Abstract
Objective
Supraglottic airway devices (SGAs) have advantages in reducing respiration-associated complications. However, limited studies on the influence of head and neck rotation on the risk of air leakage have been conducted. We hypothesize that different head and neck rotation angles will increase the risk of air leakage when using SGAs.
Methods
A prospective, randomized study was conducted with 51 patients in the i-gelTM group and 50 patients in the AuraOnceTM group. The head and neck were subsequently rotated to the following positions: 0 (neutral), 15, 30, 45, and 60 degrees. Airway pressure over 20 cmH2O was defi ned as negative for air leakage.
Results
The percentage of air leakage was proportional to the increase in rotational degrees at the various rotation angles. The incidence of patients without air leakage at the largest angle (60 degrees) of head and neck rotation in both groups was approximately 80% (i-gelTM: 82.35%; AuraOnceTM: 79.59%).
Conclusion
SGAs presented acceptable performance with increased head and neck rotation angles.
Keywords
AuraOnceTM ; air leak ; head and neck rotation ; i-gelTM ; positive pressure ventilation ; supraglottic airway devices
Introduction
The use of a supraglottic airway device (SGA) under positive pressure ventilation was associated with a risk of air leakage, leading to insuffi cient ventilation in patients during surgery.1,2 Furthermore, airway maintenance during head and neck position changes when using a SGA remains a great challenge. Trachea tubes are usually favored over SGAs to avoid the risk of air leakage if head and neck rotation is necessary during surgery. Nevertheless, the trend of using SGAs to substitute endotracheal tubes has increased due to the lower invasiveness and fewer side effects of SGAs.3 Some new SGAs such as the cuffed Ambu® AuraOnceTM Laryngeal Mask (AuraOnceTM, Ambu A⁄S, Ballerup, Denmark) and the uncuffed i-gelTM airway (i-gelTM, Intersurgical Ltd., Wokingham, Berkshire, UK) have unique designs to provide more effective airway maintenance during controlled ventilation.4-7
However, limited studies have been conducted with respect to different head and neck rotation angles while using SGAs.8-12 To the best of our knowledge, no existing studies have addressed the effects of different head and neck rotation angles on air leakage during SGA use.
The objective of our study was to investigate the influence of different head and neck rotation angles on air leakage with SGAs in both anesthetized and paralyzed patients. We hypothesized that the risk of air leakage would increase with different head and neck rotation angles.
Methods
A total of 101 patients were analyzed in the current study after obtaining their written informed consent and Ethics Committee approval under No. 201306042RIND. The 101 patients with American Society of Anesthesiologists (ASA) physical statuses I and II, aged from 20 to 80 years old, were evaluated during elective orthopedic surgery in our study. The patients were excluded if they had limited head and neck movement or contraindications for the use of a SGA (e.g., limited mouth opening, morbid obesity, gastric reflux disease, or insufficient fasting time). Furthermore, each patient was confirmed to be capable of conducting different head and neck rotation angles without discomfort prior to joining the study. The AuraOnceTM and i-gelTM are classified as cuffed and uncuffed SGAs, respectively. These SGAs were used and randomly applied to the patients in the study.
Anesthesia was induced in patients with propofol (2.5 mg/kg) and fentanyl (2 μg/kg) followed by cisatracurium (0.1 mg/kg) administration. No nitrous oxide was applied throughout the whole anesthesia process.13 General anesthesia was maintained by sevoflurane.
All SGAs used in the study were inserted and adjusted by a well-trained anesthesiologist to achieve proper positioning. Airway pressure over 20 cmH2O was defined as negative for air leakage.14 A fiberscopic view was subsequently evaluated according to the various head and neck rotations. The intra-cuff pressure was subsequently adjusted to 60 cmH2O using a pocket cuff pressure gauge in the AuraOnceTM.
