < 0.001) were lower in the 28-day nonsurvivors than in the survivors. Matched comparison revealed that the TSVD (20.7 [3.7] vs. 25.2 [2.3]; p < 0.001), PSVD (19.8 [3.0] vs. 24.3 [2.7]; p < 0.001), and MFI score (2.7 [2.4−3.0] vs. 3.0 [2.7−3.0]; p=0.019) were lower in the patients with sepsis than in the healthy volunteers.
Conclusion
Age and sex were correlated with microcirculatory parameters of the healthy volunteers. In the patients with sepsis, microcirculatory dysfunction was more severe in the 28-day nonsurvivor group than in the 28-day survivor group. Furthermore, the patients with sepsis exhibited significantly lower TSVD, PSVD, and MFI scores than the healthy volunteers.
Keywords
microcirculation; sepsis; shock;
1.Introduction
Sepsis-related systemic inflammatory response syndrome may cause excess vasodilation, resulting in hypotension. Activated endothelial cells may secrete inflammatory chemokines, which could increase microvascular permeability, leading to capillary leakage and tissue edema.1 Endotoxins activate the coagulatory functions of endothelial cells, resulting in microvascular thrombosis.2 Excess vasodilation, capillary leakage, and microvascular thrombosis can result in microcirculatory dysfunction, which leads to tissue hypoperfusion and ultimately multiple organ dysfunction syndrome and death. Videomicroscopic techniques have facilitated the observation of sublingual microcirculatory anomalies in patients with sepsis.3,4
Recent clinical trials have focused on microcirculation changes in patients with severe sepsis,5-7 however, information on normal ranges of microcirculatory parameters in the healthy population is very limited. Furthermore, the treatment targets for microcirculatory parameters in patients with sepsis remains unknown. Moreover, microcirculatory conditions probably differ among races. The primary aim of this study was to investigate the differences in microcirculatory parameters between healthy volunteers and patients with sepsis. First, this study investigated sublingual microcirculation in healthy volunteers of different age groups and evaluated the correlation between participants’ baseline characteristics and microcirculatory parameters. Second, this study enrolled patients with sepsis and compared the microcirculatory parameters of 28-day nonsurvivor and survivor groups. Finally, this study investigate the differences in microcirculatory parameters between healthy volunteers and patients with sepsis using a matched comparison.
2.Methods
Enrollment and Matching
This observational study was approved by the Research Ethics Committee of National Taiwan University Hospital, and was registered on the ClinicalTrials.gov Protocol registration system (healthy volunteers, ID: NCT02359682; patients with sepsis, ID: NCT00808691). The authors assured and certified that this research has been conducted in accordance with all of the ethics standards required by the Declaration of Helsinki issued in 2013. The inclusion criteria for healthy volunteers were an age of 20−79 years and a body mass index (BMI) ranging from 18.5 to 27 kg/m2. The exclusion criteria for healthy volunteers were a systolic blood pressure (SBP) > 140 mmHg, diastolic blood pressure (DBP) > 95 mmHg, or SBP < 90 mmHg; body temperature> 37.5 °C or < 35.5 °C at enrollment; and diagnosis of any one of the following diseases: hypertension, diabetes mellitus, peripheral arterial occlusive disease, coronary arterial disease, liver cirrhosis, chronic kidney disease, stroke, anemia, asthma, chronic bronchitis, metabolic diseases, hematologic diseases, uncured cancer, and other diseases that may limit daily activities. Finally, 45 healthy female and 45 healthy male volunteers were enrolled and divided equally into three age groups: young (20−39 years), middle-aged (40−59 years), and elderly (60−79 years). The baseline heart rate (HR), blood pressure, and body temperature were recorded. Sublingual microcirculation was examined through sidestream dark-field (SDF) videomicroscopy (MicroScan, Microvision Medical, Amsterdam, The Netherlands). The inclusion criteria for patients with sepsis were an age elder than 20 years, admission to an intensive care units (ICU), and diagnosis of severe sepsis or septic shock. The exclusion criteria were inability to undergo sublingual microcirculation examination (e.g., limited mouth opening); hemoglobin < 9 g/dL and transfusion refusal; and the patient’s (or next of kin) refusal to participate. Severe sepsis and septic shock were treated according to the practice guidelines for severe sepsis and septic shock. The sublingual microcirculatory parameters were examined using a SDF video microscope at 24 h after severe sepsis or septic shock onset. HR and mean arterial pressure (MAP) were recorded at 24 h. The patients with sepsis were divided into survivor and nonsurvivor groups based on their survival status at 28 days after severe sepsis or septic shock onset. One-to-one matching of patients with sepsis and healthy volunteers was performed on the basis of demographic data, including age and sex.
