Abstract
Introduction
The impact of preoperative glycated haemoglobin (HbA1c) in patients undergoing gastrointestinal and hepatobiliary surgery is unclear as data is limited.
Methods
Patients undergoing gastrointestinal surgery attending pre-assessment screening (PAS) clinics from August to September 2016 at the Queen Elizabeth Hospital Birmingham (QEHB) were identifi ed. Outcome measure was postoperative complications as defi ned by the Clavien-Dindo classifi cation system.
Results
In this study, 381 patients were included, of which 48% (181/381) had HbA1c measured. Of these, 27% (49/181) had a HbA1c ≥ 48 mmol/mol. Overall complications were 14% and major complication rates were 3% (11/381). In unadjusted models, patients with HbA1c ≥ 48 mmol/mol had signifi cantly higher rates of overall complications (odds ratio [OR] = 2.82, 95% confi dence interval [CI] = 1.22–6.49; p = 0.015). In adjusted models, only surgical grade was predictive of overall complications. In patients undergoing major surgery (n = 93), there were signifi cantly higher rates of overall complications in patients with HbA1c ≥ 48 mmol/mol as compared to those with HbA1c < 48 mmol/mol (63% vs. 46%, p=0.043).
Conclusion
Utility of HbA1c to stratify patients undergoing gastrointestinal and hepatobiliary surgery into high-risk clinics is limited from this study. Future studies should aim to validate these fi ndings in much larger cohorts.
Keywords
HbA1c ; outcomes ; surgery ; post-op complications ;
Introduction
Glycated haemoglobin (HbA1c) is formed when the oxygen-carrying pigment, HbA1c combines irreversibly with glucose in blood. HbA1c is commonly used as a marker to monitor long term glycaemic control in patients with type 1 (T1DM) and 2 diabetes mellitus (T2DM).1,2 A recent report published by the Association of Anaesthetists of Great Britain and Ireland (AAGBI) highlighted that 10–15% of surgical patients are diabetic and are reported to have greater mortality rates, complication rates and length of hospital stay.3 The importance of optimum glycaemic control was also emphasized by the 2011 National Health Service (NHS) Diabetes Guideline which recommended elective surgeries to be postponed if HbA1c ≥ 69 mmol/mol.4
Recently, there has been much interest in using HbA1c as a marker of glycaemic control to guide perioperative care of patients undergoing surgery, in diabetic and patients. Blankush et al. evaluating impact of preoperative HbA1c on postoperative infections across multiple specialties and concluded that the risk factors of postoperative infections are multiple and likely to be synergistic.5 In addition, a prospective cohort study including 120 patients who underwent major colorectal surgeries found that postoperative complications were more prevalent in patients with higher HbA1c level.6 A recent systematic review demonstrated inconclusive association between increased preoperative HbA1c with increased rates of postoperative morbidity or mortality in patients with T2DM.7 Nevertheless, the results obtained from this review were mainly based on patients undergoing orthopaedic, cardiac, and general surgeries with minimal inclusion of gastrointestinal and hepatobiliary surgery.
To date, data on the impact of HbA1c in patients undergoing gastrointestinal and hepatobiliary surgery is limited. As such, usefulness of HbA1c measurements during pre-assessment is unclear. Due to the heterogeneity of the systematic review and limited body of evidence available, this study sought to explore the relationship between the level of preoperative HbA1c with postoperative complications in patients undergoing hepatobiliary and gastrointestinal surgery.
Methods
This prospective study identified consecutive adult (≥ 18 years) patients attending pre-assessment screening (PAS) clinics for gastrointestinal and hepatobiliary surgeries between August 2016 and September 2016 at the Queen Elizabeth Hospital Birmingham (QEHB). Eligible procedures were those involving surgery on any part of the gastrointestinal tract or biliary tree, involving a hospital admission with an overnight stay. Patients undergoing day-case urological, gynaecological, vascular, or transplant procedures were excluded. This study was registered and approved by the local audit department. Patients’ medical records were reviewed and the data were extracted on to a uniform database (Microsoft® Excel 2010, Microsoft Corp., Redmond, WA, USA) that was designed to include all relevant details pertinent to this study.
Pre-Assessment
Clinics At QEHB, all patients undergoing surgical procedures are referred by the surgeon to dedicated pre-assessment clinics according to surgery grade and comorbidities. Clinics are divided into low risk and high risk; numerically these correspond to levels 1 and 2A and 2B and 3. Low risk clinics are led and delivered by trained pre-assessment nurses whereas high risk clinics are led and delivered by more experienced nursing staff and consultant anaesthetists. Currently, there is no systematic way of allocating patients into these clinics as patients are risk-assessed individually by the surgeons.
Explanatory Variable
The main variable of interest was preoperative HbA1c. Since it is not standard practice to measure HbA1c for all patients at pre-assessments, values were taken based on measurements from PAS clinics or any available measurement within 3 months of surgery. In cases, where HbA1c were not available, these patients were recorded as “Not Done.” Patients were categorised into two main groups, those with HbA1C < 48 mmol/mol or HbA1C ≥ 48 mmol/mol. This cutoff point was chosen as previous studies have used similar cut-offs although no standard consensus currently exists in the literature.5-8
Outcome Measures
The primary outcome measure was 30-day complications as defined by the Clavien-Dindo classification system.9 Secondary outcome measures were major complications, 30-day readmission rates and postoperative care setting.