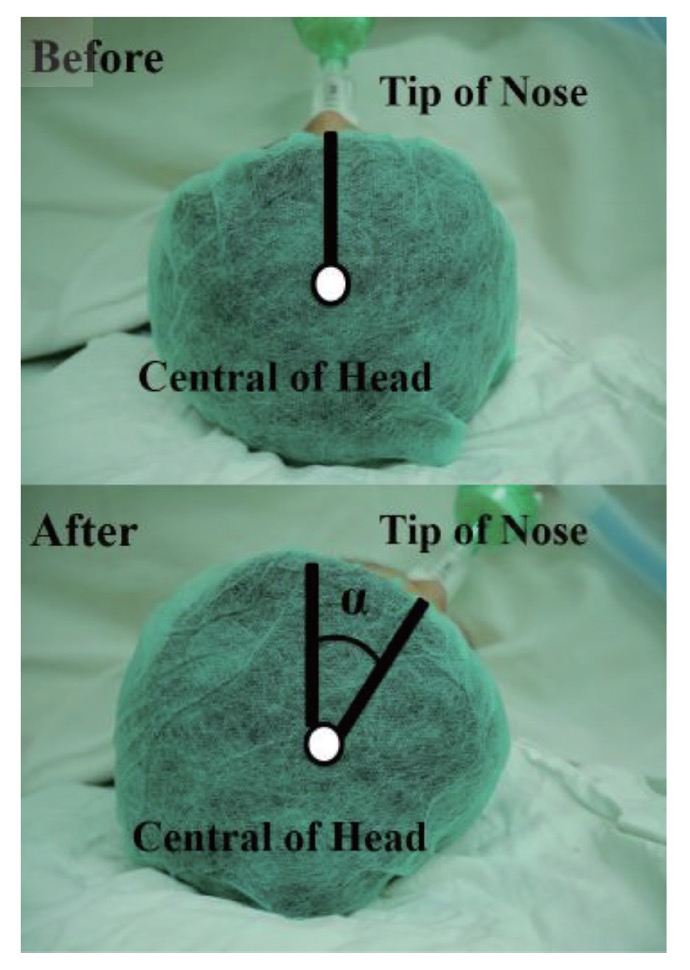
Each patient’s head and neck position was rotated through a series of different angles (0 [neutral], 15, 30, 45, and 60 degrees). The rotation angle was defined as the angle change relative to the axis between the center of the superior aspect of the head and the tip of the nose measured using a goniometer (Fig. 1).
Download full-size image
Air leakage was determined by closing the expiratory valve of the circular anesthetic breathing system at a fixed gas flow of 3 L/min after an airway pressure of 20 cmH2O was observed.8 Additionally, the justification of air leakage was identified according to the rotation angle regardless of the leakage area occurring in the SGA (right side, left side, or both). The occurrence of air leakage for different rotational positions using the cuffed or uncuffed SGA and the corresponding patient information such as age, weight, height, body mass index (BMI), and ASA physical status were documented.
We documented basic information for the 101 patients and calculated the percentage of patients with air leakage at different head and neck rotation angles (0 [neutral], 15, 30, 45, 60 degrees, respectively) with the use of the two SGAs. The calculated percentage of patients with air leakage was accordingly divided into the AuraOnceTM cohort and the i-gelTM cohort. Generalized estimation equation models were used to calculate the odds ratio of air leakage by dividing the odds ratio of each rotational angle with that of the neutral position as well as to compare the odds ratio of air leakage at the rotation angles of 15, 30, 45, and 60 degrees relative to that of 0 (neutral). The sample size of 101 patients reached a power value greater than 0.8 using G Power 3 software.15 A p value less than 0.05 was reported and was thus used to indicate statistical significance. Statistical tests were performed using SPSS 17.0 statistical software (SPSS Inc., Chicago, IL, USA).