Sublingual Microcirculatory Parameters Measurements
Five video sequences (20 s) were obtained from different sublingual sites and digitally stored with code numbers that did not reveal participant information for later offline analysis by using automated analysis software (AVA 3.0, Academic Medical Centre, University of Amsterdam, Amsterdam, The Netherlands). The following microcirculatory parameters were investigated: total small vessel density (TSVD, vessel diameter < 20 mm), perfused small vessel density (PSVD), proportion of perfused vessels (PPV), microvascular flow index (MFI) score, and heterogeneity index (HI). TSVD was calculated using the automated analysis software. The PSVD, PPV, MFI scores, and HI were obtained according to the methods described in our previous study.8
Statistical Analysis
Statistical analyses were performed using SPSS 20 (IBM, Armonk, NY, USA). Continuous data were presented as the mean (standard deviation) or median (interquartile range) where appropriate. Categorical data were summarized as discrete values and percentages (n [%]). Continuous variables were compared using the Student’s t-test or Mann-Whitney test. Categorical samples were compared using the Fisher’s exact test or χ2 test. Analysis of variance (ANOVA) or the Kruskal-Wallis test was used to evaluate the microcirculatory parameters among the three groups of healthy volunteers. The correlation between sublingual microcirculatory parameters and baseline characteristics was evaluated using the Pearson correlation test. Multivariate regression analysis was used to find independent factors associated with microcirculatory parameters. All p values were two tailed, and p < 0.05 was considered statistically significant.
3.Results
Baseline Characteristics and Microcirculatory Parameters of Healthy Volunteers
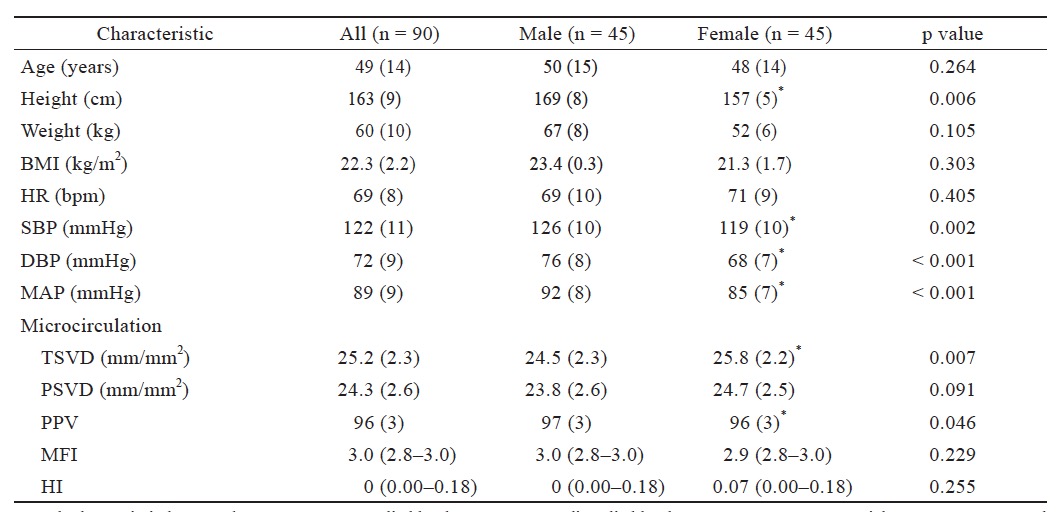
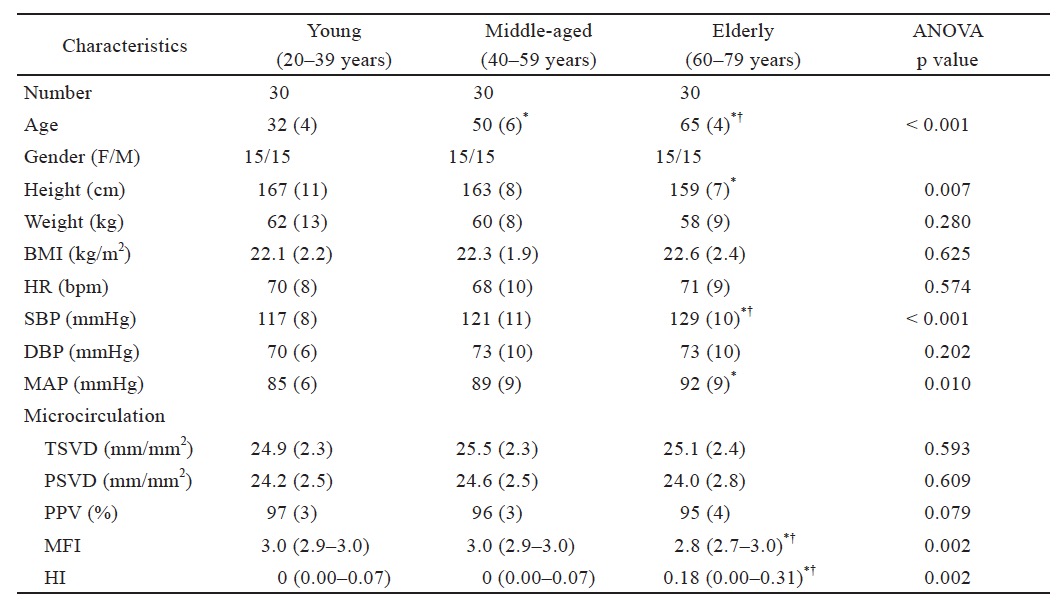
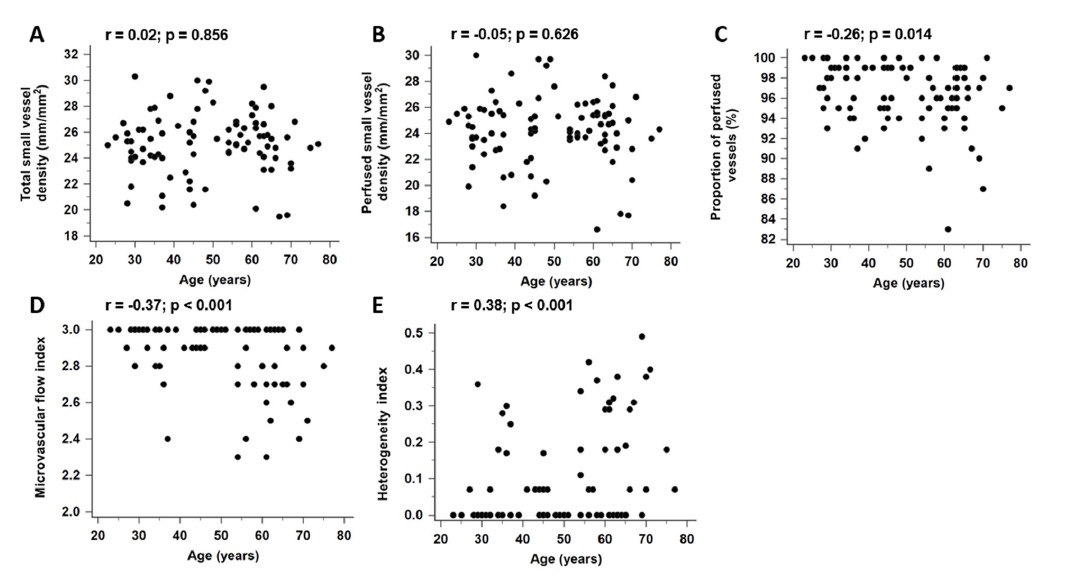
Table 1 shows the baseline characteristics and microcirculatory parameters of the healthy volunteers. Table 2 presents the microcirculatory parameters of the healthy volunteers in the three age groups. SBP and MAP were higher in the elderly group than in the young group. The HI was higher and MFI scores were lower in the elderly group than in the young and middle-aged groups. The other microcirculatory parameters did not differ significantly among the three groups. Age was positively correlated with the HI (r = 0.38, p < 0.001) and negatively correlated with the PPV and MFI scores (r=-0.26, p=0.014 and r=-0.37, p < 0.001, respectively; Fig. 1 ).