Statistical Analysis
Baseline characteristics were compared between groups using Pearson chi-square (χ2) test for categorical variables and Mann-Whitney U test for continuous variables. Multivariate logistic regression was used to determine the strength association between risk factors for postoperative complications. Models built included age, sex, ethnicity, grade of surgery, presence of specific co-morbid diseases, surgical specialty and surgical approach. Results are presented as odds ratios (ORs) with 95% confidence interval (CI). In all analyses, a p-value of < 0.05 were maintained as statistically significant. Data analysis was performed using R Foundation Statistical software (R 3.2.1) with TableOne and Hmisc packages (R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline Demographics
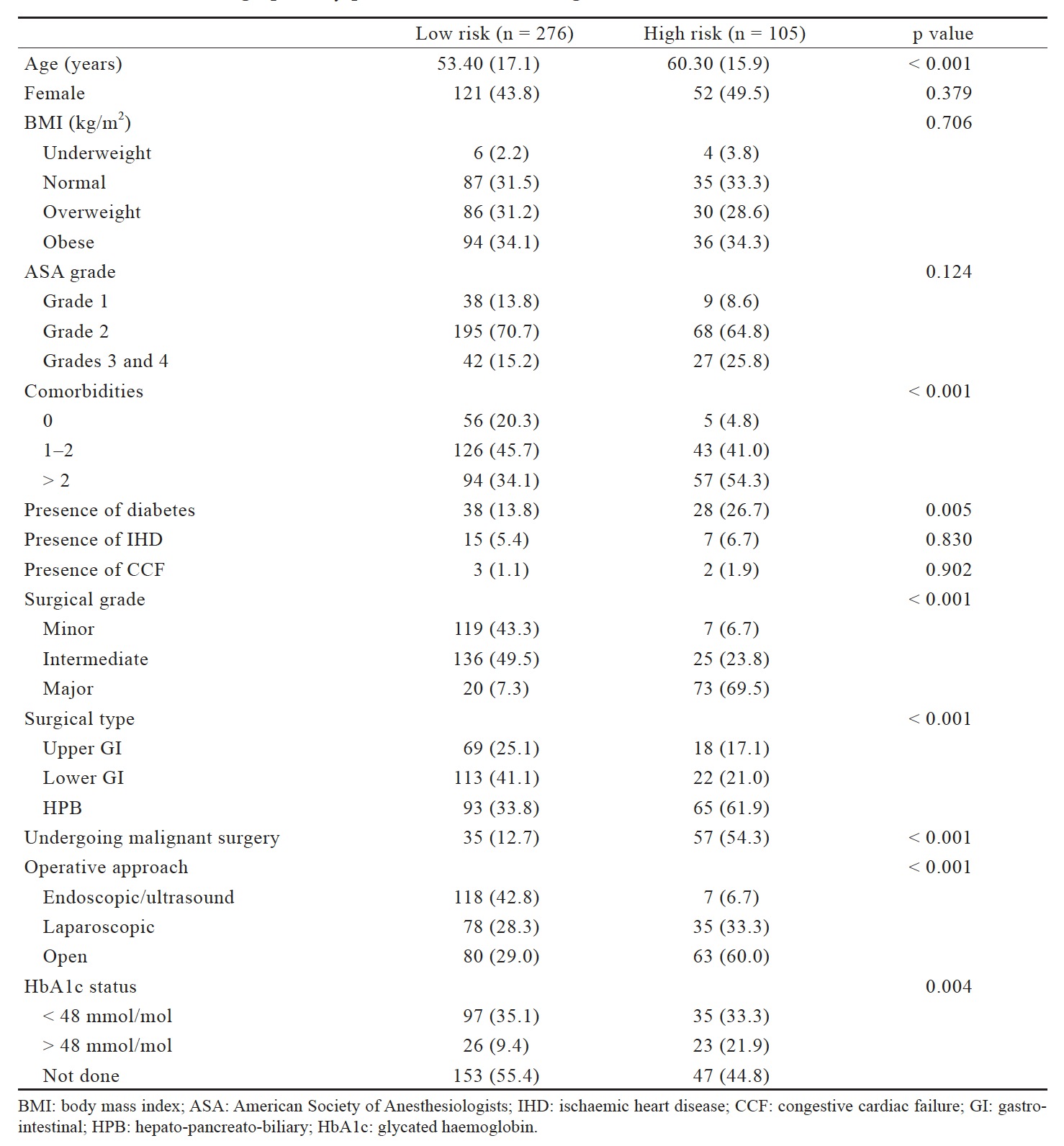
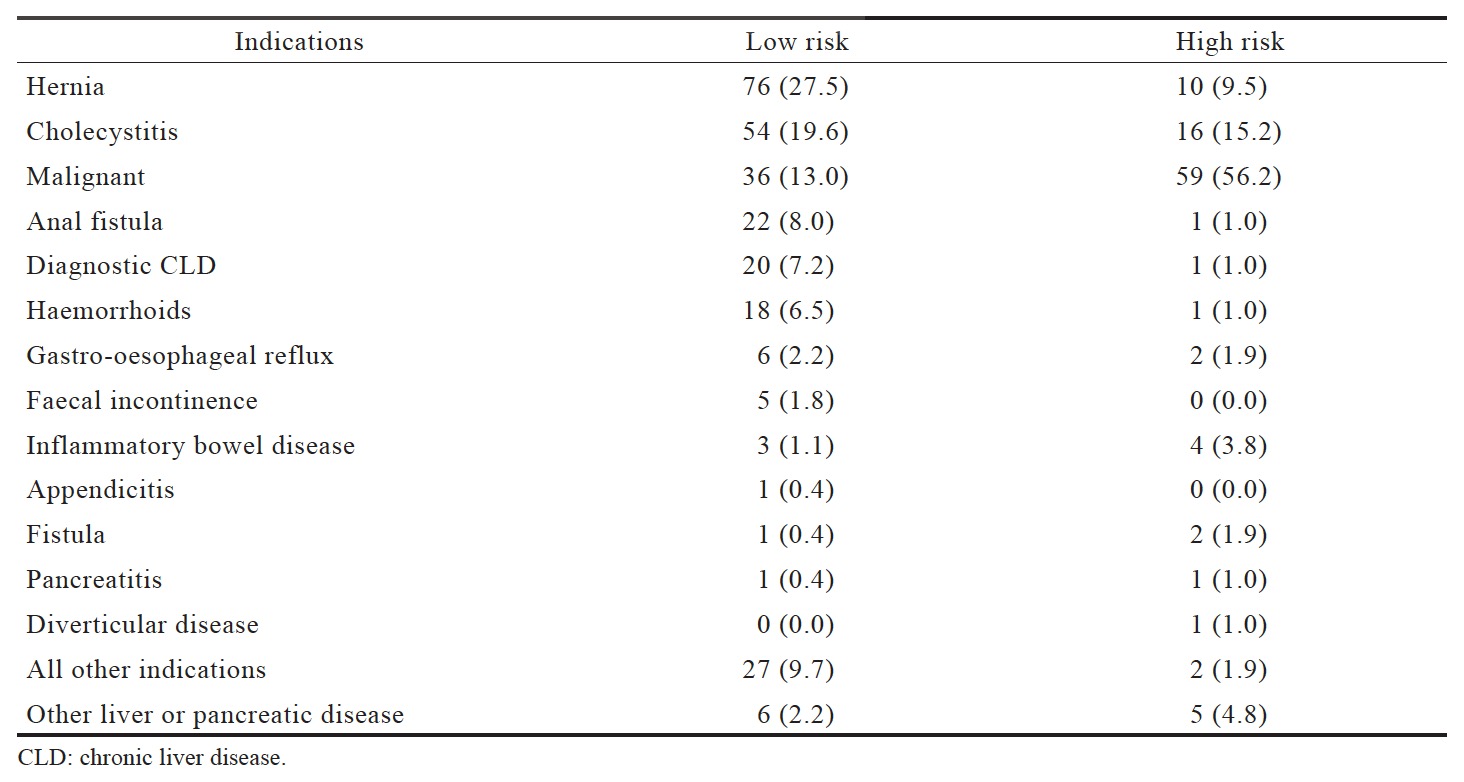
This study identified 381 patients attending PAS clinics, of which 72% were seen in low-risk clinics (276/381) whereas 28% in high risk clinics (105/381). The baseline demographics of patients seen in these clinics are presented in Table 1. Patients seen in high risk clinics were significantly older (p < 0.001), have> 2 comorbidities (p < 0.001), and were more likely to undergo major surgeries. In this cohort, 54% of patients in the high-risk clinics were undergoing surgery for malignant indication as compared to 13% in the low risk clinic (p < 0.001). Surgical indications between the low-risk and high-risk pre-assessment clinics are presented in Table 2.