Results
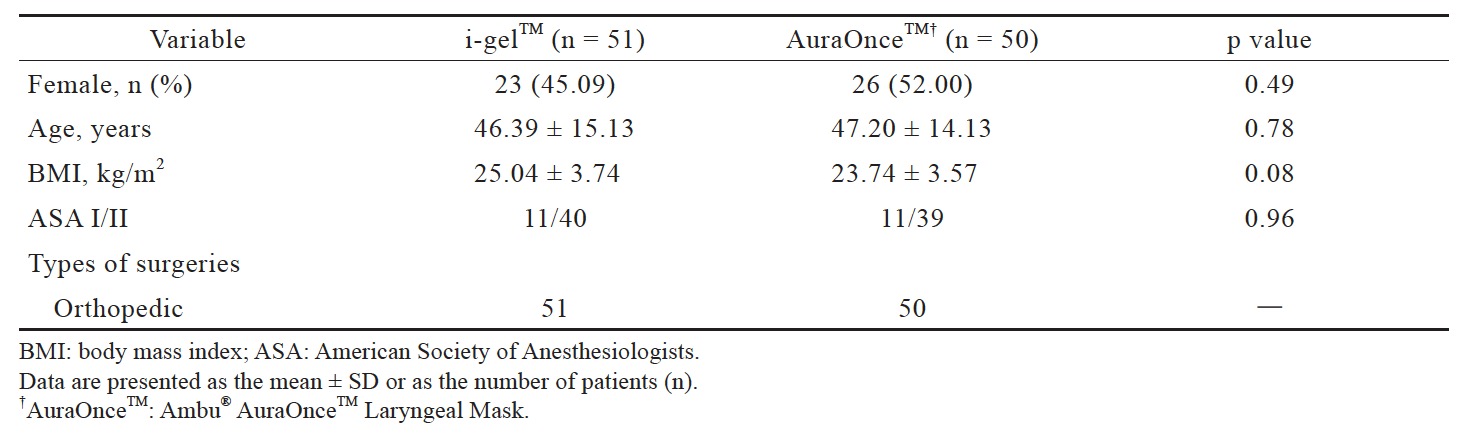
The patients’ descriptive data are shown in Table 1, and no significantly difference between the i-gelTM and the AuraOnceTM groups.
Download full-size image
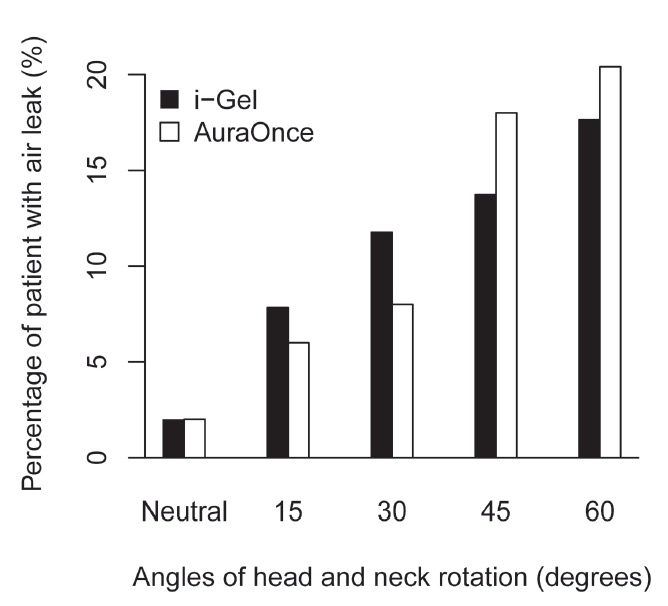
As shown in Fig. 2, the head and neck were rotated through different angles (0 [neutral], 15, 30, 45 and 60 degrees), and the percentage of patients with air leakage during i-gelTM or AuraOnceTM use was calculated by dividing the number of patients with air leakage by the total number of patients in the i-gelTM or AuraOnceTM group. In the i-gelTM group, 1.96% (1/51), 7.84% (4/51), 11.76% (6/51), 13.73% (7/51), and 17.65% (9/51) of patients had leakage at 0 (neutral), 15, 30, 45, and 60 degrees, respectively. In the AuraOnceTM group, 2% (1/50), 6% (3/50), 8% (4/50), 18% (9/50), and 20.41% (10/50) of patients had leakage at 0 (neutral), 15, 30, 45, and 60 degrees, respectively.