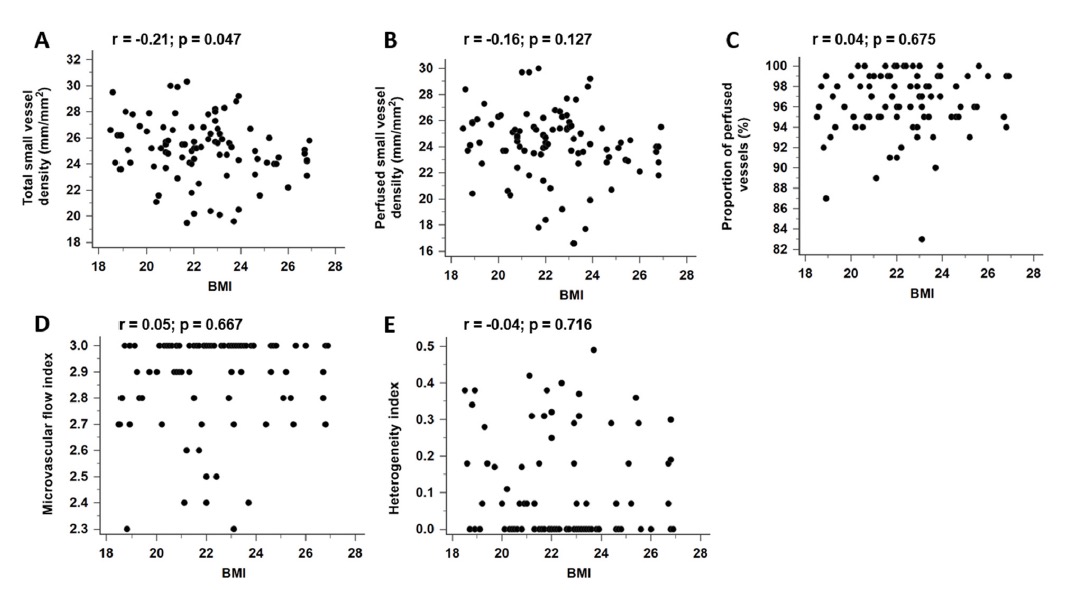
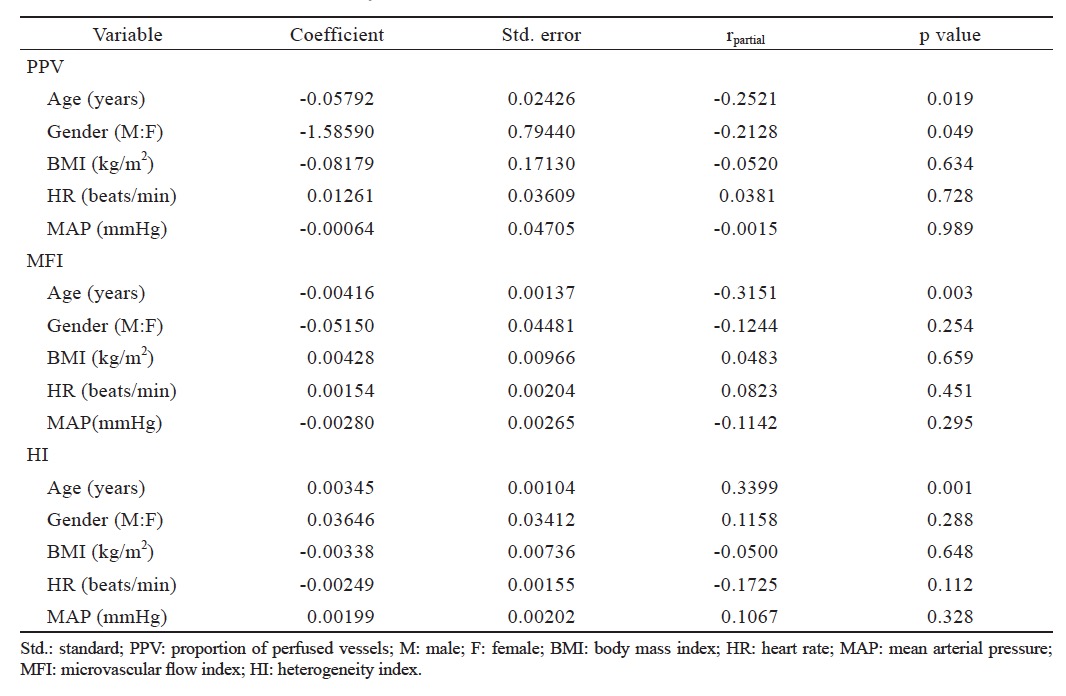
SBP, DBP, and MAP were higher in male participants than in female participants. TSVD was higher in female participants than in male participants (Table 1 ). However, the PPV was lower in female participants than in male participants. BMI was negatively correlated with TSVD (r = -0.21, p = 0.047; Fig. 2). Table 3 revealed that age and sex are independent factor of PPV in multivariate regression analysis. And the only independent factor associated with MFI and HI is age.