Download full-size image
Download full-size image
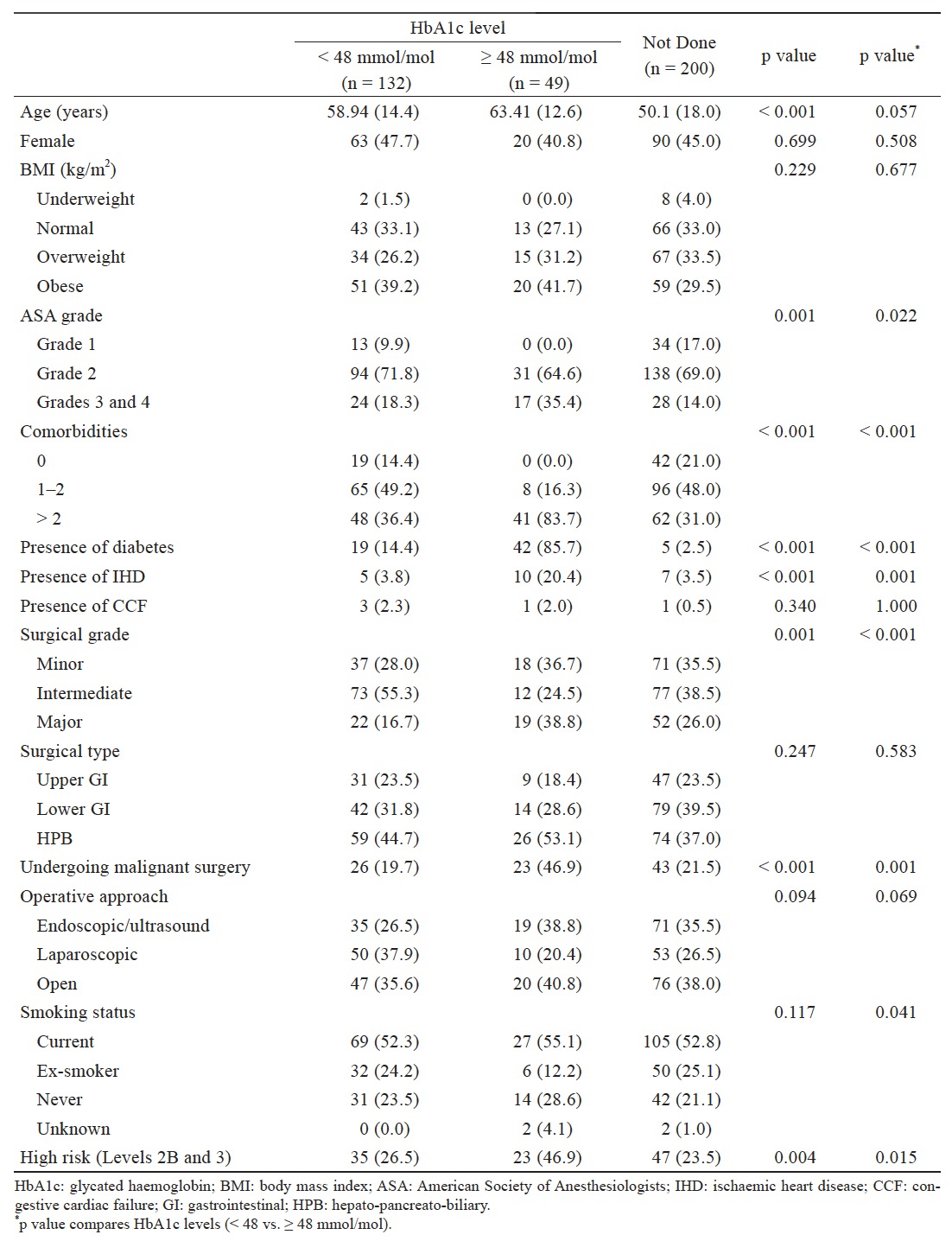
There were significantly higher rates of patients with T2DM in the high-risk clinics as compared to the low risk clinics (27% vs. 14%, p = 0.005). HbA1c was only performed in 48% (181/381) of patients during pre-assessment clinics. Only 34% (61/181) of these patients had T2DM. In patients that did not have HbA1c (n = 200), 3% (5/200) had T2DM. Patients seen in the high-risk clinics were more likely to have HbA1c > 48 mmol/mol as compared to those in the low risk clinics (22% vs. 9%, p = 0.004). Baseline demographics of patients with HbA1c ≥ 48 vs. < 48 mmol/mol are presented in Table 3. Patients with HbA1c ≥ 48 mmol/mol had significantly higher number of comorbidities, major surgeries and American Society of Anesthesiologists (ASA) grades 3 and 4.