Download full-size image
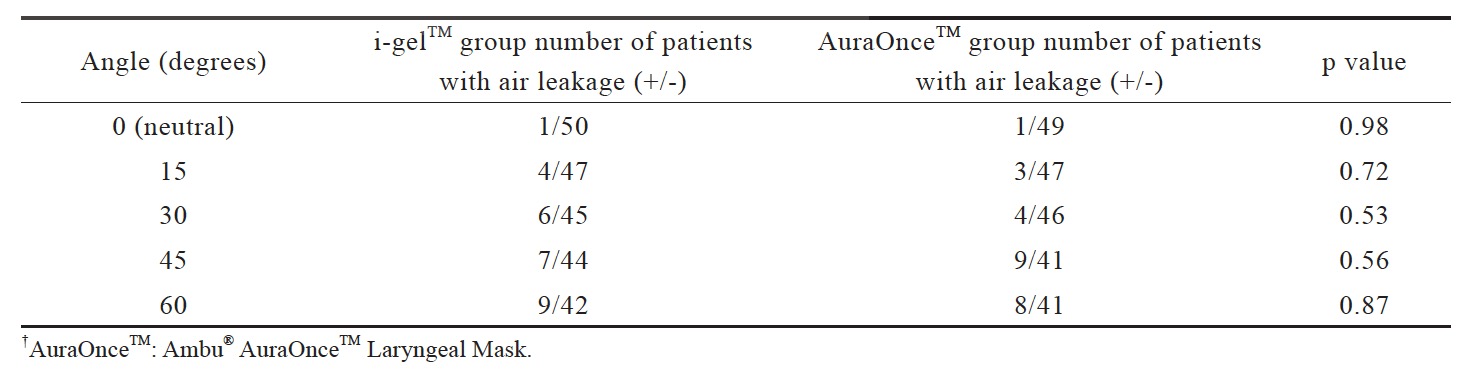
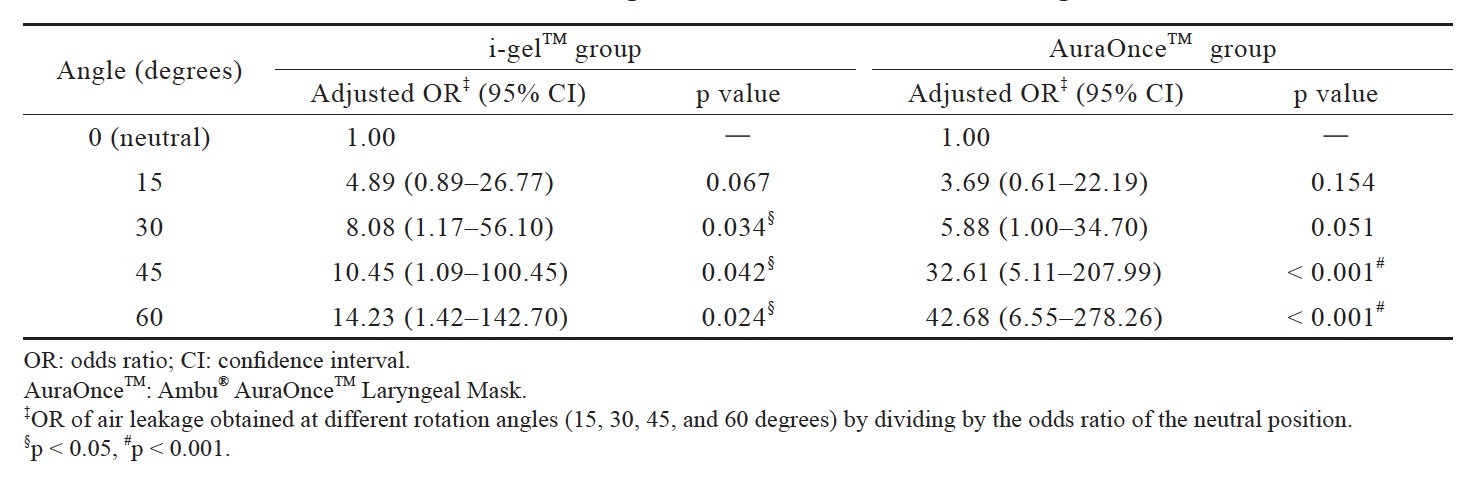
The number of air-leakage patients between the i-gelTM and AuraOnceTM groups showed no significance (Table 2). The odds ratio increased as the rotation angle increased in both groups. Additionally, in the i-gelTM group, the odds ratios of air leakage at the rotation angles of 30, 45, and 60 degrees were statistically significant relative to the neutral position. Compared with the neutral position, the odds ratios of air leakage in the AuraOnceTM group significantly increased at the rotation angles of 45 and 60 degrees. The tabulation data are shown in Table 3.