Download full-size image
Data are represented as the mean (standard deviation) or median (interquartile range).
*p < 0.05 vs. male.
Download full-size image
MFI: microvascular flow index; HI: heterogeneity index.
Data are represented as the mean (standard deviation) or median (interquartile range).
*p < 0.05 vs. young group; †p < 0.05 vs. middle-aged group.
Download full-size image
Download full-size image
Download full-size image
Baseline Characteristics and Microcirculation of Septic Patients
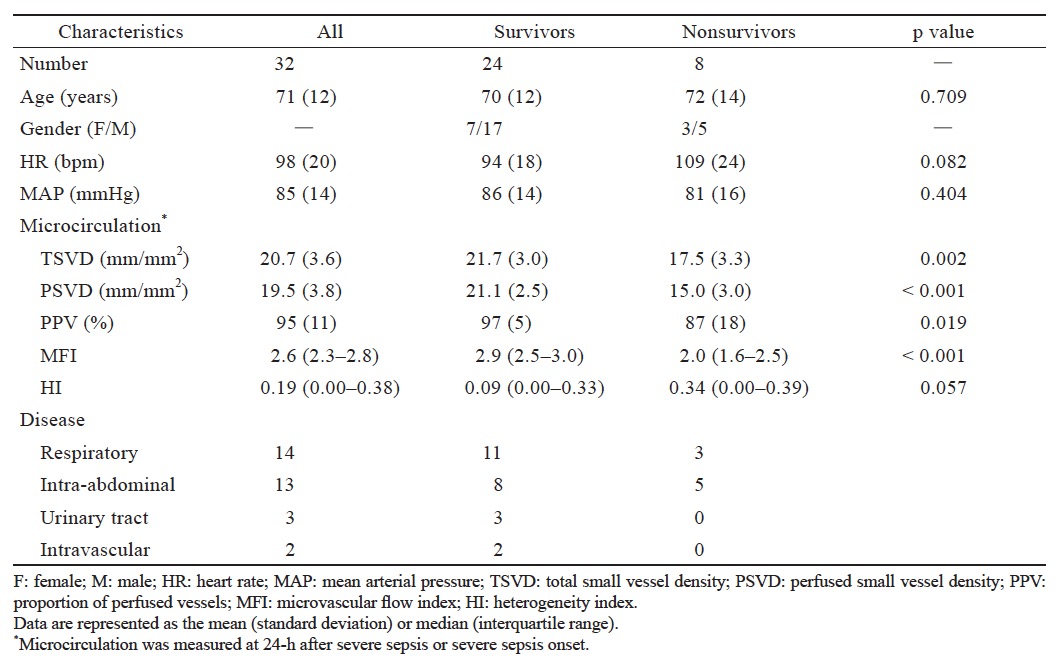
Table 4 presents the baseline characteristics and microcirculatory parameters of the 32 septic patients with sepsis at 24-h. After 24-h resuscitation of severe sepsis and septic shock, HR and MAP did not differ between the 28-day nonsurvivor and survivor groups. However, TSVD, PSVD, and MFI score were lower in the 28-day nonsurvivor group than in the 28-day survivor group.