Download full-size image
Postoperative Outcomes
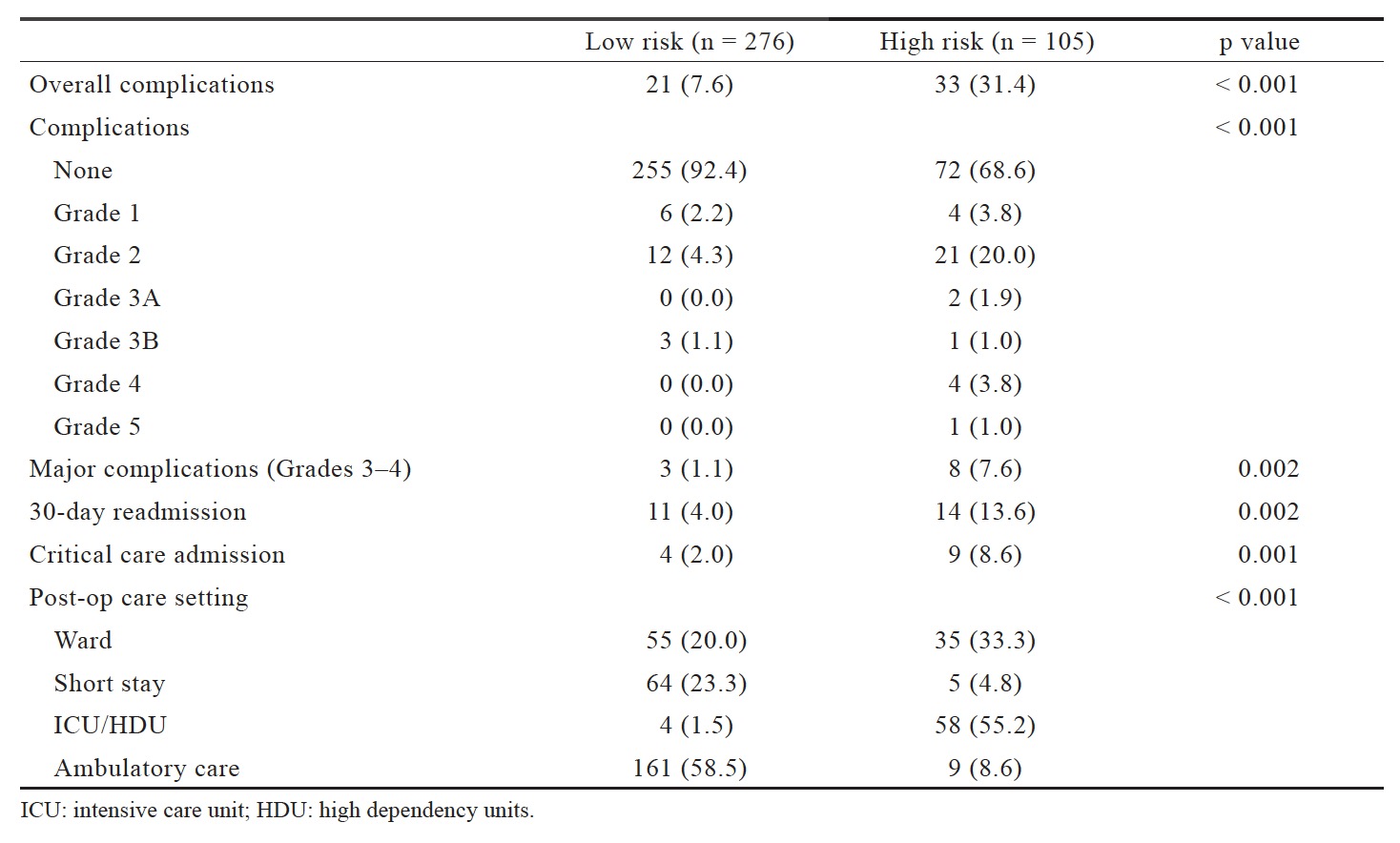
The postoperative outcomes are presented in Table 4. In the unmatched cohort, 14% developed complications, of which 31% were from high risk clinics as compared to 8% from the low risk clinic (p < 0.001). Patients seen in the high-risk clinics had significantly higher rates of major complications (Grades 3–5) than patients from low risk clinics (8% vs. 1%, p=0.002). Rates of readmission to hospital within 30- day were significantly higher in patients seen in highrisk clinics (14% vs. 4%, p=0.002).
Download full-size image