Download full-size image
Download full-size image
Discussion
The experimental results confirmed our hypothesis that head and neck rotation changes may lead cause the risk of air leakage with use of the i-gelTM and AuraOnceTM. However, the two SGAs preserved acceptable ventilation function performance even at the maximal rotation angle of 60 degrees.
Head and neck rotation is often required in many surgeries such as upper chest and upper extremity surgeries. We therefore chose rotation angles at 15-degree increments from 0 (neutral) to 60 degrees to observe the incidence of air leakage. A maximum rotation angle of 60 degrees has been defined to protect patients from cervical injury.16 Although conventional SGAs have been considered inapplicable for surgery requiring head and neck rotation,8 the two new SGAs used in this study allowed head and neck rotation with an acceptable air leakage risk.
The tolerance of the i-gelTM may be attributed to its unique three-dimensional structure that can adapt well to the perilaryngeal and hypopharyngeal spaces without the assistance of an inflatable cuff.6 In addition to its structural adaptability, a buccal cavity stabilizer can greatly reduce potential rotation within the oropharynx,17 and its robust structure is provided by the sturdy styrene ethylene butadiene styrene (SEBS) material.18
The AuraOnceTM was also observed to be compatible with rotation, likely due to the inherently flexible single-piece polyvinyl chloride AuraOnceTM mold, which provided improved shape deformation to adapt to the pharynx and larynx. Additionally, the slight curve between the cuff and the airway tube increases structural stability; this feature differs from other SGAs such as the LMA Classic or LMA Proseal.19,20 Thus, the material composition and structure of the AuraOnceTM are believed to increase stability when placed into pharynx and larynx as well as to increase resistance against breakage during head and neck rotation.21,22
Notably, although the incidence of air leakage began to show statistical significance at 30 and 45 degrees in the i-gelTM and AuraOnceTM groups, the incidence of air leakage was only approximately 20% at the maximal head and neck rotation of 60 degrees. This acceptable incidence may be due to the stable conformations of the SGAs, which maintain their function during head and neck rotation.
The study included some limitations. Our findings focused on the effects of various head and neck rotation angles on air leakage under 20 cmH2O airway pressure because we aimed to further investigate the risk factors of air leakage. First, more parameters should be taken into account, including changes in head and neck rotation angle under different parameters such as airway pressure levels, age or BMI groups, oropharyngeal leak pressures, intracuff pressures, and expiratory tidal volumes in the use of various SGAs. Second, the administration of a muscle relaxant to anesthetized patients may have affected their perilaryngeal muscle tone; thus, the risk of air leakage should be assessed without the use of neuromuscular blocking drugs.
Conclusions
In conclusion, SGAs showed decent ventilation function performance of an acceptable air leakage risk of approximately 20% at the largest rotation angle of 60 degrees. Therefore, SGAs may be applied during operations involving different angles of head and neck rotation.
Conflicts of Interest
No competing financial interests.
Author Contributions
Chih-Jun Lai participated in the collection and analysis of the data and in formulating the paper. Shou-Zen Fan and Yi-Chia Wang participated in the design of project and formulating the paper. Chih-Min Liu guided the design of project and participated in formulating the paper.
Acknowledgements
We thank all staff in the Department of Anesthesiology in National Taiwan University Hospital for their valuable comments in helping the study.
References
| 1 |
Weiler N, Latorre F, Eberle B, Goedecke R, Heinrichs W.
Respiratory mechanics, gastric insufflation pressure, and air leakage of the laryngeal mask airway.
Anesth Analg 1997;84:1025–1028.
|
| 2 |
Hockings L, Heaney M, Chambers NA, Erb TO, von Ungern-Sternberg BS.
Reduced air leakage by adjusting the cuff pressure in pediatric laryngeal mask airways during spontaneous ventilation.
Paediatr Anaesth 2010;20:313–317.
|
| 3 |
Devitt JH, Wenstone R, Noel AG, O’Donnel MP.
The laryngeal mask airway and positive-pressure ventilation.
Anesthesiology 1994;80:550–555.
|
| 4 |
Shariffuddin II, Wang CY.
Randomised crossover comparison of the Ambu AuraOnce Laryngeal Mask with the LMA Classic laryngeal mask airway in paralysed anaesthetised patients.
Anaesthesia 2008;63:82–85.
|
| 5 |
Baidya DK, Chandralekha, Darlong V, Pandey R, Maitra S, Khanna P.