Download full-size image
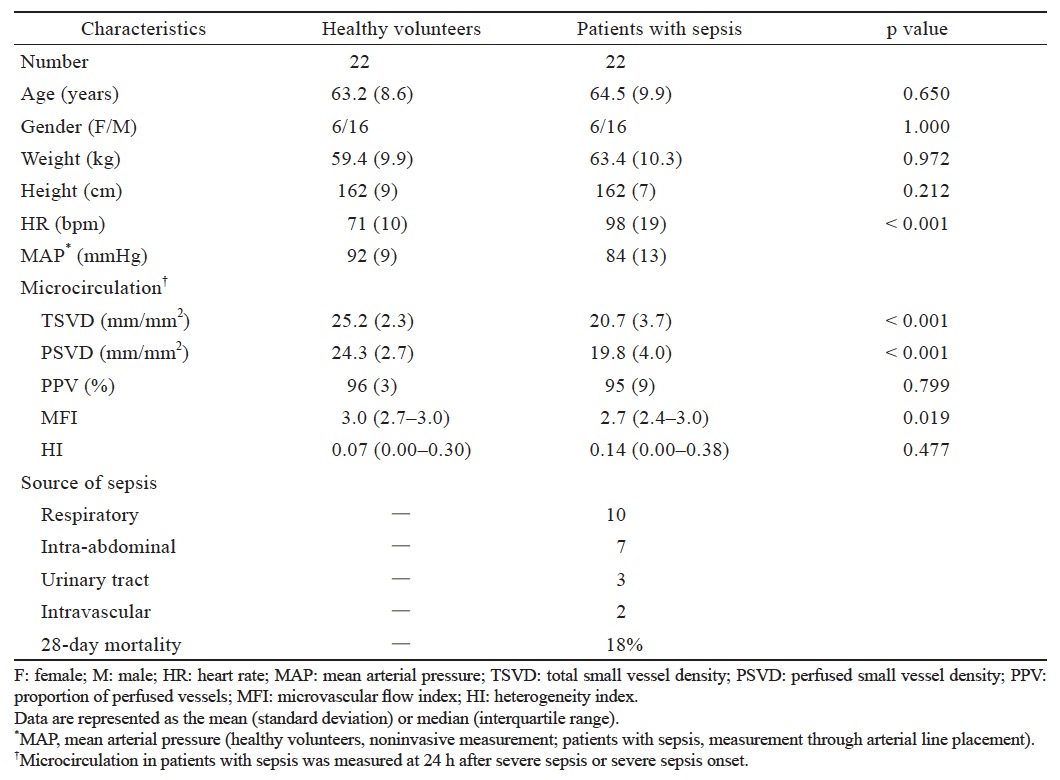
Matched Comparison Between Healthy Volunteers and Patients with Sepsis
Table 5 presents the baseline characteristics and microcirculatory parameters of matched pairs of healthy volunteers and patients with sepsis. The patients with sepsis had a 28-day mortality rate of 18%. TSVD, PSVD, and MFI scores were lower in the patients with sepsis than in the healthy volunteers. However, PPV and HI did note differ significantly between the health volunteers and patients with sepsis.
Download full-size image
4.Discussion
The present study demonstrated that age, sex, and BMI were correlated with the microcirculatory parameters in the healthy volunteers. In the patients with sepsis, macrocirculatory parameters did not differ significantly between the 28-day nonsurvivor and survivor group; however, microcirculatory dysfunction was more severe in the 28-day nonsurvivor group than in the 28-day survivor group. Moreover, matched comparison revealed that TSVD and PSVD was 18% and 19% lower, respectively, in the patients with sepsis than in the healthy volunteers.