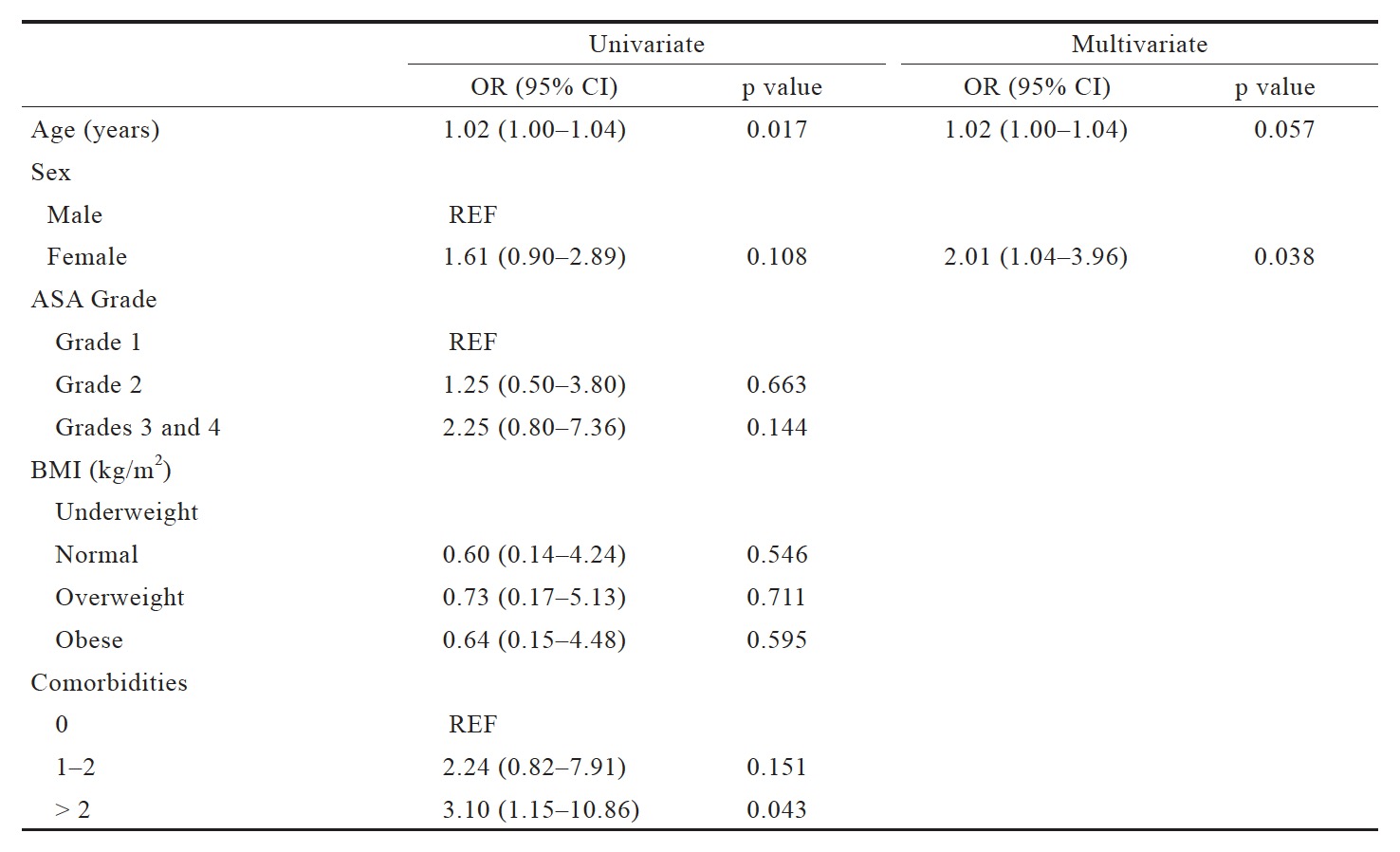
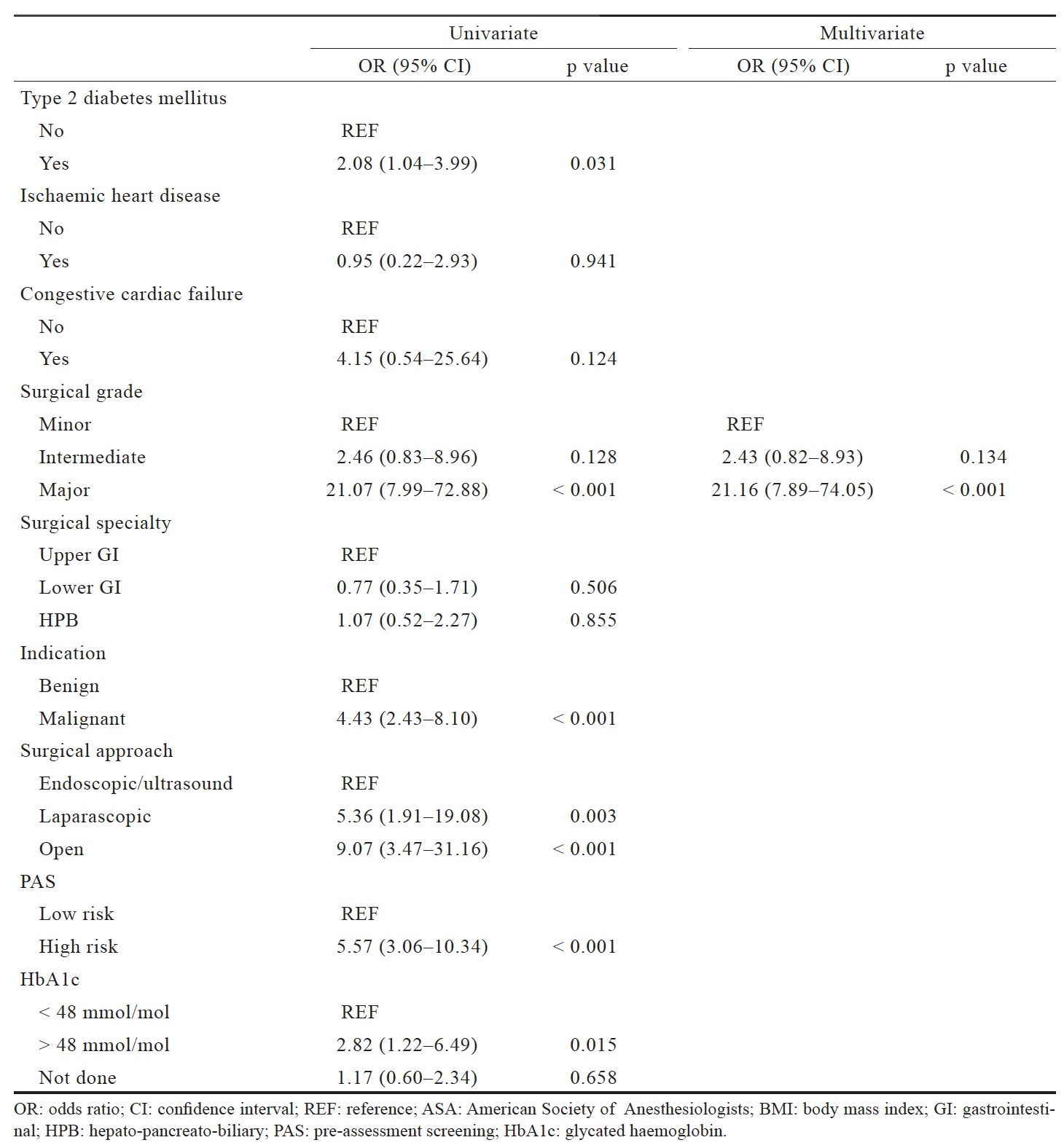
Factors Predicting Postoperative Complications
Univariate and multivariate regression were carried out to identify factors predictive of overall complications in the matched cohort (Table 5). Patients with hyperglycaemia (HbA1c > 48 mmol/mol) were significantly at increased risk of overall complications (OR = 2.82, 95% CI = 1.22–6.49; p = 0.015). Major surgical grade (OR = 21.07, 95% CI = 7.99–72.88; p < 0.001) and patients undergoing surgery for malignancy (OR=4.43, 95% CI=2.43–8.10; p < 0.001) were also significantly at increased risk of postoperative complications. In adjusted models, hyperglycaemia was not predictive of overall complications in this cohort.