Comparative efficacy and safety of the Ambu® AuraOnceTM laryngeal mask airway during general anaesthesia in adults: a systematic review and meta-analysis.
Anaesthesia 2014;69:1023–1032.
|
| 6 |
Levitan RM, Kinkle WC.
Initial anatomic investigations of the I-gel airway: a novel supraglottic airway without inflatable cuff.
Anaesthesia 2005;60:1022–1026.
|
| 7 |
Russo SG, Cremer S, Galli T, et al.
Randomized comparison of the i-gelTM, the LMA SupremeTM, and the Laryngeal Tube Suction-D using clinical and fibreoptic assessments in elective patients.
BMC Anesthesiol 2012;7:18.
|
| 8 |
Park SH, Han SH, Do SH, Kim JW, Kim JH.
The influence of head and neck position on the oropharyngeal leak pressure and cuff position of three supraglottic airway devices.
Anesth Analg 2009;108:112–117.
|
| 9 |
Buckham M, Brooker M, Brimacombe J, Keller C.
A comparison of the reinforced and standard laryngeal mask airway: ease of insertion and the influence of head and neck position on oropharyngeal leak pressure and intracuff pressure.
Anaesth Intensive Care 1999;27:628–631.
|
| 10 |
Brimacombe J, Keller C.
Stability of the LMA-ProSeal and standard laryngeal mask airway in different head and neck positions: a randomized crossover study.
Eur J Anaesthesiol 2003;20:65–69.
|
| 11 |
Okuda K, Inagawa G, Miwa T, Hiroki K.
Influence of head and neck position on cuff position and oropharyngeal sealing pressure with the laryngeal mask airway in children.
Br J Anaesth 2001;86:122–124.
|
| 12 |
Sanuki T, Uda R, Sugioka S, et al.
The influence of head and neck position on ventilation with the i-gel airway in paralysed, anaesthetised patients.
Eur J Anaesthesiol 2011;28:597–599.
|
| 13 |
Maino P, Dullenkopf A, Bernet V, Weiss M.
Nitrous oxide diffusion into the cuffs of disposable laryngeal mask airways.
Anaesthesia 2005;60:278–282.
|
| 14 |
Egan B, Eng RL.
Laryngeal mask airway.
In: Chu L, Fuller A, eds. Manual of Clinical Anesthesiology. 1st ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2011:174.
|
| 15 |
Erdfelder E, Faul F, Buchner A.
GPOWER: a general power analysis program.
Behav Res Methods 1996;28:1-11.
|
| 16 |
Norkin CC, White DJ.
The cervical spine.
In: Norkin CC, White DJ, eds. Measurement of Joint Motion: A Guide to Goniometry. 4th ed. Philadelphia, PA: F.A. Davis Company; 2009:351.
|
| 17 |
Kannaujia A, Srivastava U, Saraswat N, Mishra A, Kumar A, Saxena S.
A preliminary study of I-gel: a new supraglottic airway device.
Indian J Anaesth 2009;53:52–56.
|
| 18 |
Kleine-Brueggeney M, Theiler L, Urwyler N, Vogt A, Greif R.
Randomized trial comparing the i-gelTM and Magill tracheal tube with the single-use ILMATM and ILMATM tracheal tube for fibreoptic-guided intubation in anaesthetized patients with a predicted difficult airway.
Br J Anaesth 2011;107:251–257.
|
| 19 |
Vaida SJ, Yodfat UA.
Angulation of the airway tube in the AMBU laryngeal mask could be responsible for improved insertion success.
Anesth Analg 2006;103:264.
|
| 20 |
Sood J.
Laryngeal mask airway and its variants.
Indian J Anaesth 2005;49:275–280.
|
| 21 |
Sudhir G, Redfern D, Hall JE, Wilkes AR, Cann C.
A comparison of the disposable Ambu AuraOnce Laryngeal Mask with the reusable LMA Classic laryngeal mask airway.
Anaesthesia 2007;62:719–722.
|
| 22 |
Hagberg CA, Jensen, FS, Genzwuerker HV, et al.
A multicenter study of the Ambu® Laryngeal Mask in nonparalyzed, anesthetized patients.
Anesth Analg 2005;101:1862–1866.
|