Many experimental studies have reported that sublingual microcirculation and age are related;9-11 however, conflicting results have been observed. A study revealed that MFI scores are significantly lower in the 70–90 year age group and suggested that sublingual microcirculation changes significantly during aging.9 Reynolds et al.10 reported that increasing age does not affect sublingual microvascular flow. However, they compared healthy volunteers aged < 25 years with those aged> 55 years. Furthermore, the > 55-year age group was relatively younger than the elderly group in our study. Another study revealed that aging does not affect sublingual microcirculation;11 however, that study included patients with hypertension and diabetes mellitus, which are considered confounding factors. Endothelial function was reported to be progressively impaired with aging because of primary dysfunction in the NO system and subsequent oxidative stress, which cause age-related reduction in endothelium-dependent vasodilation.12,13 Microcirculation could be altered by impairment of endothelium- dependent vasodilation of human vessels. The finding that endothelial function is progressively impaired with aging is consistent with other studies.14,15
In our study, TSVD was higher and the PPV was lower in female participants than in male participant likely because the lower baseline blood pressure in women than in men. The finding is similar to that of a previous study,16 which demonstrated that optic nerve vessel microcirculation were higher in healthy female participants through laser speckle flowgraphy. Scardina et al.17 reported that oral microcirculation patterns are correlated with sex; microvascular loop density and length are higher in women than in men. In addition, BMI and TSVD exhibited a significant negative correlation in our study, but BMI is not an independent factor associated with microcirculation in multivariate regression analysis. Obesity, without any coexisting cardiovascular diseases, is associated with impaired vasomotor function.18 Obesity could lead to microvascular endothelium dysfunction by inducing enhanced reactive oxygen production and reducing NO-mediated arteriolar dilation.18-20 Other microcirculatory parameters were not correlated potentially because participants with a BMI > 27 were excluded.
In the patient with sepsis, the 28-day nonsurvivor group had lower TSVD, PSVD, and MFI scores than the 28-day survivor group. Nonsurvivors have been reported to exhibit more severe microcirculation alterations than survivors.6,21,22 De Backer et al.6 reported similar microcirculation alterations. Another study reported that compared with survivors, nonsurvivors exhibit a decreased PSVD, PPV, and MFI scores along with an increased HI.22 Furthermore, microcirculation improvement between sepsis day 1 and sepsis day 2 could be prognostic for survival.21 In summary, microcirculation parameters could be associated with sepsis severity.
Our matched comparison revealed that TSVD, PSVD, and MFI scores were significantly reduced in the patients with sepsis than in the healthy volunteers; however, the PPV and HI did not differ significantly between these two groups. The finding that patients with sepsis have decreased TSVD and PSVD is consistent with the study of De Backer et al.3 However, two previous studies have reported that PPV and HI were worse than in the sepsis group than in the healthy group.5,22 This discrepancy among studies has three possible explanations. First, age and sex were not controlled in the previous studies.5,22 Second, we excluded 10 patients with sepsis who could not be matched because of a very old age (> 80 years). Our result merely revealed that aging is correlated with microcirculatory parameters. Third, the time point of microcirculatory parameter measurements in the sepsis group were different. In the previous studies, the time points were within 6-h of presentation5 and during the first 24-h after admission to an ICU.22 However, in our study, microcirculation was measured at 24-h after severe sepsis or sepsis shock onset.
The present study has three major limitations. First, elderly people with hypertension were excluded. The microvascular condition and endothelial function of healthy elderly are satisfactory. However, the microcirculatory change in elderly people with hypertension could be more obvious than in healthy elderly people. Second, microcirculation in the patients with sepsis were measured at 24-h after severe sepsis or septic shock onset. Therefore, the time course of microcirculation changes and the effects of septic shock resuscitation including fluid resuscitation or blood transfusion, inotropic use, and dose of vasopressors were not investigated. Further studies are warranted to investigate the effects of these influencing factors on microcirculation. Third, the sample size after matching was relatively small. Therefore, the statistical power may have been insufficient to identify minor differences in the microcirculatory parameters of the patients with sepsis and healthy volunteers.
In conclusion, our study provides normal ranges of microcirculatory parameters in healthy volunteers, which could facilitate further investigation on the clinical application of microcirculation resuscitation in septic patients. Furthermore, age, sex, and BMI are correlated with microcirculatory parameters. In patients with sepsis, we confirmed that microcirculatory dysfunction is more severe in 28-day nonsurvivors than in 28-day survivors in Taiwan. Finally, TSVD, PSVD, and MFI scores are lower in patients with sepsis than in healthy volunteers.
References
| 1 |
Vincent JL.
Microvascular endothelial dysfunction: a renewed appreciation of sepsis pathophysiology.
Crit Care 2001;5(Suppl 2):S1–S5.
|
| 2 |
Hack CE, Zeerleder S.
The endothelium in sepsis: source of and a target for inflammation.