Download full-size image
Download full-size image
Impact of HbA1c in Patients With T2DM
Subgroup analysis were carried out in the 66 patients with T2DM of which, 29% (19/66) had HbA1c < 48 mmol/mol, 64% (42/66) had HbA1c ≥ 48 mmol/ mol and 7% (5/66) did not HbA1c tests. There were no significant differences in patient characteristics between these groups. Although rates of overall complications in patients with HbA1c ≥ 48 mmol/mol were higher than patients with HbA1c levels < 48 mmol/ mol and those not tested, this was not significant (26% vs. 16% vs. 20%, p=0.661). Similarly, there were no significant differences in the rates of major complications (7% vs. 5% vs. 0%, p=0.806), 30-day readmission (7% vs. 6% vs. 0%, p=0.815) and unplanned critical care admissions (10% vs. 0% vs. 0%, p=0.296) between patients with HbA1c ≥ 48 mmol/ mol, < 48 mmol/mol, and those that were not tested.
Impact of HbA1c in Patients Undergoing Major Surgery
In this cohort, 93 patients underwent major gastrointestinal and hepatobiliary surgeries. Of these patients, 20% (19/93) had HbA1c < 48 mmol/mol, 24% (22/93) had HbA1c ≥ 48 mmol/mol and 56% (52/93) did not have a HbA1c test. Patients with HbA1c ≥ 48 mmol/mol were significantly older, higher ASA grade and have> 2 comorbidities. Patients with HbA1c ≥ 48 mmol/mol had significantly higher rates of T2DM than patients with HbA1c < 48 mmol/mol (84% vs. 18%). Overall complication rates were significantly higher in patients with HbA1c ≥ 48 mmol/mol as compared to those with HbA1c < 48 mmol/mol (63% vs. 46%, p=0.043). Rates of overall complications in patients that did not have HbA1c tested were 31% (16/52). However, there was no significant difference in major complications, 30-day readmission and critical care admissions. In T2DM patients undergoing major surgery (n=20), there were no significant difference in rates of overall complications between patients with HbA1c ≥ 48 mmol/mol and < 48 mmol/ mol (63% vs. 25%, p=0.432).
Discussion
This study aimed at investigating the relationship between preoperative HbA1c with postoperative complications. Our study demonstrated that patients with HbA1c ≥ 48 mmol/mol have significantly higher risk of overall complications, but not in adjusted multivariate models. In patients undergoing major surgeries, rates of overall complications were also significantly higher in patients with HbA1c ≥ 48 mmol/mol. Subgroup analysis of T2DM patients, undergoing all surgeries as well major surgeries only, did not show significant differences in rates of overall complications between the two groups respectively.
Currently, there are conflicting and inconclusive evidence regarding the association between preoperative HbA1c with postoperative complications across different surgical specialties. A large cohort study involving 10,232 patients demonstrated a positive correlation between HbA1c levels and incidence of cardiovascular events in diabetics and non-diabetic patients.10 Suboptimal HbA1c levels were identified as a significant risk factor of overall 30-day morbidity rate in patients undergoing vascular surgery.1 These results are further supported by a study assessing major adverse cardiac events after percutaneous coronary intervention (PCI).11 However, as these studies evaluated outcomes in patients undergoing cardiovascular surgery, the results might not be comparable to patients undergoing hepatobiliary and gastrointestinal surgery.
To date, impact of HbA1c in patients undergoing gastrointestinal and hepatobiliary surgery is unclear. A retrospective review of patients with gastrointestinal cancer and T2DM concluded that an elevated level of HbA1c has a positive correlation and was an independent predictor of short term adverse outcomes.12 Gustafsson et al. also reported significantly higher rates of postoperative complications in patients with high HbA1c level following major colorectal surgery.6 In contrary, a retrospective study involving patients undergoing gastric bypass surgery concluded no increased risk of complications in patients with elevated levels of HbA1c.13 Furthermore, a systematic review also showed that elevated preoperative HbA1c level was not associated with increased morbidity or mortality rates in patients with diabetes mellitus, of which 2 studies included in this review were for non-cardiac surgeries.7
Despite having guidelines on the perioperative management of adult patients diagnosed with diabetes, there are currently no recommendations on the management of patients with unknown diabetes status with elevated levels of HbA1c.4 In a prospective observational cohort study by Wexler et al. nearly one in five patients of hospitalised patients had elevated levels of HbA1c without a diagnosis of diabetes.14 At QEHB, a two-tier system of risk assessment was recently introduced to classify patients into different risk groups according to their ASA and comorbidities. The preoperative assessment was mainly conducted based on clinical judgement of surgeons, anaesthetists, and specialist nurses guided by previously diagnosed conditions. Therefore, there is no systematic way being implemented to classify patients into different risk groups based according to their HbA1c levels.
One of the limitations of this study was that it is a single-institution study of which the results will require validation from other centres with a similar approach of pre-assessment of surgical patients. Secondly, there were small numbers of patients in the subgroup analysis of T2DM undergoing major surgery, limiting our ability to establish if there is an impact of elevated HbA1c on postoperative complications. Lastly, the measurement of HbA1c was not routinely done in PAS clinics. Therefore, alternative HbA1c value from most recent data available within 3 months of PAS had to be taken. Nevertheless, despite these limitations, this study adds into the limited body of evidence available to investigate the impacts of elevated HbA1c levels in patients undergoing hepatobiliary and gastrointestinal surgery.
Conclusion
Utility of HbA1c to stratify patients undergoing gastrointestinal and hepatobiliary surgery into highrisk clinics is limited from this study. Patients undergoing major surgery with HbA1c > 48 mmol/mol appear to have higher rates of overall complications. Therefore, HbA1c status in these patients would allow risk stratification prior to surgery. To move forwards, future studies should aim to validate these findings in much larger cohorts and enable a clear consensus supporting the need for preoperative HbA1c measurement needs to be established.
Conflicts of Interest
None of the authors have any conflicts of interest to declare. Funding No funding was received for any part of this study.
References
| 1 |
O’Sullivan CJ, Hynes N, Mahendran B, et al.
Haemoglobin A1c (HbA1C) in non-diabetic and diabetic vascular patients.
Is HbA1C an independent risk factor and predictor of adverse outcome? Eur J Vasc Endovasc Surg 2006;32:188–197.
|
| 2 |
Haller MJ, Stalvey MS, Silverstein JH.
Predictors of control of diabetes: monitoring may be the key.
J Pediatr 2004;144:660–661.
|
| 3 |
Barker P, Creasey PE, Dhatariya K, et al.
Peri-operative management of the surgical patient with diabetes 2015: Association of Anaesthetists of Great Britain and Ireland.
Anaesthesia 2015;70:1427–1440.
|
| 4 |
Dhatariya K, Levy N, Kilvert A, et al.
NHS Diabetes guideline for the perioperative management of the adult patient with diabetes.
Diabet Med 2012;29:420–433.
|
| 5 |
Blankush JM, Leitman IM, Soleiman A, Tran T.
Association between elevated pre-operative glycosylated hemoglobin and post-operative infections after non-emergent surgery.
Ann Med Surg (Lond) 2016;10:77–82.
|
| 6 |
Gustafsson UO, Thorell A, Soop M, Ljungqvist O, Nygren J.
Haemoglobin A1c as a predictor of postoperative hyperglycaemia and complications after major colorectal surgery.
Br J Surg 2009;96:1358–1364.
|
| 7 |
Rollins KE, Varadhan KK, Dhatariya K, Lobo DN.
Systematic review of the impact of HbA1c on outcomes following surgery in patients with diabetes mellitus.
Clin Nutr 2016;35:308–316.
|
| 8 |
Goodenough CJ, Liang MK, Nguyen MT, et al.
Preoperative glycosylated hemoglobin and postoperative glucose together predict major complications after abdominal surgery.
J Am Coll Surg 2015;221:854–861.e1.
|
| 9 |
Clavien PA, Barkun J, de Oliveira ML, et al.
The Clavien-Dindo classification of surgical complications: five-year experience.
Ann Surg 2009;250:187–196.
|
| 10 |
Khaw KT, Wareham N, Bingham S, Luben R, Welch A, Day N.
Association of hemoglobin A1c with cardiovascular disease and mortality in adults: the European prospective investigation into cancer in Norfolk.
Ann Intern Med 2004;141:413–420.
|
| 11 |
Corpus RA, O’Neill WW, Dixon SR, Timmis GC, Devlin WH.
Relation of hemoglobin A1c to rate of major adverse cardiac events in nondiabetic patients undergoing percutaneous coronary revascularization.
Am J Cardiol 2003;92:1282–1286.
|
| 12 |
Huang Y, Zheng H, Chen P, et al.
An elevated HbA1c level is associated with short-term adverse outcomes in patients with gastrointestinal cancer and type 2 diabetes mellitus.
J Clin Med Res 2017;9:303–309.
|
| 13 |
Rawlins L, Rawlins MP, Brown CC, Schumacher DL.
Effect of elevated hemoglobin A1c in diabetic patients on complication rates after Roux-en-Y gastric bypass.
Surg Obes Relat Dis 2013;9:749–752.
|
| 14 |
Wexler DJ, Nathan DM, Grant RW, Regan S, Van Leuvan AL, Cagliero E.
Prevalence of elevated hemoglobin A1c among patients admitted to the hospital without a diagnosis of diabetes.
J Clin Endocrinol Metab 2008;93:4238–4244.
|