Crit Care Med 2001;29(7 Suppl):S21–S27.
|
| 3 |
De Backer D, Creteur J, Preiser JC, Dubois MJ, Vincent JL.
Microvascular blood flow is altered in patients with sepsis.
Am J Respir Crit Care Med 2002;166:98–104.
|
| 4 |
Vincent JL, De Backer D.
Microvascular dysfunction as a cause of organ dysfunction in severe sepsis.
Crit Care 2005;9(Suppl 4):S9–S12.
|
| 5 |
Spanos A, Jhanji S, Vivian-Smith A, Harris T, Pearse RM.
Early microvascular changes in sepsis and severe sepsis.
Shock 2010;33:387–391.
|
| 6 |
De Backer D, Donadello K, Sakr Y, et al.
Microcirculatory alterations in patients with severe sepsis: impact of time of assessment and relationship with outcome.
Crit Care Med 2013;41:791–799.
|
| 7 |
Nencioni A, Trzeciak S, Shapiro NI.
The microcirculation as a diagnostic and therapeutic target in sepsis.
Intern Emerg Med 2009;4:413–418.
|
| 8 |
Yeh YC, Wang MJ, Chao A, et al.
Correlation between early sublingual small vessel density and late blood lactate level in critically ill surgical patients.
J Surg Res 2013;180:317–321.
|
| 9 |
Abdo IS, Turek Z, Parizkova R, Cerny V.
Imaging of the sublingual microcirculation in elderly patients—a pilot study.
Appl Cardiopulm Pathophysiol 2012;16:276–282.
|
| 10 |
Reynolds T, Vivian-Smith A, Jhanji S, Pearse RM.
Observational study of the effects of age, diabetes mellitus, cirrhosis and chronic kidney disease on sublingual microvascular flow.
Perioper Med (Lond) 2013;2:7.
|
| 11 |
Kanoore Edul VS, Ince C, Estenssoro E, et al.
The effects of arterial hypertension and age on the sublingual microcirculation of healthy volunteers and outpatients with cardiovascular risk factors.
Microcirculation 2015;22:485–492.
|
| 12 |
Taddei S, Virdis A, Ghiadoni L, et al.
Age-related reduction of NO availability and oxidative stress in humans.
Hypertension 2001;38:274–279.
|
| 13 |
Higashi Y, Kihara Y, Noma K.
Endothelial dysfunction and hypertension in aging.
Hypertens Res 2012;35:1039– 1047.
|
| 14 |
Bentov I, Reed MJ.
The effect of aging on the cutaneous microvasculature.
Microvasc Res 2015;100:25–31.
|
| 15 |
Muller-Delp JM.
Aging-induced adaptations of microvascular reactivity.
Microcirculation 2006;13:301–314.
|
| 16 |
Aizawa N, Kunikata H, Nitta F, et al.
Age- and sex-dependency of laser speckle flowgraphy measurements of optic nerve vessel microcirculation.
PLoS One 2016;11:e0148812.
|
| 17 |
Scardina GA, Cacioppo A, Messina P.
Anatomical evaluation of oral microcirculation: capillary characteristics associated with sex or age group.
Ann Anat 2009;191:371–378.
|
| 18 |
Stepp DW.
Impact of obesity and insulin resistance on vasomotor tone: nitric oxide and beyond.
Clin Exp Pharmacol Physiol 2006;33:407–414.
|
| 19 |
Nernpermpisooth N, Qiu S, Mintz JD, et al.
Obesity alters the peripheral circadian clock in the aorta and microcirculation.
Microcirculation 2015;22:257–266.
|
| 20 |
Bagi Z, Feher A, Cassuto J.
Microvascular responsiveness in obesity: implications for therapeutic intervention.
Br J Pharmacol 2012;165:544–560.
|
| 21 |
Top AP, Ince C, de Meij N, van Dijk M, Tibboel D.
Persistent low microcirculatory vessel density in nonsurvivors of sepsis in pediatric intensive care.
Crit Care Med 2011;39:8–13.
|
| 22 |
Edul VS, Enrico C, Laviolle B, Vazquez AR, Ince C, Dubin A.
Quantitative assessment of the microcirculation in healthy volunteers and in patients with septic shock.
Crit Care Med 2012;40:1443–1448.
|